Chelation therapy
Editor-In-Chief: C. Michael Gibson, M.S., M.D. [3], Gervasio Lamas, M.D.
To read more about chelation therapy for cardiovascular disease click here.
Overview
Chelation therapy is the administration of chelating agents to remove heavy metals from the body. Chelation therapy has a long history of use in clinical toxicology. For the most common forms of heavy metal intoxication – lead, arsenic, or mercury – a number of chelating agents are available. The US Food and Drug Administration (FDA) only approves the use of calcium-disodium EDTA and DMSA, and not penicillamine and succimer, in the management of adult patients with lead poisoning. Dimercaptosuccinic acid (DMSA) has been recommended for the treatment of lead poisoning in children by poison centers around the world.[1] Other chelating agents, such as 2,3-dimercapto-1-propanesulfonic acid (DMPS) and alpha lipoic acid (ALA), are used in conventional and alternative medicine. The use of chelation as alternative therapy can prove fatal, particularly when disodium EDTA is confused for calcium EDTA and pushed rapidly intravenously in children. Death due to hypocalcemia may occur.[2] Until recently, medical evidence did not support the effectiveness of chelation therapy for any other purpose than the treatment of heavy metal poisoning. Although there is randomized trials evidence that EDTA-based infusions decrease cardiovascular events in patients with prior heart attack,[3] particularly in patients with diabetes,[4] these indications are not currently recognized by the U.S. Food and Drug Administration (FDA). The FDA also considers over-the-counter (OTC) chelation products to be "unapproved".
Discovery and History in Medicine
Chelating agents were introduced into medicine as a result of the use of poison gas in World War I. The first widely used chelating agent—the organic dithiol compound dimercaprol, also named British Anti-Lewisite or BAL—was used as an antidote to the arsenic-based poison gas, Lewisite. The sulphur atoms in BAL's mercaptan groups strongly bond to the arsenic in Lewisite, forming a water-soluble compound that entered the bloodstream, allowing it to be removed from the body by the kidneys and liver. BAL had severe side-effects.
After World War II, a large number of navy personnel suffered from lead poisoning as a result of their jobs repainting the hulls of ships. The medical use of EDTA as a lead chelating agent was introduced. Unlike BAL, it is a synthetic amino acid and contains no mercaptans. While EDTA had some uncomfortable side effects, they were not as severe as BAL.
In the 1960s, BAL was modified into DMSA, a related dithiol with far fewer side effects. DMSA quickly replaced both BAL and EDTA, becoming the US standard of care for the treatment of lead, arsenic, and mercury poisoning, which it remains today. EDTA chelation is approved by the U.S. Food and Drug Administration (FDA) for treating lead poisoning and heavy metal toxicity.
Research in the former Soviet Union led to the introduction of DMPS, another dithiol, as a mercury-chelating agent. The Soviets also introduced ALA, which is transformed by the body into the dithiol dihydrolipoic acid, a mercury- and arsenic-chelating agent. DMPS has experimental status in the US FDA, while ALA is a common nutritional supplement.
Since the 1970s, iron chelation therapy has been used as an alternative to regular phlebotomy to treat excess iron stores in people with haemochromatosis.[5]
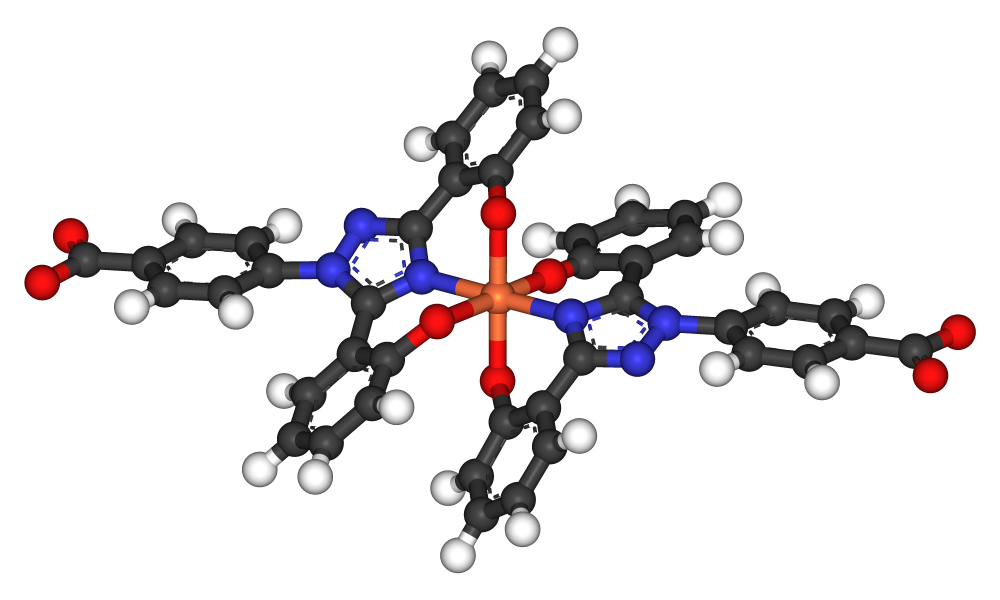
Other chelating agents have been discovered. They all function by making several chemical bonds with metal ions, thus rendering them much less chemically reactive. The resulting complex is water-soluble, allowing it to enter the bloodstream and be excreted harmlessly.
