HIV AIDS cost-effectiveness of therapy
|
AIDS Microchapters |
|
Diagnosis |
|
Treatment |
|
Case Studies |
|
HIV AIDS cost-effectiveness of therapy On the Web |
|
American Roentgen Ray Society Images of HIV AIDS cost-effectiveness of therapy |
|
Risk calculators and risk factors for HIV AIDS cost-effectiveness of therapy |
Editor-In-Chief: C. Michael Gibson, M.S., M.D. [1]; Associate Editors-in-Chief: Ujjwal Rastogi, MBBS ; Alejandro Lemor, M.D. [2] ; Ammu Susheela, M.D. [3]
Overview
HIV and AIDS retard economic growth by destroying human capital. Without proper nutrition, health care and medicine that is available in developed countries, large numbers of people are falling victim to AIDS. They will not only be unable to work, but will also require significant medical care. The forecast is that this will likely cause a collapse of economies and societies in the region. In some heavily infected areas, the epidemic has left behind many orphans cared for by elderly grandparents.[1]
Cost-Effectiveness of Therapy
Cost of HIV Treatment
- Treatment accounts for the majority of cost of HIV AIDS.
- It mostly depends on the health car utilization by HIV patients.
- The costs associated with health care utilization in each disease stage are summed across all disease stages from infection to death.
- The average annual cost of HIV care in the ART era was estimated to be $19,912 (in 2006 dollars; $23,000 in 2010 dollars[2]
- The most recent published estimate of lifetime HIV treatment costs was $367,134 (in 2009 dollars; $379,668 in 2010 dollars).[3]
Cost of HIV Testing
Testing in Non-Health Care Settings
- Non-health care settings, such as jails/prisons, community-based organizations (CBOs), and outreach venues, are also common places to implement HIV testing programs.
- The cost per new HIV diagnosis associated with CBO-sponsored activities ranged from $10,334 to $20,413 (2010 dollars).[4][5]
- Variance in the cost per new HIV diagnosis was more pronounced when evaluating HIV testing programs in jails (from $2,946 per new diagnosis in Florida jails to $30,392 in Wisconsin jails indicting difference in implementation cost.
Testing in Health Care Setting
- Several US-based studies have evaluated the cost-effectiveness of routine opt-out HIV screening in clinical settings.
- These settings included emergency departments, primary care settings, urgent care centers, and STD clinics.
- The cost per new diagnosis ranged from $1,900 to $10,000 (in 2010 dollars), and varied by setting and testing implementation strategy[6][7]
HIV Survival
- The use of highly active antiretroviral therapy (HAART) since 1996 has significantly improved survival for persons infected with HIV. Schackman et al. estimated life expectancy from the time of infection to be 32.1 years from a large dataset of persons in routine outpatient care in the current treatment era.
- Using US national HIV surveillance data, another study estimated that average life expectancy after an HIV diagnosis increased from 10.5 to 22.5 years from 1996 to 2005[8]
Annual Cost of HIV by State
- The states with highest number of new diagnoses in 2009, and thus the greatest financial burden, were Florida, California, New York, and Texas. In all, the total lifetime treatment cost for HIV based on new diagnoses in 2009 was estimated to be $16.6 billion.
|
| ||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
Impact on Other Countries
- The increased mortality in this Southern African countries will result in a smaller skilled population and labor force.[1] This smaller labor force will be predominantly young people, with reduced knowledge and work experience leading to reduced productivity.
- An increase in workers’ time off to look after sick family members or for sick leave will also lower productivity.
- Increased mortality will also weaken the mechanisms that generate human capital and investment in people, through loss of income and the death of parents.[1]
- AIDS seriously weakens the taxable population, reducing the resources available for public expenditures such as education and health services not related to AIDS resulting in increasing pressure for the state's finances and slower growth of the economy.
- This results in a slower growth of the tax base, an effect that will be reinforced if there are growing expenditures on treating the sick, training (to replace sick workers), sick pay and caring for AIDS orphans.
- On the level of the household, AIDS results in both the loss of income and increased spending on healthcare by the household.
- The income effects of this lead to spending reduction as well as a substitution effect away from education and towards healthcare and funeral spending.
