HIV AIDS pathophysiology
| https://https://www.youtube.com/watch?v=5g1ijpBI6Dk%7C350}} |
|
AIDS Microchapters |
|
Diagnosis |
|
Treatment |
|
Case Studies |
|
HIV AIDS pathophysiology On the Web |
|
American Roentgen Ray Society Images of HIV AIDS pathophysiology |
|
Risk calculators and risk factors for HIV AIDS pathophysiology |
Editor-In-Chief: C. Michael Gibson, M.S., M.D. [1]; Associate Editor(s)-in-Chief: Ammu Susheela, M.D. [2], Jesus Rosario Hernandez, M.D. [3]
Overview
HIV causes acquired immunodeficiency syndrome by depleting CD4+ T helper lymphocytes. The virus is acquired by either sexual contact, exposure to contaminated blood, or mother-to-child transmission. Once the virus is acquired, it disseminates to the majority of lymphoid organs, where it enters a period of rapid viral replication. This leads to the acute phase of the infection, which is characterized by a very elevated viral titer and an acute drop in CD4 T-lymphocyte count. As the immune response mounts, viral replication and the CD4-cell depletion rate drops. The immune system continues to deteriorate, but at a slower pace. This is known as the chronic phase of HIV infection. The HIV virus causes CD4-cell death by a variety of mechanisms including cytopathic single-cell destruction, syncytia formation, autoimmunity, and superantigen formation.[1]
Pathophysiology
HIV transmission
| Exposure Route | Estimated infections per 10,000 exposures to an infected source |
|---|---|
| Blood Transfusion | 9,000[3] |
| Childbirth | 2,500[4] |
| Needle-sharing injection drug use | 67[5] |
| Receptive anal intercourse¶ | 50[6][7] |
| Percutaneous needle stick | 30[8] |
| Receptive penile-vaginal intercourse¶ | 10[6][7][9] |
| Insertive anal intercourse¶ | 6.5[6][7] |
| Insertive penile-vaginal intercourse¶ | 5[6][7] |
| Receptive fellatio¶ | 1[7] |
| Insertive fellatio¶ | 0.5[7] |
| ¶ Assuming no condom use. | |
Since the beginning of the pandemic, three main transmission routes for HIV have been identified: sexual route, blood or blood product route, and mother-to-child transmission.
Sexual route
- The majority of HIV infections are acquired through unprotected sexual relations. Sexual transmission can occur when infected sexual secretions of one partner come into contact with the genital, oral, or rectal mucous membranes of another.
Blood or blood product route
- This transmission route can account for infections in intravenous drug users, hemophiliacs and recipients of blood transfusions (though most transfusions are checked for HIV in the developed world) and blood products.
- It is also of concern for persons receiving medical care in regions where there is prevalent substandard hygiene in the use of injection equipment, such as the reuse of needles in Third World countries. HIV can also be spread through the sharing of needles.
- Health care workers such as nurses, laboratory workers, and doctors, have also been infected, although this occurs more rarely. People who give and receive tattoos, piercings, and scarification procedures can also be at risk of infection.
Mother-to-child transmission (MTCT)
- The transmission of the virus from the mother to the child can occur in utero during pregnancy and intrapartum at childbirth. In the absence of treatment, the transmission rate between the mother and child is around 25%.[4] However, where combination antiretroviral drug treatment and Cesarian section are available, this risk can be reduced to as low as 1%.[4] Breast feeding also presents a risk of infection for the baby.
- HIV-2 is transmitted much less frequently by the MTCT and sexual route than HIV-1.
Other Considerations
- HIV has been found at low concentrations in the saliva, tears and urine of infected individuals, but there are no recorded cases of infection by these secretions and the potential risk of transmission is negligible.[10]
- The use of physical barriers such as the latex condom is widely advocated to reduce the sexual transmission of HIV. Spermicide, when used alone or with vaginal contraceptives like a diaphragm, actually increases the male to female transmission rate due to inflammation of the vagina; it should not be considered a barrier to infection.[11]
- A panel of experts convened by WHO and the UNAIDS Secretariat has "recommended that male circumcision now be recognized as an additional important intervention to reduce the risk of heterosexually acquired HIV infection in men."[12]
- Research is clarifying whether there is a historical relationship between rates of male circumcision and rates of HIV in differing social and cultural contexts. Previously, Siegfried et al. suggested that it was possible that the correlation between circumcision and HIV in observational studies may be due to confounding factors, and remarked that the randomized controlled trials would therefore provide "essential evidence" about the effects of circumcision.[13]
- There is little data on circumcision's effect on HIV risk with homosexual men and it is still being studied. A study of foreign and American men by scientists at the University of Washington, Seattle concluded: "Uncircumcised homosexual men in Seattle had a two fold increased risk of HIV infection.
