Endoscopy
Editor-In-Chief: C. Michael Gibson, M.S., M.D. [1]
Overview
Endoscopy means looking inside and typically refers to looking inside the human body for medical reasons using an instrument called an endoscope. Endoscopy can also refer to using a borescope in technical situations where direct line-of-sight observation is not feasible.
Overview
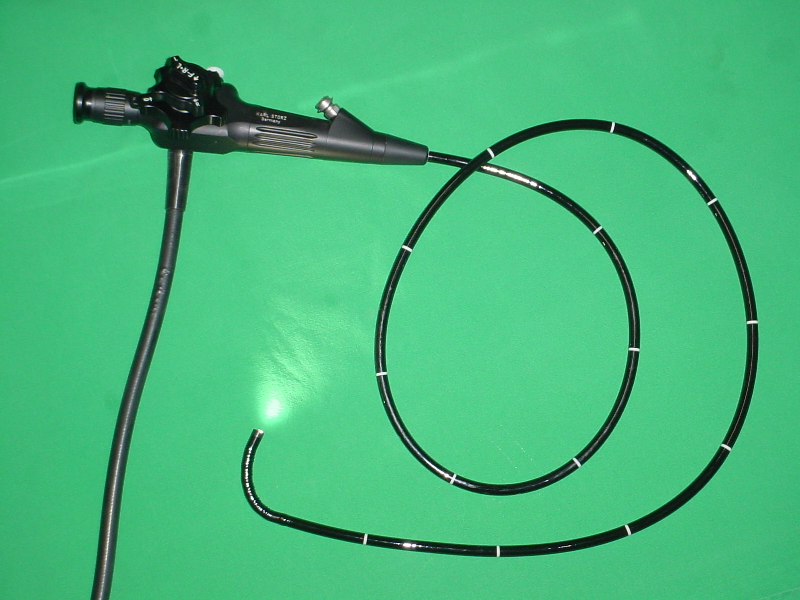
Endoscopy is a minimally invasive diagnostic medical procedure that is used to assess the interior surfaces of an organ by inserting a tube into the body. The instrument may have a rigid or flexible tube and not only provide an image for visual inspection and photography, but also enable taking biopsies and retrieval of foreign objects. Endoscopy is the vehicle for minimally invasive surgery.
Many endoscopic procedures are considered to be relatively painless and, at worst, associated with mild discomfort. Most patients tolerate the procedure with only topical anaesthesia of the oropharynx using lignocaine spray (Source: Esophagogastroduodenoscopy, Wikipedia). Complications are rare (only 5% of all operations) but can include perforation of the organ under inspection with the endoscope or biopsy instrument. If that occurs open surgery may be required to repair the injury.
Components
An endoscope can consist of
- a rigid or flexible tube
- a light delivery system to illuminate the organ or object under inspection. The light source is normally outside the body and the light is typically directed via an optical fiber system
- a lens system transmitting the image to the viewer from the fiberscope
- an additional channel to allow entry of medical instruments or manipulators
Uses
Endoscopy can involve
- The gastrointestinal tract (GI tract):
- oesophagus, stomach and duodenum (esophagogastroduodenoscopy)
- small intestine
- colon (colonoscopy,proctosigmoidoscopy)
- Bile duct
- endoscopic retrograde cholangiopancreatography (ERCP), duodenoscope-assisted cholangiopancreatoscopy, intraoperative cholangioscopy
- The respiratory tract
- The nose (rhinoscopy)
- The lower respiratory tract (bronchoscopy)
- The urinary tract (cystoscopy)
- The female reproductive system
- The cervix (colposcopy)
- The uterus (hysteroscopy)
- The Fallopian tubes (Falloscopy)
- Normally closed body cavities (through a small incision):
- The abdominal or pelvic cavity (laparoscopy)
- The interior of a joint (arthroscopy)
- Organs of the chest (thoracoscopy and mediastinoscopy)
- During pregnancy
- The amnion (amnioscopy)
- The fetus (fetoscopy)
- Plastic Surgery
- Panendoscopy (or triple endoscopy)
- Combines laryngoscopy, esophagoscopy, and bronchoscopy
- Non-medical uses for endoscopy
- The planning and architectural community have found the endoscope useful for pre-visualization of scale models of proposed buildings and cities (architectural endoscopy)
- Internal inspection of complex technical systems (borescope)
- Endoscopes are also a tool helpful in the examination of improvised explosive devices by bomb disposal personnel.
- The FBI uses endoscopes for conducting surveillance via tight spaces.
History
The first endoscope, of a kind, was developed in 1806 by Philip Bozzini with his introduction of a "Lichtleiter" (light conductor) "for the examinations of the canals and cavities of the human body". However, the Vienna Medical Society disapproved of such curiosity. An endoscope was first introduced into a human in 1822 by William Beaumont, an army surgeon at Mackinac Island, Michigan. The use of electric light was a major step in the improvement of endoscopy. The first such lights were external. Later, smaller bulbs became available making internal light possible, for instance in a hysteroscope by Charles David in 1908. Hans Christian Jacobaeus has been given credit for early endoscopic explorations of the abdomen and the thorax with laparoscopy (1912) and thoracoscopy (1910). Laparoscopy was used in the diagnosis of liver and gallbladder disease by Heinz Kalk in the 1930s. Hope reported in 1937 on the use of laparoscopy to diagnose ectopic pregnancy. In 1944, Raoul Palmer placed his patients in the Trendelenburg position after gaseous distention of the abdomen and thus was able to reliably perform gynecologic laparoscopy.