- A study in Côte d'Ivoire showed that households with an HIV/AIDS patient spent twice as much on medical expenses as other households.[11]
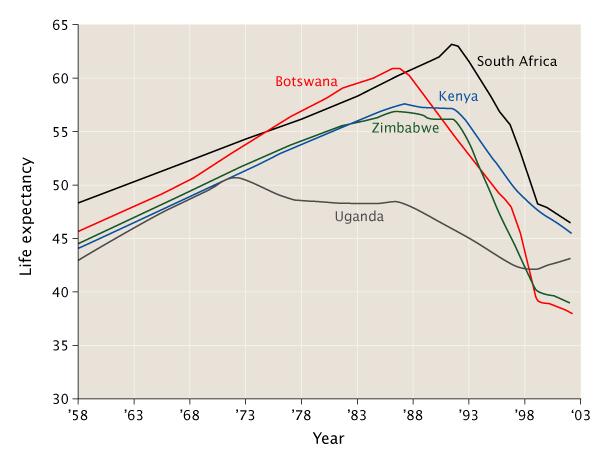
- UNAIDS, WHO and the United Nations Development Program have documented a correlation between the decreasing life expectancy and the lowering of gross national product in many African countries with prevalence rates of 10% or more.
- Since 1992, predictions that AIDS would slow economic growth in these countries have been published. The degree of impact depended on assumptions about the extent to which illness would be funded by savings and who would be infected.[11]
- Conclusions reached from models of the growth trajectories of 30 sub-Saharan economies over the period 1990–2025 were that the economic growth rates of these countries would be between 0.56 and 1.47% lower.
- The impact on gross domestic product (GDP) per capita was less conclusive. However, in 2000, the rate of growth of Africa's per capita GDP was in fact reduced by 0.7% per year from 1990–1997 with a further 0.3% per year lower in countries also affected by malaria.[12]
- The forecast now is that the growth of GDP for these countries will undergo a further reduction of between 0.5 and 2.6% per annum.[1] However, these estimates may be an underestimate, as they do not look at the effects on output per capita.[13]
- Many governments in sub-Saharan Africa denied that there was a problem for years, and are only now starting to work towards solutions. Underfunding is a problem in all areas of HIV prevention when compared to even conservative estimates of the problems.
- Recent research by the Overseas Development Institute (ODI) has suggested that the private sector has begun to recognize the impact of HIV/AIDS on the bottom line, both directly and indirectly.
- It is estimated that a company can generate an average return of US$3 for every US$1 invested in employee health due to a reduced absenteeism, better productivity and reduction in employee turnover.[14]
- Many multi-national corporations (MNCs) have therefore gotten involved in HIV/AIDS initiatives of three main types: a community-based partnerships, supply chain support, and sector-based initiatives.[15]
- The launching of the world's first official HIV/AIDS Toolkit in Zimbabwe on October 3 2006 is a product of collaborative work between the International Federation of Red Cross and Red Crescent Societies, World Health Organization and the Southern Africa HIV/AIDS Information Dissemination Service. [16]
- It is for the strengthening of people living with HIV/AIDS and nurses by minimal external support. The package, which is in form of eight modules focusing on basic facts about HIV and AIDS, was pre-tested in Zimbabwe in March 2006 to determine its adaptability. It disposes, among other things, categorized guidelines on clinical management, education and counseling of AIDS victims at community level.[16]
- The Copenhagen Consensus is a project that seeks to establish priorities for advancing global welfare using methodologies based on the theory of welfare economics. The participants are all economists, with the focus of the project being a rational prioritization based on economic analysis. The project is based on the contention that, in spite of the billions of dollars spent on global challenges by the United Nations, the governments of wealthy nations, foundations, charities, and non-governmental organizations, the money spent on problems such as malnutrition and climate change is not sufficient to meet many internationally-agreed targets. [17]
- The highest priority was assigned to implementing new measures to prevent the spread of HIV and AIDS. The economists estimated that an investment of $27 billion could avert nearly 30 million new infections by 2010.[17]
Reference
- ↑ 1.0 1.1 1.2 1.3 Greener R (2002). "AIDS and macroeconomic impact". In S, Forsyth (ed.). State of The Art: AIDS and Economics. IAEN. pp. 49&ndash, 55.
