Wolff-Parkinson-White syndrome EKG: Difference between revisions
Rim Halaby (talk | contribs) |
Rim Halaby (talk | contribs) |
||
| Line 43: | Line 43: | ||
The [[EKG]] findings include: | The [[EKG]] findings include: | ||
* Regular rhythm<br> | * Regular rhythm<br> | ||
* [[Wide QRS complexes]] | * [[Wide QRS complexes]] similar to that of [[ventricular tachycardia]]<br> | ||
[[File:Wide complex tachy.jpg|800px|center]] | [[File:Wide complex tachy.jpg|800px|center]] | ||
Revision as of 01:32, 18 April 2014
|
Wolff-Parkinson-White syndrome Microchapters |
|
Differentiating Wolff-Parkinson-White syndrome from other Diseases |
|---|
|
Diagnosis |
|
Treatment |
|
Case Studies |
|
Wolff-Parkinson-White syndrome EKG On the Web |
|
Risk calculators and risk factors for Wolff-Parkinson-White syndrome EKG |
Editor-In-Chief: C. Michael Gibson, M.S., M.D. [1]; Associate Editor-In-Chief: Cafer Zorkun, M.D., Ph.D. [2]
Overview
Wolff-Parkinson-White (WPW) pattern is characterized by the presence of characteristic ECG findings, such as a short PR interval and a delta wave. WPW syndrome is the occurrence of tachycardia with or without associated symptoms in a subject with existing WPW pattern.[1] Several types of arrhythmia can occur in WPW syndrome such as AV reentrant tachycardia (AVRT), atrial fibrillation,or atrial flutter, the most common of which is AVRT.[2] WPW syndrome can present as an orthodromic or antidromic AVRT during which the delta wave no longer appears. Atrial fibrillation in a patient with WPW should be suspected when there is ECG findings of an irregularly irregular rhythm and absent P waves suggestive of atrial fibrillation in the context of a heart rate higher than 220 beats per minute.
WPW Pattern
- WPW pattern is characterized by the following typical ECG findings:
