Warthin's tumor pathophysiology
Editor-In-Chief: C. Michael Gibson, M.S., M.D. [1]
|
Warthin's tumor Microchapters |
|
Diagnosis |
|---|
|
Treatment |
|
Case Studies |
|
Warthin's tumor pathophysiology On the Web |
|
American Roentgen Ray Society Images of Warthin's tumor pathophysiology |
|
Risk calculators and risk factors for Warthin's tumor pathophysiology |
Overview
Warthin's tumor arises from salivary gland epithelium, which are secretary cells of salivary gland. On gross pathology, cystic and multicentric appearance are characteristic findings of Warthin's tumor. On microscopic histopathological analysis, papillae, fibrous capsule, and cystic spaces are characteristic findings of Warthin's tumor.
Pathogenesis
- Warthin tumors (or papillary cystadenoma lymphomatosum) are a benign, sharply demarcated tumor of the salivary gland. They are bilateral in 10-15% of cases.
- The gland most likely affected is the parotid gland. In fact, it is the only tumor virtually restricted to the parotid gland. Though much less likely to occur thanpleomorphic adenoma, Warthin's tumor is the second most common benign parotid tumor.
- The first symptom is usually a painless, slow-growing bump in front of the ear, on the bottom of the mouth, or under the chin. Warthin tumors may increase in size over time, but few become cancerous.
- The tumor is slow growing, painless, and usually appears in the tail of the parotid gland near the angle of the mandible. In 5–14% of cases, Warthin's tumor is bilateral, but the two masses usually are at different times. Warthin's tumor is highly unlikely to become malignant.[1]
Genetics
- Expression of CRTC1 - MAML2 chimeric genes through t(11;19)(q21;p13) translocation is involved in the pathogenesis of Warthin's tumor.
Gross Pathology
- They are often multicentric (20%) and are usually small (1-4 cm). They have a typically heterogeneous appearance on all modalities, often with cystic components (30%).[2]
- The size of the tumor is 2.5 centimeter.
- They tends to favour the parotid tail region.
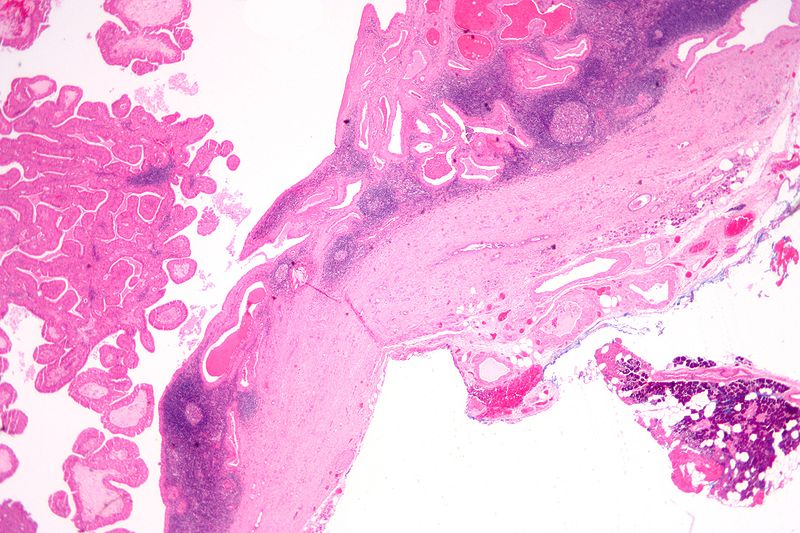
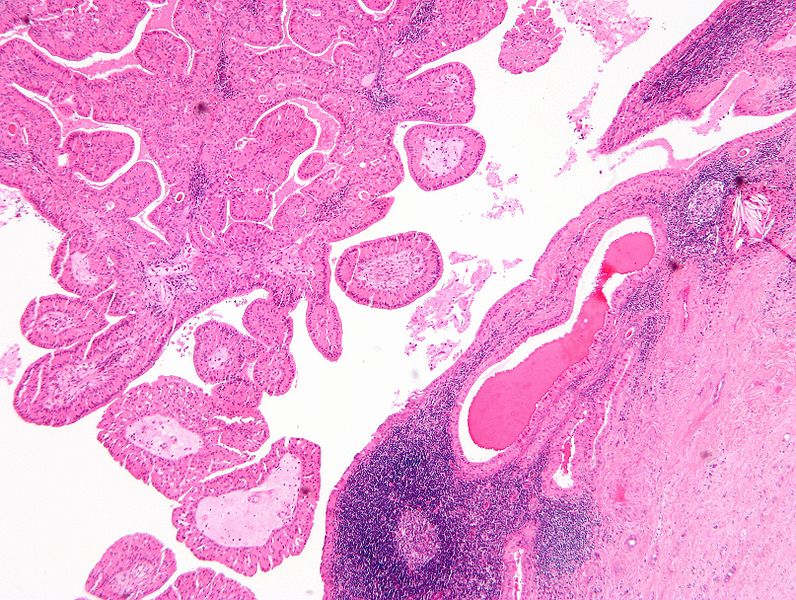
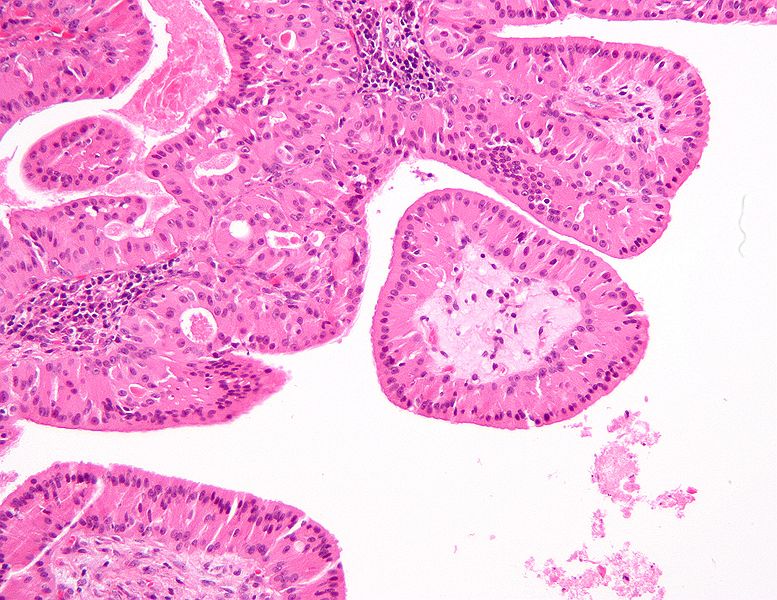
Microscopic Pathology
- The appearance of this tumor under the microscope is unique. There are cystic spaces surrounded by two uniform rows of cells with centrally placed pyknotic nuclei.
- The cystic spaces have epithelium referred to as papillary infoldings that protude into them. Additionally, the epithelium has lymphoid stroma with germinal center formation.