- ↑ Gebo KA, Fleishman JA, Conviser R, Hellinger J, Hellinger FJ, Josephs JS; et al. (2010). "Contemporary costs of HIV healthcare in the HAART era". AIDS. 24 (17): 2705–15. doi:10.1097/QAD.0b013e32833f3c14. PMC 3551268. PMID 20859193 PMID: 20859193 Check
|pmid=value (help). - ↑ Schackman BR, Gebo KA, Walensky RP, Losina E, Muccio T, Sax PE; et al. (2006). "The lifetime cost of current human immunodeficiency virus care in the United States". Med Care. 44 (11): 990–7. doi:10.1097/01.mlr.0000228021.89490.2a. PMID 17063130 PMID: 17063130 Check
|pmid=value (help). - ↑ Farnham PG, Hutchinson AB, Sansom SL, Branson BM (2008). "Comparing the costs of HIV screening strategies and technologies in health-care settings". Public Health Rep. 123 Suppl 3: 51–62. PMC 2567019. PMID 19166089 [ PMID: 19166089 [ Check
|pmid=value (help). - ↑ Shrestha RK, Clark HA, Sansom SL, Song B, Buckendahl H, Calhoun CB; et al. (2008). "Cost-effectiveness of finding new HIV diagnoses using rapid HIV testing in community-based organizations". Public Health Rep. 123 Suppl 3: 94–100. PMC 2567009. PMID 19166093 PMID: 19166093 Check
|pmid=value (help). - ↑ Phillips KA, Fernyak S (2000). "The cost-effectiveness of expanded HIV counselling and testing in primary care settings: a first look". AIDS. 14 (14): 2159–69. PMID 11061658 PMID: 11061658 Check
|pmid=value (help). - ↑ Farnham PG, Hutchinson AB, Sansom SL, Branson BM (2008). "Comparing the costs of HIV screening strategies and technologies in health-care settings". Public Health Rep. 123 Suppl 3: 51–62. PMC 2567019. PMID 19166089 PMID: 19166089 Check
|pmid=value (help). - ↑ Harrison KM, Song R, Zhang X (2010). "Life expectancy after HIV diagnosis based on national HIV surveillance data from 25 states, United States". J Acquir Immune Defic Syndr. 53 (1): 124–30. doi:10.1097/QAI.0b013e3181b563e7. PMID 19730109 PMID: 19730109 Check
|pmid=value (help). - ↑ "CDC HIV Cost-effectiveness".
- ↑ "CDC HIV Cost-effectiveness".
- ↑ 11.0 11.1 Over M (1992). "The macroeconomic impact of AIDS in Sub-Saharan Africa, Population and Human Resources Department". The World Bank.
- ↑ Bonnel R (2000). "HIV/AIDS and Economic Growth: A Global Perspective". S. A. J. Economics. 68 (5): 820&ndash, 855.
- ↑ Template:Cite paper
- ↑ Goetzel RZ, Ozminkowski RJ, Baase CM, Billotti GM (2005). "Estimating the return-on-investment from changes in employee health risks on the Dow Chemical Company's health care costs". Journal of Occupational and Environmental Medicine. 47: 759–68. PMID 16093925.
- ↑ "AIDS and the private sector: The case of South Africa" (PDF). Overseas Development Institute. 2007. Unknown parameter
|accessyear=ignored (|access-date=suggested) (help) - ↑ 16.0 16.1 Mu Xuequan (2006). "Zimbabwe launches world's first AIDS training package". xinhua. Retrieved 2006-10-03.
- ↑ 17.0 17.1 "$27 Billion Boost for HIV Prevention Programs Could Avert Majority of Projected HIV Infections Worldwide". kaisernetwork.org. 2002. Retrieved 2008-03-10.
- CS1 maint: Extra text: editors list
- CS1 errors: PMID
- CS1 maint: Explicit use of et al.
- CS1 maint: Multiple names: authors list
- CS1 maint: PMC format
- Pages with citations using unsupported parameters
- HIV/AIDS
- Disease
- Immune system disorders
- Viral diseases
- Pandemics
- Sexually transmitted infections
- Syndromes
- Virology
- AIDS origin hypotheses
- Medical disasters
- Immunodeficiency
- Microbiology
- Emergency mdicine
- Up-To-Date
- Infectious disease