Tricuspid stenosis diagnostic study of choice: Difference between revisions
| (14 intermediate revisions by the same user not shown) | |||
| Line 1: | Line 1: | ||
__NOTOC__ | __NOTOC__ | ||
{{Tricuspid stenosis}} | {{Tricuspid stenosis}} | ||
{{CMG}}; {{AE}} | {{CMG}}; {{AE}} {{VKG}} | ||
== Overview == | == Overview == | ||
[[Tricuspid stenosis]] (TS) is characterized by structural changes in the [[tricuspid valve]]. The most common cause of [[tricuspid stenosis]] (TS) is [[rheumatic heart disease]]. Echocardiography is the gold standard test for the diagnosis of tricuspid stenosis which gives tricuspid peak inflow velocity and degree of thickening of tricuspid valve leaflets. | [[Tricuspid stenosis]] (TS) is characterized by structural changes in the [[tricuspid valve]]. The most common cause of [[tricuspid stenosis]] (TS) is [[rheumatic heart disease]]. Echocardiography is the gold standard test for the diagnosis of tricuspid stenosis which gives tricuspid peak inflow velocity and degree of thickening of tricuspid valve leaflets. | ||
| Line 9: | Line 9: | ||
=== Study of choice === | === Study of choice === | ||
* Echocardiography is the gold standard test for the diagnosis of tricuspid stenosis. | *[[Echocardiography]] is the gold standard test for the diagnosis of [[tricuspid stenosis]]. | ||
* The following result of echocardiography is confirmatory of tricuspid stenosis:<ref name="MorganForker1971">{{cite journal|last1=Morgan|first1=Jacob R.|last2=Forker|first2=Alan D.|last3=Coates|first3=J. R.|last4=Myers|first4=W. S.|title=Isolated Tricuspid Stenosis|journal=Circulation|volume=44|issue=4|year=1971|pages=729–732|issn=0009-7322|doi=10.1161/01.CIR.44.4.729}}</ref><ref name="FinneganAbrams1973">{{cite journal|last1=Finnegan|first1=P|last2=Abrams|first2=L D|title=Isolated tricuspid stenosis.|journal=Heart|volume=35|issue=11|year=1973|pages=1207–1210|issn=1355-6037|doi=10.1136/hrt.35.11.1207}}</ref> | * The following result of [[echocardiography]] is confirmatory of [[tricuspid stenosis]]:<ref name="MorganForker1971">{{cite journal|last1=Morgan|first1=Jacob R.|last2=Forker|first2=Alan D.|last3=Coates|first3=J. R.|last4=Myers|first4=W. S.|title=Isolated Tricuspid Stenosis|journal=Circulation|volume=44|issue=4|year=1971|pages=729–732|issn=0009-7322|doi=10.1161/01.CIR.44.4.729}}</ref><ref name="FinneganAbrams1973">{{cite journal|last1=Finnegan|first1=P|last2=Abrams|first2=L D|title=Isolated tricuspid stenosis.|journal=Heart|volume=35|issue=11|year=1973|pages=1207–1210|issn=1355-6037|doi=10.1136/hrt.35.11.1207}}</ref><ref name="BaumgartnerHung2009">{{cite journal|last1=Baumgartner|first1=Helmut|last2=Hung|first2=Judy|last3=Bermejo|first3=Javier|last4=Chambers|first4=John B.|last5=Evangelista|first5=Arturo|last6=Griffin|first6=Brian P.|last7=Iung|first7=Bernard|last8=Otto|first8=Catherine M.|last9=Pellikka|first9=Patricia A.|last10=Quiñones|first10=Miguel|title=Echocardiographic Assessment of Valve Stenosis: EAE/ASE Recommendations for Clinical Practice|journal=Journal of the American Society of Echocardiography|volume=22|issue=1|year=2009|pages=1–23|issn=08947317|doi=10.1016/j.echo.2008.11.029}}</ref> | ||