Disodium EDTA was first used in 1956 to treat coronary disease, and has remained controversial to date.[6][7] Its use has been restricted primarily to alternative medicine chelation practitioners. In 1998, the U.S. Federal Trade Commission (FTC) pursued the American College for Advancement in Medicine (ACAM), an organization that promotes "complementary, alternative and integrative medicine" over the claims made regarding the treatment of atherosclerosis in advertisements for EDTA chelation therapy. The FTC concluded that there was a lack of scientific studies to support these claims and that the statements by the ACAM were false. In 1999, the ACAM agreed to stop presenting chelation therapy as effective in treating heart disease, avoiding legal proceedings. In 2010 the U.S. Food and Drug Administration (FDA) warned companies who sold over-the-counter (OTC) chelation products and stated that such "products are unapproved drugs and devices and that it is a violation of federal law to make unproven claims about these products. There are no FDA-approved OTC chelation products."
Interestingly, in 2001, in the midst of the unresolved controversy on EDTA chelation therapy use by alternative medicine practitioners, the National Center for Complementary and Alternative Medicine and the National Heart, Lung, and Blood Institute released an RFA (RFA 01-004, April 2001) for a definitive trial of chelation therapy for patients with atherosclerotic coronary disease – not metal intoxication. The grant was ultimately awarded in 2002 (U01 HL92607 from the NHLBI and NCCAM), the results are available in detail.[3][4]
Approved Medical Use
Chelation therapy is used as a treatment for acute mercury, iron (including in cases of thalassemia), arsenic, lead, uranium, plutonium and other forms of toxic metal poisoning. The chelating agent may be administered intravenously, intramuscularly, or orally, depending on the agent and the type of poisoning.
Several chelating agents are available, having different affinities for different metals. Shown below is a table summarizing the common chelating agents and their clinical use.
| Chelating agents | Clinical use |
| Dimercaprol (British anti-Lewisite; BAL) | - Arsenic poisoning - Mercury poisoning - Lead poisoning (in addition to EDTA) - Lewisite poisoning (for which it was developed as an antidote) |
| Dimercaptosuccinic acid (DMSA) | - Lead poisoning - Arsenic poisoning - Mercury poisoning |
| Dimercapto-propane sulfonate (DMPS) | - Severe arsenic poisoning - Severe mercury poisoning |
| D-penicillamine | Mainly in: - Copper toxicity Occasionally adjunctive therapy in: - Gold toxicity - Arsenic poisoning - Lead poisoning - Rheumatoid arthritis |
| Ethylenediamine tetraacetic acid (calcium disodium versante) (CaNa2-EDTA) | - Lead poisoning |
| Deferoxamine and defarasirox | - Acute iron poisoning - Iron overload |
Medically Diagnosed Heavy Metal Poisoning
Some common chelating agents are EDTA (ethylenediaminetetraacetic acid), DMPS (2,3-dimercaptopropanesulfonic acid), TTFD (thiamine tetrahydrofurfuryl disulfide), and DMSA (2,3-dimercaptosuccinic acid). Calcium-disodium EDTA and DMSA are only approved for the removal of lead by the Food and Drug Administration while DMPS and TTFD are not approved by the FDA. These drugs bind to heavy metals in the body and prevent them from binding to other agents. They are then excreted from the body. The chelating process also removes vital nutrients such as vitamins C and E, therefore these must be supplemented.