- Short PR interval: The PR interval is short because the ventricles begins to contract earlier than usual because the electrical signal travels through the accessory pathway faster than the AV node.
- Wide QRS
- Presence of a delta wave
- Other findings that can be present in a subject with an accessory pathway include QRS alternans and ST segment depression.
Determining the location of the accessory pathway
| Check lead V1 | |||||
| Negative delta wave in V1 = right ventricle | Positive delta wave im V1= left ventricle | ||||
| Negative delta wave and QRS in II, III, AVF | Left axis | Inferior axis | Negative delta wave and QRS in II, III, AVF | Isoelectric or negative delta I, AVL, V5, V6 | |
| Posteroseptal | Right free wall | Anteroseptal | Posteroseptal | Lateral | |
WPW Syndrome
WPW syndrome is the occurrence of tachycardia with or without associated symptoms in a subject with existing WPW pattern.[3] Several types of arrhythmia can occur in WPW syndrome such as AV reentrant tachycardia (AVRT), atrial fibrillation,or atrial flutter, the most common of which is AVRT.[2]
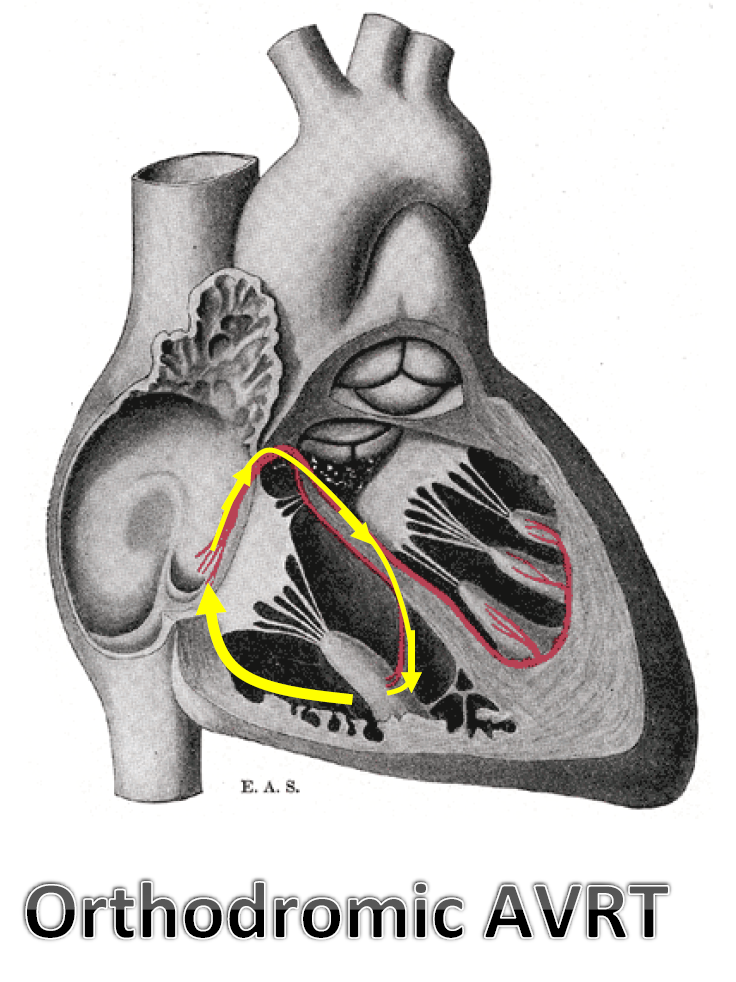
Orthodromic AVRT
In orthodromic AVRT, the anterograde conduction (from the atrium to the ventricle) passes through the AV node and the retrograde conduction (from the ventricle to the atrium) passes through the accessory pathway. Orthodromic AVRT occurs in approximately 90 to 95% of WPW.
The EKG findings include:
- Regular rhythm
- Narrow QRS complexes
- Retrograde P wave following the QRS complex
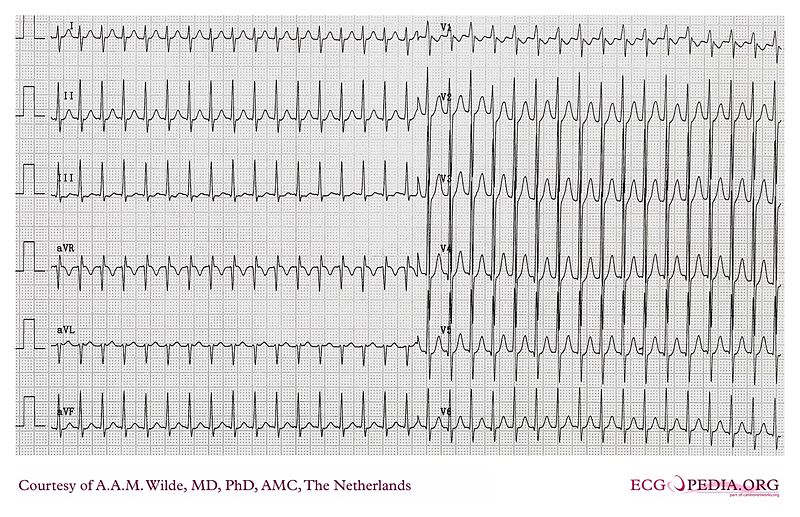
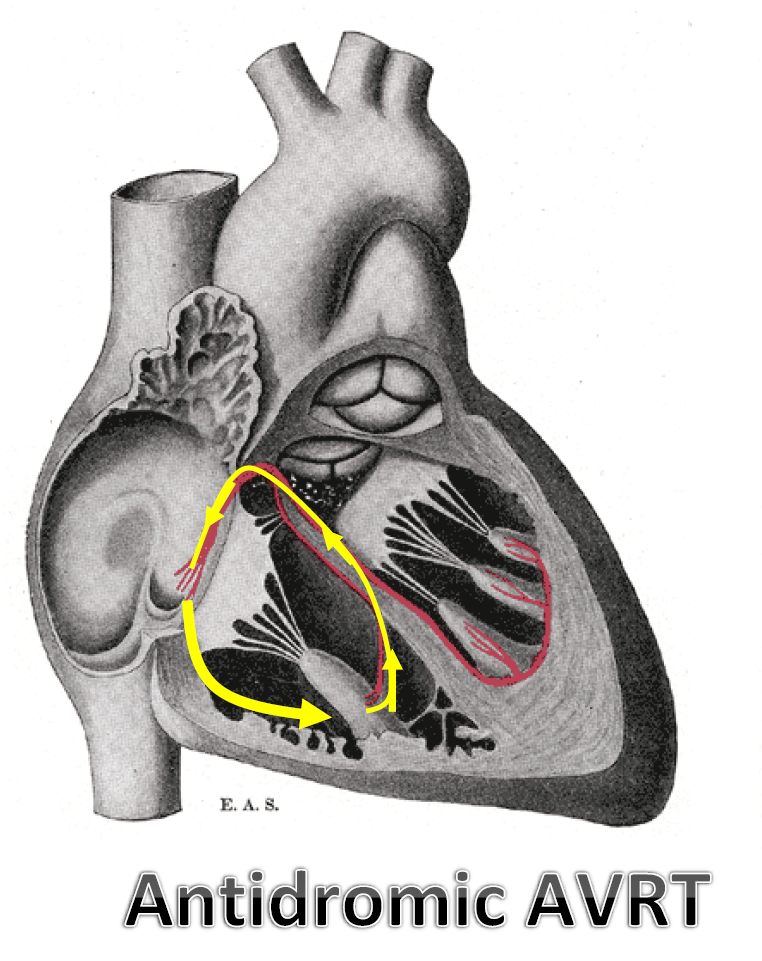
Antidromic AVRT
The anterograde conduction (from the atrium to the ventricle) passes through the accessory pathway and the retrograde conduction (from the ventricle to the atrium) passes through the AV node. It apprears in less than 10% of WPW.
The EKG findings include:
- Regular rhythm