**The degree of thickening of tricuspid valve leaflets | **The degree of thickening of [[Tricuspid valve|tricuspid]] valve leaflets | ||
**Calcification of tricuspid valve leaflets | **[[Calcification]] of [[tricuspid valve]] leaflets | ||
**Limited leaflet mobility of tricuspid valve leaflets | **Limited leaflet mobility of [[tricuspid valve]] leaflets | ||
**Reduced separation of the tricuspid valve leaflet tips | **Reduced separation of the [[tricuspid valve]] leaflet tips | ||
**Diastolic doming of the tricuspid valve | **[[Diastole|Diastolic]] doming of the [[tricuspid valve]] | ||
**Echocardiography gives the degree of fusion of the commissures and chordae tendineae of the tricuspid valve | **[[Echocardiography]] gives the degree of fusion of the [[commissures]] and [[chordae tendineae]] of the [[tricuspid valve]] | ||
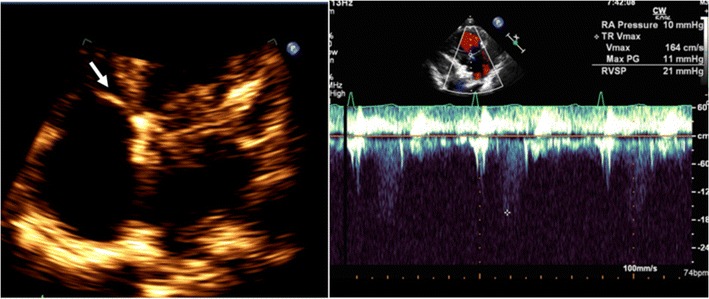
[[File:Normal echocardiographic appearance of tricuspid valve.jpg|center|thumb|709x709px|Normal echocardiographic appearance of tricuspid valve (''arrow'') and wave pattern. Case courtesy by Soham Shah et al<ref>{{Cite web|url=https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5028338/|title=Multimodal imaging of the tricuspid valve: normal appearance and pathological entities|last=|first=|date=|website=|archive-url=|archive-date=|dead-url=|access-date=}}</ref>]] | |||
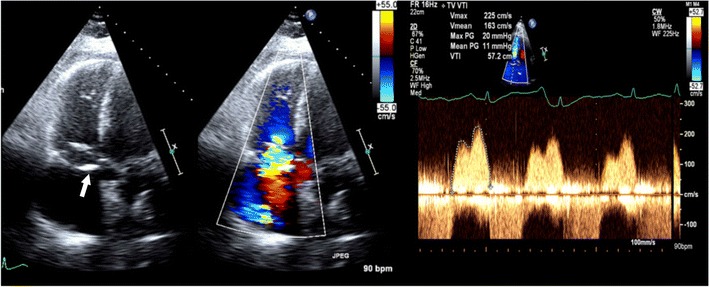
[[File:Tricuspid stenosis in echocardiography.jpg|alt=Tricuspid stenosis in echocardiography|center|thumb|709x709px|Tricuspid stenosis in echocardiography. 2D and color Doppler images in a patient with antiphospholipid antibody syndrome shows thickening of the valve leaflets (''arrow'') and continuous-wave Doppler with a mean pressure gradient of 11 mmHg, which is consistent with severe tricuspid stenosis. Case courtesy by Soham Shah et al<ref>{{Cite web|url=https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5028338/|title=Multimodal imaging of the tricuspid valve: normal appearance and pathological entities|last=|first=|date=|website=|archive-url=|archive-date=|dead-url=|access-date=}}</ref>]] | |||
=== Staging of Tricuspid stenosis === | |||
* Based on the valve anatomy, hemodynamics, and consequences tricuspid stenosis can be staged into the following:<ref name="NishimuraOtto2014">{{cite journal|last1=Nishimura|first1=Rick A.|last2=Otto|first2=Catherine M.|last3=Bonow|first3=Robert O.|last4=Carabello|first4=Blase A.|last5=Erwin|first5=John P.|last6=Guyton|first6=Robert A.|last7=O’Gara|first7=Patrick T.|last8=Ruiz|first8=Carlos E.|last9=Skubas|first9=Nikolaos J.|last10=Sorajja|first10=Paul|last11=Sundt|first11=Thoralf M.|last12=Thomas|first12=James D.|title=2014 AHA/ACC Guideline for the Management of Patients With Valvular Heart Disease|journal=Journal of the American College of Cardiology|volume=63|issue=22|year=2014|pages=e57–e185|issn=07351097|doi=10.1016/j.jacc.2014.02.536}}</ref><ref name="NishimuraOtto2017">{{cite journal|last1=Nishimura|first1=Rick A.|last2=Otto|first2=Catherine M.|last3=Bonow|first3=Robert O.|last4=Carabello|first4=Blase A.|last5=Erwin|first5=John P.|last6=Fleisher|first6=Lee A.|last7=Jneid|first7=Hani|last8=Mack|first8=Michael J.|last9=McLeod|first9=Christopher J.|last10=O’Gara|first10=Patrick T.|last11=Rigolin|first11=Vera H.|last12=Sundt|first12=Thoralf M.|last13=Thompson|first13=Annemarie|title=2017 AHA/ACC Focused Update of the 2014 AHA/ACC Guideline for the Management of Patients With Valvular Heart Disease: A Report of the American College of Cardiology/American Heart Association Task Force on Clinical Practice Guidelines|journal=Circulation|volume=135|issue=25|year=2017|issn=0009-7322|doi=10.1161/CIR.0000000000000503}}</ref><ref name="NishimuraOtto20142">{{cite journal|last1=Nishimura|first1=Rick A.