Children with severe lead poisoning, as manifested by blood lead level of 70 µg/dL or higher or by the presence of encephalopathy, should be administered a combination of dimercaprol and CaNa2 EDTA.[8] Chelation therapy with CaNa2 EDTA and dimercaprol is indicated for adults with blood lead level higher than 100 µg/dL and symptomatic patients with blood lead level higher than 50 µg/dL. Chelation therapy can be considered for asymptomatic adults with blood lead level ranging from 80 to 99 100 µg/dL.[9]
Unapproved Use in Alternative Medicine
Alternative medicine uses chelation therapy as a non-standard treatment for some ailments, including heart disease and autism.[10][11] In 2010 the U.S. Food and Drug Administration (FDA) warned companies who sold over-the-counter (OTC) chelation products and stated that such "products are unapproved drugs and devices and that it is a violation of federal law to make unproven claims about these products. There are no FDA-approved OTC chelation products." Attempts have been made to use it in treating kidney dysfunction, calcific band keratopathy (an eye disorder), ovarian cancer, and atherosclerotic coronary and peripheral arterial disease.
Cancer
The American Cancer Society says of chelation therapy: "Available scientific evidence does not support claims that it is effective for treating other conditions such as cancer. Chelation therapy can be toxic and has the potential to cause kidney damage, irregular heartbeat, and even death."
Heart Disease
Until recently, the use of EDTA chelation therapy as a treatment for coronary artery disease had not been shown to be effective and is still not approved by the U.S. Food and Drug Administration (FDA).[12] Several possible mechanisms have been proposed, though none has been scientifically validated. The American Heart Association stated that there is "no scientific evidence to demonstrate any benefit from this form of therapy" and that the "United States Food and Drug Administration (FDA), the National Institutes of Health (NIH) and the American College of Cardiology all agreed with the American Heart Association" that "there have been no adequate, controlled, published scientific studies using currently approved scientific methodology to support this therapy for cardiovascular disease."[12] Like other scientific commentators, they note that any improvement among heart patients undergoing chelation therapy can be attributed to the placebo effect and lifestyle changes discovered in conventional medicine but recommended by chelationists; "quitting smoking, losing weight, eating more fruits and vegetables, avoiding foods high in saturated fats and exercising regularly". They note their concern that patients could put off proven treatments for heart disease like drugs or surgery. A 2005 systematic review found that controlled scientific studies did not support chelation therapy for heart disease. It found that very small trials and uncontrolled descriptive studies have reported benefits while larger controlled studies have found results no better than placebo.[13] In 2009, the Montana Board of Medical Examiners issued a position paper concluding that "chelation therapy has no proven efficacy in the treatment of cardiovascular disease, and in some patients could be injurious."[14]
However, in the face statements by professional associations and self-appointed anti-chelationists that EDTA chelation was ineffective and possibly dangerous, patients continued to seek, and practitioners to administer this therapy. Therefore, in 2001, the National Center for Complementary and Alternative Medicine and the National Heart, Lung, and Blood Institute released an RFA (RFA 01-004, April 2001) for a definitive trial of chelation therapy for patients with atherosclerotic coronary disease – not metal intoxication. The grant was ultimately awarded in 2002 (U01 HL92607 from the NHLBIand NCCAM) (Trial to Assess Chelation Therapy (TACT)) and started enrolling in 2003.[15] NCCAM Director Stephen E. Straus cited the "widespread use of chelation therapy in lieu of established therapies, the lack of adequate prior research to verify its safety and effectiveness, and the overall impact of coronary artery disease" as factors motivating the trial.[16] The American College for Advancement in Medicine, the leading organization of chelation practitioners, created to promote chelation therapy, played a part in the adoption of the TACT clinical trial, which led to further criticism of the trial.[17] Atwood et al. argued that methodological flaws and lack of prior probability make this trial "unethical, dangerous, pointless, and wasteful."[17] However, an OHRP investigation of the trial, instigated by self-appointed anti-chelation individuals, closed after the TACT study team, including NIH scientists, answered all questions and made satisfactory changes.[18]
Moreover, the assertions that the trial was unnecessary due to abundant existing data was wrong. A 2002 analysis by Cochrane reported that there were not enough data to reach a conclusion for or against chelation therapy.[19] “Cochrane Authors' conclusions: At present, there is insufficient evidence to decide on the effectiveness or ineffectiveness of chelation therapy in improving clinical outcomes of people with atherosclerotic cardiovascular disease. This decision must be preceded by conducting randomized controlled trials that would include endpoints that show the effects of chelation therapy on longevity and quality of life among people with atherosclerotic cardiovascular disease.”
