Acromioclavicular separation
| Acromioclavicular separation | |
 | |
|---|---|
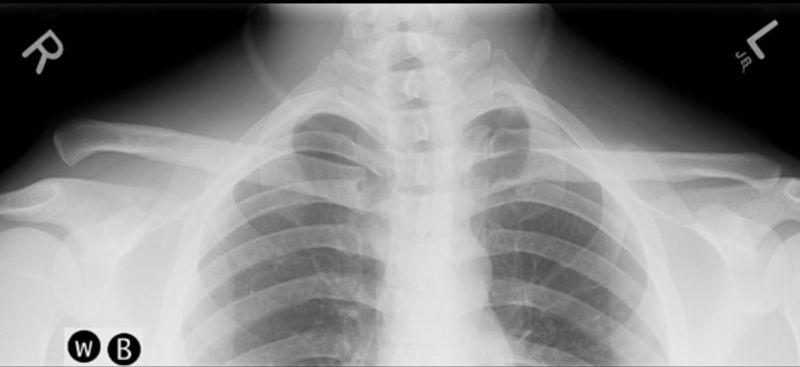
| A Separated Shoulder XRay modified to easily show bones. Notice the separation between the end of the collarbone and the scapula. | |
| ICD-10 | S43.1 |
| ICD-9 | 831.04, 831.14 |
| eMedicine | orthoped/462 |
Editor-In-Chief: C. Michael Gibson, M.S., M.D. [1]
A separated shoulder, otherwise known as an acromioclavicular separation or AC separation, is a common injury to the acromioclavicular joint. This is not the same as a shoulder dislocation as that involves a dislocation of the Glenohumeral joint
Overview
Separated shoulders often occur in people who participate in sports such as American football, soccer, horseback riding, hockey, mountain biking, biking, roller derby, rowing, and rugby. The dislocation is classified into 6 types, with 1 through 3 increasing in severity, and 4 through 6 being the most severe. The most common mechanism of injury is a fall on the tip of the shoulder or also a fall on an outstretched hand (FOOSH). In falls where the force is transmitted indirectly, often only the acromioclavular ligament is affected, and the coracoclavicular ligaments remain unharmed.[1] In hockey, the separation is sometimes due to a lateral force, as when one gets forcefully checked into the side of the rink. [2]
Types
Type I
A Type I AC separation involves trauma to the ligaments that form the joint, but no severe tearing or fracture. It is commonly referred to as a sprain. Most doctors treat this type of dislocation with anti-inflammatory drugs, pain medication and the placement of the arm in a sling or an immobilizer.
Type II
A Type II AC separation involves complete tearing of the acromioclavicular ligament, as well as a sprain or partial tear of the coracoclavicular ligaments. This often causes a noticeable bump on the shoulder. By pressing on the sternal aspect of the clavicle you force the acromial end down, and by releasing, watch it pop back up (eliciting a piano key sign due to the tearing of the AC ligament)[3]. Severe pain and loss of movement are common. Treatment is typically an arm sling, bedrest, ice and heat therapy, and anti-inflammatory drugs. Most people recover full motion of the shoulder and arm within 6 to 8 weeks, often with the assistance of physical therapy.
Type III
In a Type III AC separation both acromioclavicular and coracoclavicular ligaments are torn. A significant bump is formed by the lateral end of the clavicle. This bump is permanent. The clavicle can be moved in and out of place on the shoulder. It may take 12 weeks to heal, and physical therapy can be beneficial. It may take even longer for the shoulder strength to approach feeling normal. The injured shoulder may not be able to take the abuse that it could previously, but for most purposes it will be quite usable and sufficient. However, there still is controversy as to whether or not surgery may be necessary for optimal shoulder use in sport.
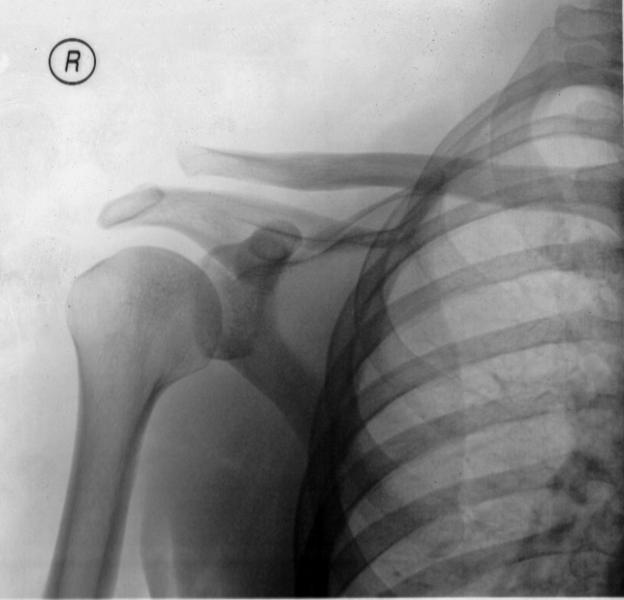
Radiograph demonstrating a right type 3 acromioclavicular separation
Type IV
This is a type III injury with avulsion of the coracoclavicular ligament from the clavicle, with the distal clavicle displaced posteriorly into or through the trapezius. This injury is generally acknowledged to require surgery.