|last2=Otto|first2=Catherine M.|last3=Bonow|first3=Robert O.|last4=Carabello|first4=Blase A.|last5=Erwin|first5=John P.|last6=Guyton|first6=Robert A.|last7=O'Gara|first7=Patrick T.|last8=Ruiz|first8=Carlos E.|last9=Skubas|first9=Nikolaos J.|last10=Sorajja|first10=Paul|last11=Sundt|first11=Thoralf M.|last12=Thomas|first12=James D.|title=2014 AHA/ACC Guideline for the Management of Patients With Valvular Heart Disease: Executive Summary|journal=Journal of the American College of Cardiology|volume=63|issue=22|year=2014|pages=2438–2488|issn=07351097|doi=10.1016/j.jacc.2014.02.537}}</ref><ref name="NishimuraOtto20144">{{cite journal|last1=Nishimura|first1=Rick A.|last2=Otto|first2=Catherine M.|last3=Bonow|first3=Robert O.|last4=Carabello|first4=Blase A.|last5=Erwin|first5=John P.|last6=Guyton|first6=Robert A.|last7=O’Gara|first7=Patrick T.|last8=Ruiz|first8=Carlos E.|last9=Skubas|first9=Nikolaos J.|last10=Sorajja|first10=Paul|last11=Sundt|first11=Thoralf M.|last12=Thomas|first12=James D.|title=2014 AHA/ACC Guideline for the Management of Patients With Valvular Heart Disease: Executive Summary|journal=Circulation|volume=129|issue=23|year=2014|pages=2440–2492|issn=0009-7322|doi=10.1161/CIR.0000000000000029}}</ref><ref name="NishimuraOtto20143">{{cite journal|last1=Nishimura|first1=Rick A.|last2=Otto|first2=Catherine M.|last3=Bonow|first3=Robert O.|last4=Carabello|first4=Blase A.|last5=Erwin|first5=John P.|last6=Guyton|first6=Robert A.|last7=O’Gara|first7=Patrick T.|last8=Ruiz|first8=Carlos E.|last9=Skubas|first9=Nikolaos J.|last10=Sorajja|first10=Paul|last11=Sundt|first11=Thoralf M.|last12=Thomas|first12=James D.|title=2014 AHA/ACC Guideline for the Management of Patients With Valvular Heart Disease|journal=Circulation|volume=129|issue=23|year=2014|issn=0009-7322|doi=10.1161/CIR.0000000000000031}}</ref> | |||
{| class="wikitable" | |||
!Stage | |||
! Definition | |||
!Valve anatomy | |||
!Valve hemodynamics | |||
!Hemodynamic consequences | |||
!Symptoms | |||
{| | |||
! | |||
! | |||
! | |||
|- | |- | ||
|C, D | |||
| | |Severe TS | ||
| | |Thickened, distorted, [[Calcification|calcified]] leaflets | ||
| | | | ||
*T ½ ≥190 ms | |||
*[[Valve]] area ≤1.0 cm2 | |||
|Right atrial / [[Inferior vena cava]] enlargement | |||
| | |||
*Stage C-No [[symptoms]] | |||
*Stage D-[[Symptom|Symptoms]] variable and dependent on the severity of associated valve disease and degree of obstruction | |||
|} | |} | ||
==References== | ==References== | ||
Latest revision as of 14:07, 1 April 2020
|
Tricuspid stenosis Microchapters |
|
Diagnosis |
|---|
|
Treatment |
|
Case Studies |
|
Tricuspid stenosis diagnostic study of choice On the Web |
|
American Roentgen Ray Society Images of Tricuspid stenosis diagnostic study of choice |
|
Risk calculators and risk factors for Tricuspid stenosis diagnostic study of choice |
Editor-In-Chief: C. Michael Gibson, M.S., M.D. [1]; Associate Editor(s)-in-Chief: Vamsikrishna Gunnam M.B.B.S [2]
Overview
Tricuspid stenosis (TS) is characterized by structural changes in the tricuspid valve. The most common cause of tricuspid stenosis (TS) is rheumatic heart disease. Echocardiography is the gold standard test for the diagnosis of tricuspid stenosis which gives tricuspid peak inflow velocity and degree of thickening of tricuspid valve leaflets.