The principal results of TACT were published in the Journal of the American Medical Association in 2013, and in Circulation: Cardiovascular Quality and Outcomes in 2014. There was a statistically significant 18% reduction in combined cardiovascular events with disodium EDTA-based chelation infusions, and a 41% reduction in patients with diabetes. Whether EDTA chelation will become a standard treatment for patients with coronary disease will likely depend on future studies. Safety analyses showed that the treatment, as applied within the clinical trial, was safe.
To read more about chelation therapy for cardiovascular disease click here.
Autism
Based on the speculation that heavy metal poisoning may trigger the symptoms of autism, some parents have turned to alternative medicine practitioners who provide chelation therapy. However, the only evidence to support this belief is anecdotal. There is strong epidemiological evidence that refutes links between environmental triggers, in particular thimerosal-containing vaccines and the onset of autistic symptoms. No scientific data supports the claim that the mercury in the vaccine preservative thiomersal causes autism[20] or its symptoms,[21] and there is no scientific support for chelation therapy as a treatment for autism.[22][23]
The hypothesis of mercury poisoning as a cause for autism was proposed by Bernard, Enayati, Roger, Binstock, and Redwood in 2002[24]. These authors stated that symptoms of autism arise from exposure to mercury. They further state that symptoms of autism tend to emerge when children are administered vaccines, the rise in children with autism in the 1990’s coincided with the introduction of two mercury-containing immunizations, and finally, patients with autism have been found to have levels of mercury in their systems[25]. An important problem with this theory is the fact that the symptoms of autism do not perfectly resemble symptoms of mercury poisoning. Though mercury poisoning can cause impaired social interactions, communication problems, and stereotypic behaviors[26], as seen in autism, it also causes “ataxia, constricted visual fields, peripheral neuropathy, hypertension, skin eruption, and thrombocytopenia”[27] - symptoms not seen in children with autism. Thimerosal, the mercury-containing preservative found in vaccines, has been removed from nearly all childhood immunizations. In one state study, however, the Caifornia Department of Developmental Services found that the prevalence of autism increased from January 1995 to March 2007, concluding that exposure to thimerosal does not lead to autism[28]. Nevertheless, caregivers of children with autism have sought out treatment to rid mercury and other heavy metals from the body, in a process known as chelation.
Chelation therapy was used by the British after World War II to remove arsenic, lead, and other metals created by the during the war due to lack of materials. Patients’ conditions improved as these metals were removed from their bodies[29]. Today, chelation therapy is used to rid the body of toxic metals such as lead and mercury. Doctors should take a blood test to assess current kidney and liver function, nutrient status, and blood-lipid levels before chelation therapy begins[30]. A gluten-free, casein-free (GFCF) diet and supplemental changes, including shots of vitamin B12, may be used. Treatment may be applied to the skin via a transdermal patch[31]. Another treatment is administered intravenously, a process that takes 2-3 hours, costs about $100 per treatment, and 20-30 treatments are often required[32].
Some common chelating agents are EDTA (ethylenediaminetetraacetic acid), DMSA (sodium 2,3 dimercaptopropane-1 sulfate), TTFD (thiamine tetrahydrofurfuryl disulfide), and DMPS (2,3 dimercaptosuccinic acid). EDTA and DMSA are only approved for the removal of lead by the Food and Drug Administration while DMPS and TTFD are not approved by the FDA. These drugs bind to heavy metals in the body and prevent them from binding to other agents. They are then excreted from the body. The chelating process also removes vital nutrients such as vitamins C and E, therefore these must be supplemented[33].
Some parents of children with autism have reported significant gains in their children’s symptoms following chelation therapy. They contend that within weeks of the initial treatment, their children have made drastic improvements in behavior and social engagement. Younger children have reportedly made faster and more significant results[34]. However, other parents have stated that chelation therapies made no difference in their children’s developmental outcomes[35].
There are significant risks associated with the use of chelation for the treatments of autism. The deaths of two children were reported due to hypocalemia and cardiac arrest after receiving chelation therapy[36]. Long-term use of the chelating agent SMSA can cause liver damage, zinc deficiency, and bone marrow suppression[37]. Mineral deficiencies, cardiovascular effects (blood pressure drop), kidney problems, and the possibility of distributing mercury throughout the body may also occur. However, using a combination of chelators, supplements, diet changes, and regular lab tests can reportedly reduce the risk of side effects[38].