- If the relative risk that we observed in Seattle were also present in other populations, the population attributable risk of uncircumcised status for HIV in homosexual men would be 40%, i.e., 40% of homosexual transmission of HIV could be potentially preventable with universal circumcision."[4]
- A study of Australian men headed by David Templeton, MD, from the University of New South Wales found "no relationship at all between circumcision and HIV seroconversion in" homosexual men. Templeton theorizes that this may be because most HIV occurs "following receptive rather than insertive intercourse," as he finds data on circumcision's effect on heterosexual men "compelling".[14] South African medical experts are concerned that the repeated use of unsterilized blades in the ritual (not medical) circumcision of adolescent boys may be spreading HIV.[15]
Viral Pathogenesis
After the virus is acquired, a period of rapid viral replication ensues, leading to abundant viremia. During primary infection, the level of HIV may reach several million virus particles per milliliter of blood.[16] This response is accompanied by a marked drop in the numbers of circulating CD4+ T cells. This acute viremia is associated in virtually all people with the activation of CD8+ T cells, which kill HIV-infected cells, and subsequently with antibody production, or seroconversion. The CD8+ T cell response is thought to be important in controlling virus levels, which peak and then decline, as the CD4+ T cell counts rebound. A good CD8+ T cell response has been linked to slower disease progression and a better prognosis, though it does not eliminate the virus.[17]
The pathophysiology of AIDS is complex. Ultimately, HIV causes AIDS by depleting CD4+ T helper lymphocytes. This weakens the immune system and allows opportunistic infections. T lymphocytes are essential to the immune response for defense against opportunistic infections and the inhibition of neoplastic proliferation. The mechanism of CD4+T cell depletion differs in the acute and chronic phases.[18] During the acute phase, HIV-induced cell lysis and killing of infected cells by cytotoxic T cells accounts for CD4+ T cell depletion, although apoptosis may also be a factor. During the chronic phase, the consequences of generalized immune activation coupled with the gradual loss of the ability of the immune system to generate new T cells appear to account for the slow decline in CD4+ T cell numbers. Although the symptoms of immune deficiency characteristic of AIDS do not appear for years after a person is infected, the bulk of CD4+ T cell loss occurs during the first weeks of infection, especially in the intestinal mucosa, which harbors the majority of the lymphocytes found in the body.[19] The reason for the preferential loss of mucosal CD4+ T cells is that a majority of mucosal CD4+ T cells express the CCR5 coreceptor, whereas a small fraction of CD4+ T cells in the bloodstream do so.[20] HIV seeks out and destroys CCR5 expressing CD4+ cells during acute infection. A vigorous immune response eventually controls the infection and initiates the clinically latent phase. However, CD4+ T cells in mucosal tissues remain depleted throughout the infection, although enough remain to initially ward off life-threatening infections.
Continuous HIV replication results in a state of generalized immune activation persisting throughout the chronic phase.[21] Immune activation, which is reflected by the increased activation state of immune cells and release of proinflammatory cytokines, results from the activity of several HIV gene products and the immune response to ongoing HIV replication. Another cause is the breakdown of the immune surveillance system of the mucosal barrier caused by the depletion of mucosal CD4+ T cells during the acute phase of disease.[22]
This results in the systemic exposure of the immune system to microbial components of the gut’s normal flora, which in a healthy person is kept in check by the mucosal immune system. The activation and proliferation of T cells that results from immune activation provides fresh targets for HIV infection. However, direct killing by HIV alone cannot account for the observed depletion of CD4+ T cells since only 0.01–0.10% of CD4+ T cells in the blood are infected.
Major Mechanisms of Disease
HIV causes major immune compromise by directly altering CD4 T-cell number and function. Some of the potential mechanisms by which the virus affects these cells include:[1]
- HIV-mediated cell destruction
Single-cell killing is secondary to the direct cytopathic effects of the virus. It results from the inhibition of protein synthesis or from the accumulation of viral DNA.