- Wide QRS complexes similar to that of ventricular tachycardia
Clinical Manifestations
- The most common form of paroxysmal tachycardia in these patients is a circus movement tachycardia (CMT) incorporating the AP.
- The CMT utilizes the following structures: the AV node, the His-Purkinje system, the ventricular myocardium (from the terminal portion of the His system to the ventricular end of the AP), the AP itself, and the atrial myocardium itself from the atrial insertion of the AP to the AV node.
- This circuit can conduct in both directions:
- Type I A CMT:
- This is the usual form of the CMT in patients with WPW.
- Is antegrade through the AV node, VA conduction through the AP.
- The QRS complex during the tachycardia shows either normal intraventricular conduction or typical bundle branch block configuration.
- Symptoms: Palpitations (97%), dyspnea (57%), anginal pain (56%), perspiration (55%), fatigue (41%), anxiety (30%), dizziness (30%),polyuria (26%).
- This is also called orthodromic reentrant tachycardia.
- There is no delta wave.
- The rate is 140 to 250 bpm.
- It is faster than the rate of tachycardia due to reentry in the AV node.
- Often triggered by a PAC
- Type I A CMT:
- Type I B CMT:
- Anterograde down the accessory pathway, retrograde in the AVN-His pathway.
- The QRS is widened (wide QRS)
- This form is rare.
- Also called antidromic reentrant tachycardia.
- Type I B CMT:
- Type II CMT (intra-AV nodal):
- Anterograde pathway is an AV nodal slow pathway, the retrograde pathway is an AV nodal fast pathway.
- No evidence of ventricular pre-excitation during the tachycardia.
- Type III CMT (uses two accessory pathways):
- Conducts anterograde down one accessory pathway and retrograde up a second accessory pathway.
- These patients can also experience atrial tachycardias and ventricular tachycardias.