Because of the lack of empirical support in controlled studies and the possibility of dangerous side effects, chelation therapy for the treatment of autism is not recommended. The most effective known interventions for children with autism are educational and behavioral therapies.
Controversy
The efficacy, safety, and much of the theory behind these alternative practices are disputed by the medical community. In 2001, researchers at the University of Calgary reported that cardiac patients receiving chelation therapy fared no better than those who received placebo treatment.[39]
In 1998, the U.S. Federal Trade Commission (FTC) charged that the web site of the American College for Advancement in Medicine (ACAM) and a brochure they published had made false or unsubstantiated claims. In December 1998, the FTC announced that it had secured a consent agreement barring ACAM from making unsubstantiated advertising claims that chelation therapy is effective against atherosclerosis or any other disease of the circulatory system.[40][41]
The use of chelation therapy by alternative medicine practitioners for behavioural and other disorders is considered pseudoscientific; there is no proof that it is effective, and it can be fatal.
Prevalence
The American College for Advancement in Medicine (ACAM), a not-for-profit 501(c)(6) organization which promotes chelation therapy, claims that 800,000 patient visits for chelation therapy, with an average of 40 visits per patient, were made in the United States in 1997.[42]
Side Effects and Safety Concerns
As approved pharmaceuticals, the various chelating agents may cause specific side effects if used improperly. When protocols are followed, there is a low occurrence of side effects. DMPS injections may cause skin reactions at the injection site. Other side effects reported include fever, headache, nausea. No death has been linked to DMPS. The EDTAs when used according to protocol are equally safe. Most important is the correct use and a slow infusion time (1 g/h or less of NaEDTA). CaEDTA may be infused more rapidly as there is less concern with hypocalcemia. Side effects are largely avoided if general medical caution is exercised. Most importantly, renal function has to be checked before any chelation substance is used. The German Environmental Agency (Umweltbundesamt) listed DMSA along with DMPS as the two most useful and safe chelating agents available at this time. Chelation treatment is the preferred medical treatment for reducing toxic effects of metals.[43]
Chelation therapy can be hazardous when used inappropriately. In August 2005, intravenous disodium EDTA was used instead of calcium EDTA, and infused rapidly, causing the death of a 5-year-old boy with autism;[17] a 3-year-old nonautistic girl died in February 2005, and a nonautistic adult died in August 2003. These deaths were due to cardiac arrest caused by hypocalcemia during chelation therapy. In two of the cases hypocalcemia appears to have been caused by the administration of Na2EDTA (Disodium EDTA) and in the third case the type of EDTA was unknown.[44][45] Only the 3-year-old girl had been medically assessed and found to have an elevated blood lead level and resulting low iron levels and anemia, a proper medical cause for chelation therapy to be conducted. According to protocol, EDTA should not be used in the treatment of children. More than 30 deaths have been recorded in association with IV-administered disodium EDTA since the 1970s, although millions have used these treatments.[17]
References
- ↑ Chisolm JJ (2000). "Safety and efficacy of meso-2,3-dimercaptosuccinic acid (DMSA) in children with elevated blood lead concentrations". J Toxicol Clin Toxicol. 38 (4): 365–75. PMID 10930052.
- ↑ Morbidity and mortality weekly report, CDC.gov
- ↑ 3.0 3.1 Lamas GA, Goertz C, Boineau R, Mark DB, Rozema T, Nahin RL; et al. (2013). "Effect of disodium EDTA chelation regimen on cardiovascular events in patients with previous myocardial infarction: the TACT randomized trial". JAMA. 309 (12): 1241–50. doi:10.1001/jama.2013.2107. PMID 23532240.
- ↑ 4.0 4.1 Escolar E, Lamas GA, Mark DB, Boineau R, Goertz C, Rosenberg Y; et al. (2014). "The Effect of an EDTA-based Chelation Regimen on Patients With Diabetes Mellitus and Prior Myocardial Infarction in the Trial to Assess Chelation Therapy (TACT)". Circ Cardiovasc Qual Outcomes. 7 (1): 15–24. doi:10.1161/CIRCOUTCOMES.113.000663. PMID 24254885.