- HIV-mediated syncytia formation
Syncytia are created by the fusion of multiple cells to create giant multinucleated cells. HIV is capable of inducing syncytia formation particularly in the accelerated phase of the disease. This allows infection of new cells while evading immune control.
- HIV-mediated autoimmunity
Both HLA-DR and HLA-DQ, two important HLA paralogues that are partly homologous in structure to gp120 and gp41 proteins of HIV type. Antibodies to these proteins may cross-react with the host MHC class II molecules.
- Anergy due to inappropriate cell signaling through gp120-CD4 interaction
Antigen-antibody complexes of gp120 are capable, in vitro, of inducing anergy in CD4 T-cells. These complexes bind the CD4 molecules making these cells refractory to further antigenic stimulation by CD3 activation.
- Superantigen-mediated disturbance of T-cell subgroups
Unlike regular antigens that bind the MHCII groove, superantigens bind to a specific variable region of the β chain of the T-cell receptor (TCR) and lead to massive stimulation of T-cells. HIV may encode superantigens that cause T-cell activation rendering these cells more susceptible to infection. [1]
 |
HIV-specific Immune Response
Although the HIV-specific immune response is important to control viral replication and spread initially, it plays an important role in the immunopathogenesis in the chronic phase of the disease. The immune response against HIV aims to eliminate HIV-infected cells further accelerating the progressive deterioration of the immune system.[1]
Role of GALT in Pathogenesis
- Port of entry for HIV infection is mostly through direct blood inoculation or exposure through genital mucosal surface. The gastrointestinal tract contains a large amount of lymphoid tissue, making it an ideal place for replication of Human Immunodeficiency Virus. GALT plays a role in HIV replication. [23]
- GALT has been found to have the following characteristics:
- Site of early viral seeding.
- Establishment of the pro-viral reservoir.
- The proviral GALT reservoir contributes to the following:
- Difficulty in controlling the infection.
- Difficulty in reducing the level of HIV provirus through sustained ART.[24] Various studies measuring the CD44 in GALT, have shown the relatively less reconstitution with ART, than that observed in peripheral blood.[25][26]
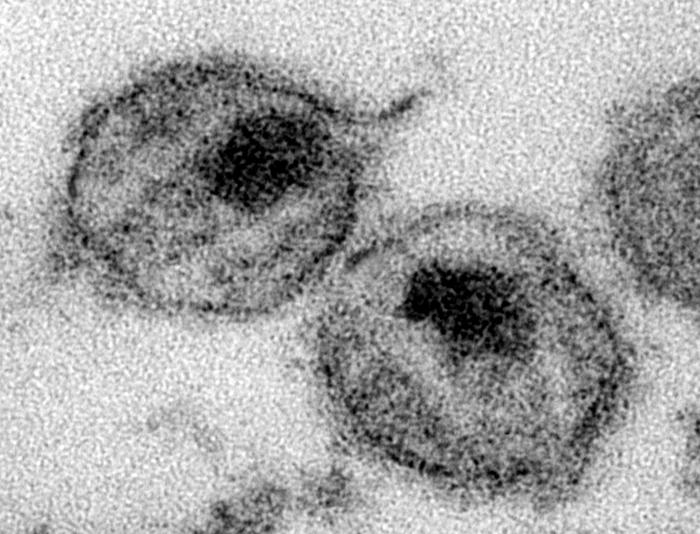
Gallery
-
HIV structure. From Public Health Image Library (PHIL). [27]
-
HIV pathophysiology. From Public Health Image Library (PHIL). [27]
References
- ↑ 1.0 1.1 1.2 1.3 Pantaleo G, Graziosi C, Fauci AS (1993). "New concepts in the immunopathogenesis of human immunodeficiency virus infection". N Engl J Med. 328 (5): 327–35. doi:10.1056/NEJM199302043280508. PMID 8093551.
- ↑ Smith, D. K., Grohskopf, L. A., Black, R. J., Auerbach, J. D., Veronese, F., Struble, K. A., Cheever, L., Johnson, M., Paxton, L. A., Onorato, I. A. and Greenberg, A. E. (2005). "Antiretroviral Postexposure Prophylaxis After Sexual, Injection-Drug Use, or Other Nonoccupational Exposure to HIV in the United States". MMWR. 54 (RR02): 1–20.