- Type II CMT (intra-AV nodal):
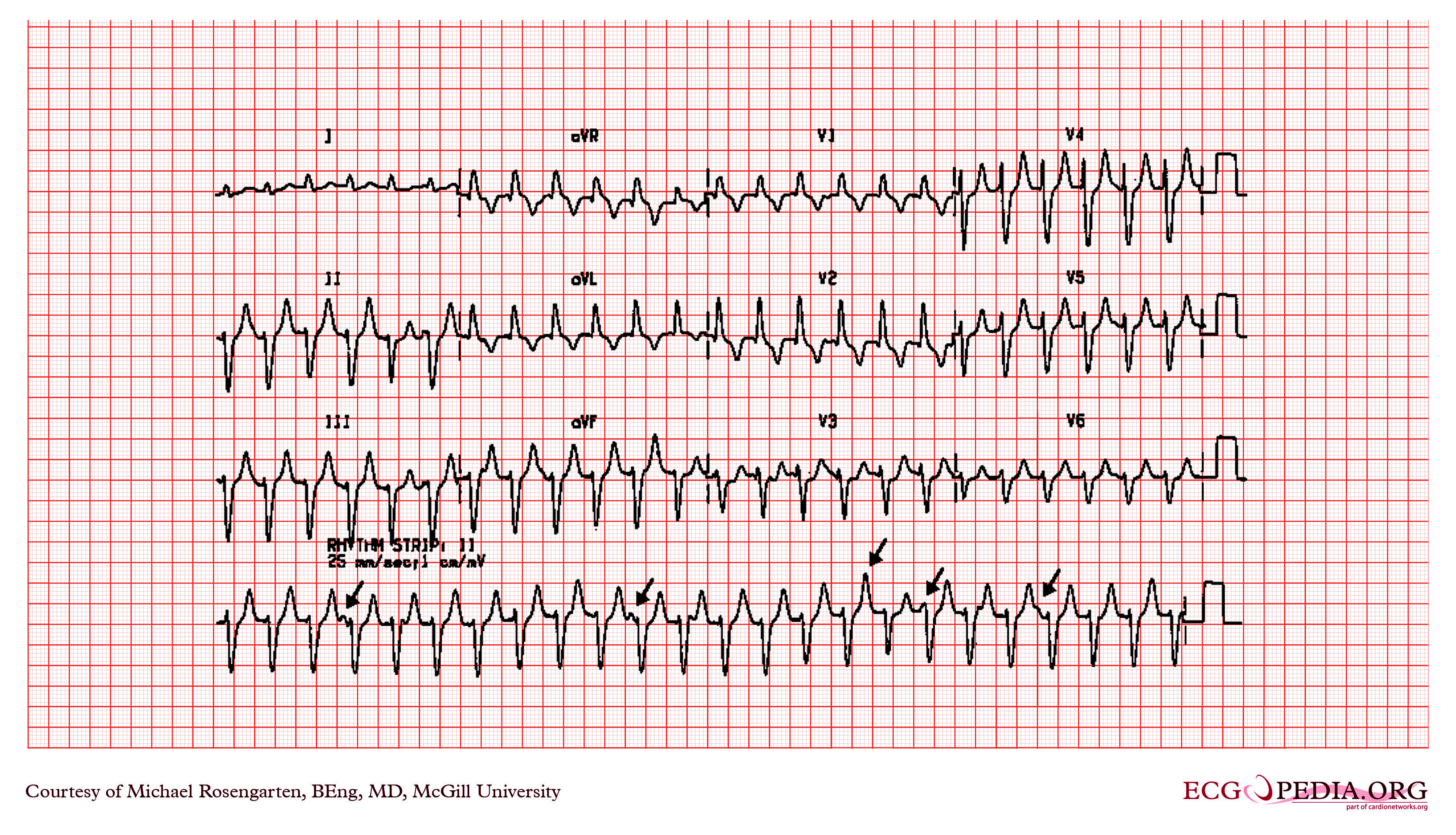
Atrial Fibrillation in WPW
Can cause life-threatening ventricular rates due to the exclusive AV conduction over the accessory pathway.
- Reduces cardiac output.
- May degenerate into VF, particularly in those with multiple bypass tracts.
- The only marker identified for degeneration into VF in the literature was the occurrence of RR intervals equal to or less than 205 msec during the a fib
- Seen in 78 of 256 of Wellen's patients with WPW. Reported incidence is 20 to 35% in other studies.
- The degree of ventricular preexcitation observed in the EKG during NSR bears no relationship whatsoever to the risk of developing life-threatening ventricular rates during the a.fib.
- The QRS complexes are wide and bizarre as a result of preexcitation.
- The ventricular rate is 220 to 360 beats per minute due to the short effective refractory period of the accessory pathway.
- It is often mistaken for VT.
- If the atrial rate in atrial fibrillation is greater than 200 BPM then suspect this. The rhythm will also be grossly irregular if it is due to atrial fibrillation. Such a rapid rate would be unusual if it were due to conduction by way of the normal AV conduction system.
Examples
Shown below is an EKG of Wolff-Parkinson-White syndrome demonstrating slurred upstroke of the QRS complex (>110 milli sec), resulting in a delta-wave (arrow). The EKG also shows a short PR interval.