- ↑ "Hemochromatosis: Monitoring and Treatment". National Center on Birth Defects and Developmental Disabilities (NCBDDD). 2007-11-01. Retrieved 2008-03-29.
- ↑ CLARKE NE, CLARKE CN, MOSHER RE (1955). "The in vivo dissolution of metastatic calcium; an approach to atherosclerosis". Am J Med Sci. 229 (2): 142–9. PMID 13228424.
- ↑ CLARKE CN, CLARKE NE, MOSHER RE (1956). "Treatment of angina pectoris with disodium ethylene diamine tetraacetic acid". Am J Med Sci. 232 (6): 654–66. PMID 13372537.
- ↑ Chisolm JJ (1968). "The use of chelating agents in the treatment of acute and chronic lead intoxication in childhood". J Pediatr. 73 (1): 1–38. PMID 4969284.
- ↑ Kosnett MJ, Wedeen RP, Rothenberg SJ, Hipkins KL, Materna BL, Schwartz BS; et al. (2007). "Recommendations for medical management of adult lead exposure". Environ Health Perspect. 115 (3): 463–71. doi:10.1289/ehp.9784. PMC 1849937. PMID 17431500.
- ↑ Ernst E (2000). "Chelation therapy for coronary heart disease: An overview of all clinical investigations". Am Heart J. 140 (1): 139–41. doi:10.1067/mhj.2000.107548. PMID 10874275.
- ↑ Weber W, Newmark S (2007). "Complementary and alternative medical therapies for attention-deficit/hyperactivity disorder and autism". Pediatr Clin North Am. 54 (6): 983–1006, xii. doi:10.1016/j.pcl.2007.09.006. PMID 18061787.
- ↑ 12.0 12.1 Ernst E (1997). "Chelation therapy for peripheral arterial occlusive disease: a systematic review". Circulation. 96 (3): 1031–3. PMID 9264515.
- ↑ Seely DM, Wu P, Mills EJ (2005). "EDTA chelation therapy for cardiovascular disease: a systematic review". BMC Cardiovasc Disord. 5: 32. doi:10.1186/1471-2261-5-32. PMC 1282574. PMID 16262904.
- ↑ Montana Board of Medical Examiners (BME) (14 May 2009). "EDTA Chelation for Cardiovascular Disease" (BME Position Paper). Business Standard Div., Montana Dept. of Labor and Industry. Archived from the original on 2010-02-04.[1]
- ↑ Lamas GA, Goertz C, Boineau R, Mark DB, Rozema T, Nahin RL; et al. (2012). "Design of the Trial to Assess Chelation Therapy (TACT)". Am Heart J. 163 (1): 7–12. doi:10.1016/j.ahj.2011.10.002. PMC 3243954. PMID 22172430.
- ↑ National Institutes of Health (NIH); National Center for Complementary and Alternative Medicine; National Heart, Lung, and Blood Institute (7 August 2002). "NIH Launches Large Clinical Trial on EDTA Chelation Therapy for Coronary Artery Disease". NIH News (Press release). (NIH).[2]
- ↑ 17.0 17.1 17.2 17.3 Atwood KC, Woeckner E, Baratz RS, Sampson WI (2008). "Why the NIH Trial to Assess Chelation Therapy (TACT) should be abandoned". Medscape J Med. 10 (5): 115. PMC 2438277. PMID 18596934.
- ↑ Bauchner H, Fontanarosa PB, Golub RM (2013). "Evaluation of the Trial to Assess Chelation Therapy (TACT): the scientific process, peer review, and editorial scrutiny". JAMA. 309 (12): 1291–2. doi:10.1001/jama.2013.2761. PMID 23532245.
- ↑ Villarruz MV, Dans A, Tan F (2002). "Chelation therapy for atherosclerotic cardiovascular disease". Cochrane Database Syst Rev (4): CD002785. doi:10.1002/14651858.CD002785. PMID 12519577.
- ↑ Doja A, Roberts W (2006). "Immunizations and autism: a review of the literature". Can J Neurol Sci. 33 (4): 341–6. PMID 17168158.
- ↑ Thompson WW, Price C, Goodson B; et al. (2007). "Early thimerosal exposure and neuropsychological outcomes at 7 to 10 years". N Engl J Med. 357 (13): 1281–92. doi:10.1056/NEJMoa071434. PMID 17898097.