The first gastrocamera was released in 1950 by Olympus Optical Co., Ltd. The device took pictures on monochromatic film using a small light bulb that was triggered manually. The device was of limited use, however, because it did not implement real-time optical capability. Olympus continued its development of endoscopes by incorporating fiber optics in the early 1960s, leading to the first useful endoscopes. In 1964, it released a gastrocamera guided by a fiberscope.[2] A few articles claim that Dr.Basil Hirschowitz of Univ.Of Michigan,Ann Arbor discussed the endoscope in early 50's.[3]
As endoscopic technology improved, so did the methods of gastrointestinal endoscopy. Owing primarily to the efforts of Dr. Hiromi Shinya in the late 1960s, GI endoscopy developed into what is more recognizable as today's colonoscopy. While many doctors experimented with techniques to take advantage of the new iterations of endoscopes, Dr. Shinya focused on techniques that would allow for successful operation of the endoscope by an individual, rejecting the common practice at the time of utilizing two people. Consequently, many of the fundamental methods and procedures of modern colonoscopy were developed by Dr. Shinya.
Dr. Shinya's other great contribution was to therapeutic endoscopy, in his invention of the electrosurgical polypectomy snare with the aid of Olympus employee Hiroshi Ichikawa. Shinya sketched his first plans for the device on January 8, 1969. He envisioned a loop of wire attached to the end of a colonoscope that would allow for easy removal of polyps during investigation by passing a current through the wire. By September of 1969, the first polypectomy using this device was performed. Polypectomy has since become the most common therapeutic procedure performed with an endoscope. Template:Wikiref
By 1980, laparoscopy training was required by gynecologists to perform tubal ligation procedures and diagnostic evaluations of the pelvis. The first laparoscopic cholecystectomy was performed in 1984 and the first video-laparoscopic cholecystectomy in 1987. During the 1990s, laparoscopic surgery was extended to the appendix, spleen, colon, stomach, kidney, and liver. Wireless capsule endoscopy or Capsule Endoscopy is now approved in all the countries including Japan where government reimbusement will be available from Oct.2007.Capsule Endoscopy [4] increases detection of Small Bowel tumors where traditional Endoscopy is not very efficient.
Risks
- Infection
- Punctured organs
- Allergic reactions due to Contrast agents or dyes (such as those used in a CT scan)
- Over-sedation
- Unnecessary and overuse[1][2]
After The Endoscopy
After the procedure the patient will be observed and monitored by a qualified individual in the endoscopy or a recovery area until a significant portion of the medication has worn off. Occasionally a patient is left with a mild sore throat, which promptly responds to saline gargles, or a feeling of distention from the insufflated air that was used during the procedure. Both problems are mild and fleeting. When fully recovered, the patient will be instructed when to resume his/her usual diet (probably within a few hours) and will be allowed to be taken home. Because of the use of sedation, most facilities mandate that the patient is taken home by another person and not to drive on his/her own or handle machinery for the remainder of the day.
Recent developments
With the application of robotic systems, telesurgery was introduced as the surgeon could operate from a site physically removed from the patient. The first transatlantic surgery has been called the Lindbergh Operation.
See also
- angiography
- fiberscope
- robotic surgery
- SmartKart Endoscopic system cart
References
- Siegler AM, Kemmann E: Hysteroscopy. Obstet Gynecol Survey 30:567-88, 1975.
- Armin Gärtner; medical technics and information technologie, Band II. Medizintechnik und Informationstechnologie, Band II. ISBN 3-8249-0941-3.
- Obituary: Professor Harold Hopkins, FRS, The Times, 3 Nov 1994.
- Template:Wikicite
External links
- Site Containing Videos and Information about Endoscopy
- Diagnostic and Therapeutic Endoscopy - Open-Access Journal
- DAVE Project, Digital Atlas of Video Education - Gastroenterology
- Global Rating Scale, GRS - Quality Assurance for Endoscopy
- Endoscope Repair Parts
cs:Endoskopický nástroj
de:Endoskop
eo:Endoskopio
eu:Endoskopia
he:אנדוסקופיה
it:Endoscopia
nl:Endoscopie
ps:اېنډوسکوپي
fi:Tähystys
sv:Endoskopi
Template:WH
Template:WS
Template:Jb1
- ↑ Shaheen NJ, Fennerty MB, Bergman JJ (2018). "Less Is More: A Minimalist Approach to Endoscopy". Gastroenterology. 154 (7): 1993–2003. doi:10.1053/j.gastro.2017.12.044. PMID 29454789.
- ↑ Heisser T, Peng L, Weigl K, Hoffmeister M, Brenner H (2019). "Outcomes at follow-up of negative colonoscopy in average risk population: systematic review and meta-analysis". BMJ. 367: l6109. doi:10.1136/bmj.l6109. PMC 6853024 Check
|pmc=value (help). PMID 31722884.