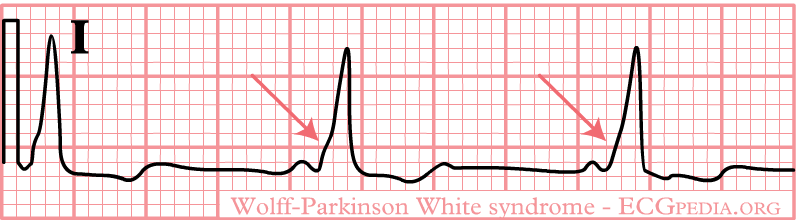
Copyleft image obtained courtesy of ECGpedia,http://en.ecgpedia.org/wiki/Main_Page
Shown below is an EKG showing a slurred upstroke QRS complex which is best appreciated in the precordial leads and a PR interval of less than 120 ms (short PR interval) suggesting WPW syndrome.
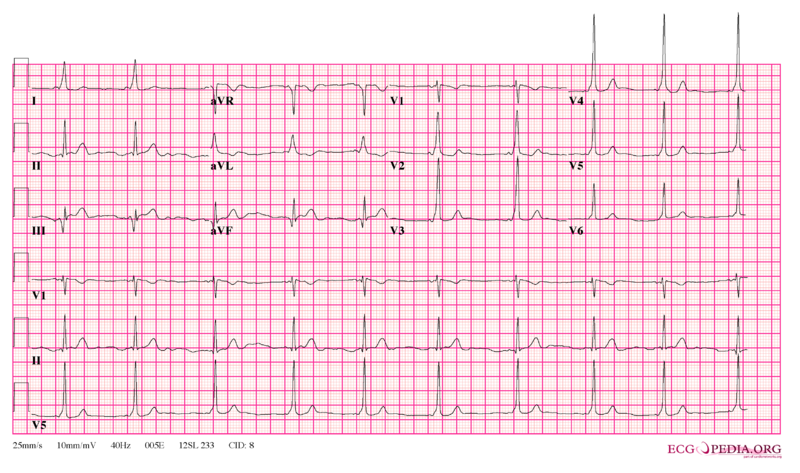
Copyleft image obtained courtesy of ECGpedia,http://en.ecgpedia.org/wiki/Main_Page
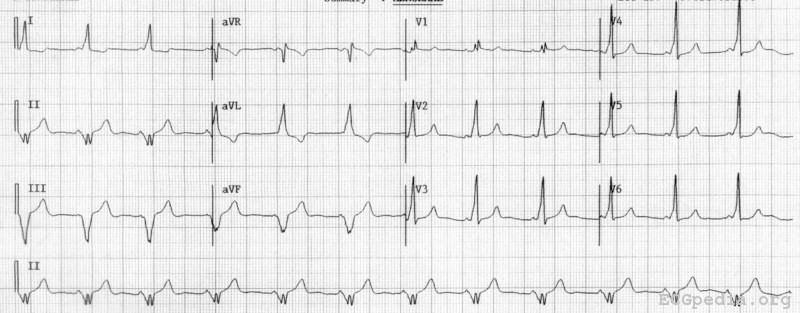
Shown below is an EKG demonstrating a delta wave in leads V2, I, aVL, with wide QRS complexes and left axis deviation suggesting WPW syndrome.

Copyleft image obtained courtesy of ECGpedia,http://en.ecgpedia.org/wiki/Main_Page
Shown below is an EKG showing a short PR interval of less than 120 ms, delta waves in leads I, aVF, aVL and chest leads with wide QRS complexes indicating WPW syndrome.
Copyleft image obtained courtesy of ECGpedia,http://en.ecgpedia.org/wiki/Main_Page
- For more EKG examples of Wolff-Parkinson-White syndrome click here.
References
- ↑ "Wolff-Parkinson-White Syndrome and Accessory Pathways". Retrieved 1 April 2014.
- ↑ 2.0 2.1 "ACC/AHA/ESC Guidelines for the Management of Patients With Supraventricular Arrhythmias—Executive Summary". Retrieved 15 August 2013.
- ↑ "Wolff-Parkinson-White Syndrome and Accessory Pathways". Retrieved 1 April 2014.