- Papillae (nipple-shaped structures) with a two rows of pink (eosinophilic) epithelial cells (with cuboidal basal cells and columnar luminal cells) - key feature.
- Fibrous capsule - pink & homogenous on H&E stain.
- Cystic space filled with debris in situ (not necrosis).
- Lymphoid stroma
- Additionally, the epithelium has lymphoid stroma with germinal center formation. [3]
-
Histopathology of Warthin tumor in the parotid gland. H&E stain[4]
-
Histopathology of Warthin tumor in the parotid gland. Another view of a file "Warthin tumor (1).jpg". H&E stain..[4]
-
Histopathology of Warthin tumor in the parotid gland. Higher magnification of a file "Warthin tumor (1).jpg". H&E stain.[4]
-
Histopathology of Warthin tumor in the parotid gland. Image courtesy of Nephron librepathology (original file ‘’here’’). Creative Commons BYSANC
-
Histopathology of Warthin tumor in the parotid gland. Image courtesy of Nephron librepathology (original file ‘’here’’). Creative Commons BYSANC
-
Histopathology of Warthin tumor in the parotid gland. Image courtesy of Nephron librepathology (original file ‘’here’’). Creative Commons BYSANC
-
Histopathology of Warthin tumor in the parotid gland. Image courtesy of Nephron librepathology (original file ‘’here’’). Creative Commons BYSANC
References
- ↑ NIH Warthin tumor. Rarediseases (2015). https://rarediseases.info.nih.gov/gard/8569/warthin-tumor/resources/1 Accessed on December 02, 2015
- ↑ Blake, Michael (2009). Adrenal imaging. Totowa, NJ: Humana Press. ISBN 193411586X.
- ↑ Warthin's tumor librepathology (2015) http://librepathology.org/wiki/index.php/Warthin_tumour Accessed on December 14, 2015
- ↑ 4.0 4.1 4.2 Abid, Syed A.; Stack, Brendan C.; Bodenner, Donald L. (2014). "Metastatic Follicular Thyroid Carcinoma Secreting Thyroid Hormone and Radioiodine Avid without Stimulation: A Case Report and Literature Review". Case Reports in Endocrinology. 2014: 1–6. doi:10.1155/2014/584513. ISSN 2090-6501.
![Histopathology of Warthin tumor in the parotid gland. H&E stain[4]](/images/c/c7/Warthin_tumor_%281%29.jpg)
![Histopathology of Warthin tumor in the parotid gland. Another view of a file "Warthin tumor (1).jpg". H&E stain..[4]](/images/c/cb/Warthin_tumor_%282%29.jpg)
![Histopathology of Warthin tumor in the parotid gland. Higher magnification of a file "Warthin tumor (1).jpg". H&E stain.[4]](/images/d/d2/Warthin_tumor_%283%29.jpg)