- ↑ Donegan, E., Stuart, M., Niland, J. C., Sacks, H. S., Azen, S. P., Dietrich, S. L., Faucett, C., Fletcher, M. A., Kleinman, S. H., Operskalski, E. A.; et al. (1990). "Infection with human immunodeficiency virus type 1 (HIV-1) among recipients of antibody-positive blood donations". Ann. Intern. Med. 113 (10): 733–739. PMID 2240875.
- ↑ 4.0 4.1 4.2 Coovadia, H. (2004). "Antiretroviral agents—how best to protect infants from HIV and save their mothers from AIDS". N. Engl. J. Med. 351 (3): 289–292. PMID 15247337.
- ↑ Kaplan, E. H. and Heimer, R. (1995). "HIV incidence among New Haven needle exchange participants: updated estimates from syringe tracking and testing data". J. Acquir. Immune Defic. Syndr. Hum. Retrovirol. 10 (2): 175–176. PMID 7552482.
- ↑ 6.0 6.1 6.2 6.3 European Study Group on Heterosexual Transmission of HIV (1992). "Comparison of female to male and male to female transmission of HIV in 563 stable couples". BMJ. 304 (6830): 809–813. PMID 1392708.
- ↑ 7.0 7.1 7.2 7.3 7.4 7.5 Varghese, B., Maher, J. E., Peterman, T. A., Branson, B. M. and Steketee, R. W. (2002). "Reducing the risk of sexual HIV transmission: quantifying the per-act risk for HIV on the basis of choice of partner, sex act, and condom use". Sex. Transm. Dis. 29 (1): 38–43. PMID 11773877.
- ↑ Bell, D. M. (1997). "Occupational risk of human immunodeficiency virus infection in healthcare workers: an overview". Am. J. Med. 102 (5B): 9–15. PMID 9845490.
- ↑ Leynaert, B., Downs, A. M. and de Vincenzi, I. (1998). "Heterosexual transmission of human immunodeficiency virus: variability of infectivity throughout the course of infection. European Study Group on Heterosexual Transmission of HIV". Am. J. Epidemiol. 148 (1): 88–96. PMID 9663408.
- ↑ Lifson AR (1988). "Do alternate modes for transmission of human immunodeficiency virus exist? A review". JAMA. 259 (9): 1353–6. PMID 2963151.
- ↑ "Should spermicides be used with condoms?". Condom Brochure, FDA OSHI HIV STDs. Retrieved 2006-10-23.
- ↑ WHO (2007). "WHO and UNAIDS announce recommendations from expert consultation on male circumcision for HIV prevention". WHO.int. Retrieved 2007-07-13.
- ↑ Siegfried, N., Muller, M., Deeks, J., Volmink, J., Egger, M., Low, N., Walker, S. and Williamson, P. (2005). "HIV and male circumcision--a systematic review with assessment of the quality of studies". Lancet Infect. Dis. 5 (3): 165–173. PMID 15766651.
- ↑ http://www.medscape.com/viewarticle/560823
- ↑ Various (2005). "Repeated Use of Unsterilized Blades in Ritual Circumcision Might Contribute to HIV Spread in S. Africa, Doctors Say". Kaisernetwork.org. Retrieved 2006-03-28.
- ↑ Piatak, M., Jr, Saag, M. S., Yang, L. C., Clark, S. J., Kappes, J. C., Luk, K. C., Hahn, B. H., Shaw, G. M. and Lifson, J.D. (1993). "High levels of HIV-1 in plasma during all stages of infection determined by competitive PCR". Science. 259 (5102): 1749–1754. Bibcode:1993Sci...259.1749P. doi:10.1126/science.8096089. PMID 8096089.
- ↑ Pantaleo G, Demarest JF, Schacker T, Vaccarezza M, Cohen OJ, Daucher M, Graziosi C, Schnittman SS, Quinn TC, Shaw GM, Perrin L, Tambussi G, Lazzarin A, Sekaly RP, Soudeyns H, Corey L, Fauci AS. (1997). "The qualitative nature of the primary immune response to HIV infection is a prognosticator of disease progression independent of the initial level of plasma viremia". Proc Natl Acad Sci U S A. 94 (1): 254–258. Bibcode:1997PNAS...94..254P. doi:10.1073/pnas.94.1.254. PMC 19306. PMID 8990195.