Type V
This is type III but with exaggeration of the vertical displacement of the clavicle from the scapula. This injury generally requires surgery.
Type VI
This is type III with inferior dislocation of the lateral end of the clavicle below the coracoid. It is extremely rare and generally only involved with motor vehicle collisions. This requires surgery.
Current treatment options
Non-surgical
Most non-surgical treatment options include physical therapy to build up the muscles around the joint, helping stabilize the joint. Literature regarding long-term follow-up after surgical repair of type III injuries is scarce, and those treated nonoperatively generally do quite well. [4] Many studies [5] [6] [7] [8] [9] have come to the conclusion that non-surgical treatment is as good or better than surgical treatment, or that anything attained because of surgery is quite limited.[9] It appears that after a while, the body "remodels" the joint, either expanding the distal clavicle or causing it to atrophy. [10] One study suggests that quarterbacks with type III injuries on their dominant side may possibly do better with surgery. [11] There may also be the potential that surgical repair may be less painful in the long run.[9]
Surgical
Type 2 separations have always been treated non-surgically, initially. However, the risks of arthritis with type 2 separations are greatly increased. If this becomes severe, the Mumford procedure or distal clavicle excision can be performed.
There have been many surgeries described to fix complete acromioclavicular separations, including recently arthroscopic. There is no consensus on which surgery is best. Several surgeries have been described with pins or hooks. Another surgery performs muscle transfer.
A common surgery is some form of Modified Weaver-Dunn procedure, which involves cutting off the end of the clavicle portion, partially sacrificing the coracoacromial ligament and suturing the displaced acromial end to the lateral aspect of the clavicle for stabilization, then often some form of additional support is introduced to replace the coracoclavicular ligament(s). Variations of this support includes grafting of tendons from the leg [12] or the use of synthetic sutures or suture anchors[13] . Other surgeries have used a Rockwood screw that is inserted initially and then removed after 12 weeks. Physical therapy is always recommended after surgery, and most patients get flexibility back, although possibly somewhat limited.
References
- ↑ Gloria M. Beim, MD (2000 Jul–Sep). "Acromioclavicular Joint Injuries". J Athl Train. 35 (3): 261–267. Retrieved 2006-11-24. Check date values in:
|date=(help) - ↑ Stephen Bushee, ATC. "Acromioclavicular Separation in Ice Hockey, Typical injury...different mechanism!". Retrieved 2006-11-01.
- ↑ http://www.hope.edu/academic/kinesiology/athtrain/program/studentprojects/Ldornbos2/shoulder/sld060.htm
- ↑ Template:Cite website
- ↑ Bjerneld H. Hovelius L. Thorling J. (October 1983). "Acromio-clavicular separations treated conservatively. A 5-year follow-up study". Acta Orthopaedica Scandinavica. 54 (5): 743–745.
- ↑ Taft TN. Wilson FC. Oglesby JW. (September 1987). "Dislocation of the acromioclavicular joint. An end-result study". Journal of Bone & Joint Surgery - American Volume. 69 (7): 1045–51.
- ↑ Template:Cite paper
- ↑ Larsen E. Bjerg-Nielsen A. Christensen P. (1986 Apr.). "Conservative or surgical treatment of acromioclavicular dislocation. Aprospective, controlled, randomized study". Journal of Bone & Joint Surgery - American Volume. 68 (4): 552–5. Check date values in:
|date=(help) - ↑ 9.0 9.1 9.2 Press J, Zuckerman JD, Gallagher M, Cuomo F. (1997). "Treatment of grade III acromioclavicular separations. Operative versus nonoperative management". Bull Hosp Jt Dis. 56 (2): 77–83.
- ↑ M. L. RAWES, J. J. DIAS (1996). "LONG-TERM RESULTS OF CONSERVATIVE TREATMENT FOR ACROMIOCLAVICULAR DISLOCATION" (PDF). J Bone Joint Surg (Br). 78 (B): 410–2.
- ↑ Schlegel TF, Boublik M, Hawkins RJ. Grade III acromioclavicular separations in NFL quarterbacks. Program and abstracts of the American Orthopaedic Society of Sports Medicine Annual Meeting; July 14-17, 2005; Keystone, Colorado.
- ↑ Template:Cite website
- ↑ Breslow MJ, Jazrawi LM, Bernstein AD, Kummer FJ, Rokito AS. (2002). "Treatment of acromioclavicular joint separation: suture or suture anchors?". J Shoulder Elbow Surg. 11 (3Template:Unicode): 225–9.
See also
External links
- Overview and diagram
- Wheelessonline (very Confusing) online orthopedic resource
- Stone Clinic: Acromioclavicular Joint Reconstruction Using Gore-Tex Tape (Now using allograft tendon)
- Arthroscopic Weaver-Dunn
- Injuries of the acromioclavicular joint and current treatment options (Free full text pdf available)
- Acromioclavicular Injuries: New Management Options Emerge (free with registration)
- Complete Dislocations of the Acromioclavicular Joint Chapter 17 of a Military book on orthopedic treatment during World War II.
Forums
Template:Dislocations, sprains and strains Template:WH Template:WS