- ↑ Weber W, Newmark S (2007). "Complementary and alternative medical therapies for attention-deficit/hyperactivity disorder and autism". Pediatr Clin North Am. 54 (6): 983–1006. doi:10.1016/j.pcl.2007.09.006. PMID 18061787.
- ↑ Blakeslee, Sandra (2004-05-19). "Panel Finds No Evidence To Tie Autism To Vaccines". New York Times. Retrieved 2008-02-01. "An examination of scientific studies worldwide has found no convincing evidence that vaccines cause autism, according to a committee of experts appointed by the Institute of Medicine."
- ↑ Bernard, S., Enayati, A., Roger, T., Binstock, T., & Redwood, L. (2002). The role of mercury in the pathogenesis of autism. Molecular Psychiatry, 7, S42-S43.
- ↑ Bernard, S., Enayati, A., Roger, T., Binstock, T., & Redwood, L. (2002). The role of mercury in the pathogenesis of autism. Molecular Psychiatry , 7, S42-S43.
- ↑ Bernard, S., Enayati, A., Roger, T., Binstock, T., & Redwood, L. (2002). The role of mercury in the pathogenesis of autism. Molecular Psychiatry , 7, S42-S43.
- ↑ Ng, D. K.-K., Chan, C.-H., Soo, M.-T., & Lee, R. S.-Y. (2007). Low-level chronic mercury exposure in children and adolescents: meta-analysis. Pediatrics International , 49, 80-87.
- ↑ Schechter, R., & Grether, J. K. (2008). Continuing increases in autism reported to California's developmental services system. Archives of General Psychiatry , 65 (1), 19-24.
- ↑ Nash, R. A. (2005). Metals in medicine. Alternative Therapies in Health and Medicine , 11 (4), 18-25.
- ↑ Klotter, J. (2006). Chelation for autism. Townsend Letter: The Examiner of Alternative Medicine , 30, p. 273.
- ↑ Bridges, S. (2006). The promise of chelation. Mothering , 54-61.
- ↑ Klotter, J. (2006). Chelation for autism. Townsend Letter: The Examiner of Alternative Medicine , 30, p. 273.
- ↑ Bridges, S. (2006). The promise of chelation. Mothering , 54-61.
- ↑ Bridges, S. (2006). The promise of chelation. Mothering , 54-61.
- ↑ Laidler, J. R. (n.d.). Through the looking glass: my involvment with autism quackery. Retrieved May 26, 2008, from Autism Watch: http://www.autism-watch.org/about/bio2.shtml
- ↑ Schechtman, M. A. (2007). Scientifically unsupported therapies in the treatment of young children with autism spectrum disorders. Psychiatric Annals , 37 (9), 639-645.
- ↑ Klotter, J. (2006). Chelation for autism. Townsend Letter: The Examiner of Alternative Medicine , 30, p. 273.
- ↑ Bridges, S. (2006). The promise of chelation. Mothering , 54-61.
- ↑ Knudtson ML, Wyse DG, Galbraith PD; et al. (2002). "Chelation therapy for ischemic heart disease: a randomized controlled trial". JAMA. 287 (4): 481–6. doi:10.1001/jama.287.4.481. PMID 11798370.
- ↑ "American College for Advancement in Medicine, File No. 962 3147, Docket No. C-3882". Federal Trade Commission. Retrieved 2007-11-11.
- ↑ "Medical Association Settles False Advertising Charges Over Promotion of 'Chelation Therapy'". Quackwatch. December 8, 1998. Retrieved 2007-11-11. Check date values in:
|date=(help) - ↑ "Physician Group Backs New NIH Chelation Therapy Study For Heart Disease" (Press release). American College for Advancement in Medicine. August 14, 2002. Retrieved 2007-11-11. Check date values in:
|date=(help) - ↑ Flora SJ (2011). "Arsenic-induced oxidative stress and its reversibility". Free Radic Biol Med. 51 (2): 257–81. doi:10.1016/j.freeradbiomed.2011.04.008. PMID 21554949.
- ↑ Brown MJ, Willis T, Omalu B, Leiker R (2006). "Deaths resulting from hypocalcemia after administration of edetate disodium: 2003-2005". Pediatrics. 118 (2): e534–6. doi:10.1542/peds.2006-0858. PMID 16882789.
- ↑ Baxter AJ, Krenzelok EP (2008). "Pediatric fatality secondary to EDTA chelation". Clin Toxicol (Phila). 46 (10): 1083–4. doi:10.1080/15563650701261488. PMID 18949650.