- ↑ Hel Z, McGhee JR, Mestecky J (June 2006). "HIV infection: first battle decides the war". Trends Immunol. 27 (6): 274–81. doi:10.1016/j.it.2006.04.007. PMID 16679064.
- ↑ Mehandru S, Poles MA, Tenner-Racz K, Horowitz A, Hurley A, Hogan C, Boden D, Racz P, Markowitz M (September 2004). "Primary HIV-1 infection is associated with preferential depletion of CD4+ T lymphocytes from effector sites in the gastrointestinal tract". J. Exp. Med. 200 (6): 761–70. doi:10.1084/jem.20041196. PMC 2211967. PMID 15365095.
- ↑ Brenchley JM, Schacker TW, Ruff LE, Price DA, Taylor JH, Beilman GJ, Nguyen PL, Khoruts A, Larson M, Haase AT, Douek DC (September 2004). "CD4+ T cell depletion during all stages of HIV disease occurs predominantly in the gastrointestinal tract". J. Exp. Med. 200 (6): 749–59. doi:10.1084/jem.20040874. PMC 2211962. PMID 15365096.
- ↑ Appay V, Sauce D (January 2008). "Immune activation and inflammation in HIV-1 infection: causes and consequences". J. Pathol. 214 (2): 231–41. doi:10.1002/path.2276. PMID 18161758.
- ↑ Brenchley JM, Price DA, Schacker TW, Asher TE, Silvestri G, Rao S, Kazzaz Z, Bornstein E, Lambotte O, Altmann D, Blazar BR, Rodriguez B, Teixeira-Johnson L, Landay A, Martin JN, Hecht FM, Picker LJ, Lederman MM, Deeks SG, Douek DC (December 2006). "Microbial translocation is a cause of systemic immune activation in chronic HIV infection". Nat. Med. 12 (12): 1365–71. doi:10.1038/nm1511. PMID 17115046.
- ↑ Talal AH, Irwin CE, Dieterich DT, Yee H, Zhang L (2001). "Effect of HIV-1 infection on lymphocyte proliferation in gut-associated lymphoid tissue". J. Acquir. Immune Defic. Syndr. 26 (3): 208–17. PMID 11242193. Retrieved 2012-05-25. Unknown parameter
|month=ignored (help) - ↑ Poles MA, Boscardin WJ, Elliott J, Taing P, Fuerst MM, McGowan I, Brown S, Anton PA (2006). "Lack of decay of HIV-1 in gut-associated lymphoid tissue reservoirs in maximally suppressed individuals". J. Acquir. Immune Defic. Syndr. 43 (1): 65–8. doi:10.1097/01.qai.0000230524.71717.14. PMID 16936559. Retrieved 2012-05-25. Unknown parameter
|month=ignored (help) - ↑ Guadalupe M, Reay E, Sankaran S, Prindiville T, Flamm J, McNeil A, Dandekar S (2003). "Severe CD4+ T-cell depletion in gut lymphoid tissue during primary human immunodeficiency virus type 1 infection and substantial delay in restoration following highly active antiretroviral therapy". J. Virol. 77 (21): 11708–17. PMC 229357. PMID 14557656. Retrieved 2012-05-25. Unknown parameter
|month=ignored (help) - ↑ Shacklett BL, Cox CA, Sandberg JK, Stollman NH, Jacobson MA, Nixon DF (2003). "Trafficking of human immunodeficiency virus type 1-specific CD8+ T cells to gut-associated lymphoid tissue during chronic infection". J. Virol. 77 (10): 5621–31. PMC 154016. PMID 12719554. Retrieved 2012-05-25. Unknown parameter
|month=ignored (help) - ↑ 27.0 27.1 "Public Health Image Library (PHIL)".
- CS1 maint: Multiple names: authors list
- CS1 maint: Explicit use of et al.
- Pages with citations using unsupported parameters
- HIV/AIDS
- Disease
- Immune system disorders
- Viral diseases
- Pandemics
- Sexually transmitted infections
- Syndromes
- Virology
- AIDS origin hypotheses
- Medical disasters
- Immunodeficiency
- Microbiology
- Emergency mdicine
- Up-To-Date
- Infectious disease
![HIV structure. From Public Health Image Library (PHIL). [27]](/images/1/13/HIV_structure01.jpeg)
![HIV pathophysiology. From Public Health Image Library (PHIL). [27]](/images/2/20/HIV_pathophysiology01.jpeg)