Diagnostic Study of Choice
Study of choice
- Echocardiography is the gold standard test for the diagnosis of tricuspid stenosis.
- The following result of echocardiography is confirmatory of tricuspid stenosis:[1][2][3]
- The degree of thickening of tricuspid valve leaflets
- Calcification of tricuspid valve leaflets
- Limited leaflet mobility of tricuspid valve leaflets
- Reduced separation of the tricuspid valve leaflet tips
- Diastolic doming of the tricuspid valve
- Echocardiography gives the degree of fusion of the commissures and chordae tendineae of the tricuspid valve
Staging of Tricuspid stenosis
- Based on the valve anatomy, hemodynamics, and consequences tricuspid stenosis can be staged into the following:[6][7][8][9][10]
| Stage | Definition | Valve anatomy | Valve hemodynamics | Hemodynamic consequences | Symptoms |
|---|---|---|---|---|---|
| C, D | Severe TS | Thickened, distorted, calcified leaflets |
|
Right atrial / Inferior vena cava enlargement |
References
- ↑ Morgan, Jacob R.; Forker, Alan D.; Coates, J. R.; Myers, W. S. (1971). "Isolated Tricuspid Stenosis". Circulation. 44 (4): 729–732. doi:10.1161/01.CIR.44.4.729. ISSN 0009-7322.
- ↑ Finnegan, P; Abrams, L D (1973). "Isolated tricuspid stenosis". Heart. 35 (11): 1207–1210. doi:10.1136/hrt.35.11.1207. ISSN 1355-6037.
- ↑ Baumgartner, Helmut; Hung, Judy; Bermejo, Javier; Chambers, John B.; Evangelista, Arturo; Griffin, Brian P.; Iung, Bernard; Otto, Catherine M.; Pellikka, Patricia A.; Quiñones, Miguel (2009). "Echocardiographic Assessment of Valve Stenosis: EAE/ASE Recommendations for Clinical Practice". Journal of the American Society of Echocardiography. 22 (1): 1–23. doi:10.1016/j.echo.2008.11.029. ISSN 0894-7317.
- ↑ "Multimodal imaging of the tricuspid valve: normal appearance and pathological entities".
- ↑ "Multimodal imaging of the tricuspid valve: normal appearance and pathological entities".
- ↑ Nishimura, Rick A.; Otto, Catherine M.; Bonow, Robert O.; Carabello, Blase A.; Erwin, John P.; Guyton, Robert A.; O’Gara, Patrick T.; Ruiz, Carlos E.; Skubas, Nikolaos J.; Sorajja, Paul; Sundt, Thoralf M.; Thomas, James D. (2014). "2014 AHA/ACC Guideline for the Management of Patients With Valvular Heart Disease". Journal of the American College of Cardiology. 63 (22): e57–e185. doi:10.1016/j.jacc.2014.02.536. ISSN 0735-1097.
- ↑ Nishimura, Rick A.; Otto, Catherine M.; Bonow, Robert O.; Carabello, Blase A.; Erwin, John P.; Fleisher, Lee A.; Jneid, Hani; Mack, Michael J.; McLeod, Christopher J.; O’Gara, Patrick T.; Rigolin, Vera H.; Sundt, Thoralf M.; Thompson, Annemarie (2017). "2017 AHA/ACC Focused Update of the 2014 AHA/ACC Guideline for the Management of Patients With Valvular Heart Disease: A Report of the American College of Cardiology/American Heart Association Task Force on Clinical Practice Guidelines". Circulation. 135 (25). doi:10.1161/CIR.0000000000000503. ISSN 0009-7322.
- ↑ Nishimura, Rick A.; Otto, Catherine M.; Bonow, Robert O.; Carabello, Blase A.; Erwin, John P.; Guyton, Robert A.; O'Gara, Patrick T.; Ruiz, Carlos E.; Skubas, Nikolaos J.; Sorajja, Paul; Sundt, Thoralf M.; Thomas, James D. (2014). "2014 AHA/ACC Guideline for the Management of Patients With Valvular Heart Disease: Executive Summary". Journal of the American College of Cardiology. 63 (22): 2438–2488. doi:10.1016/j.jacc.2014.02.537. ISSN 0735-1097.
- ↑ Nishimura, Rick A.; Otto, Catherine M.; Bonow, Robert O.; Carabello, Blase A.; Erwin, John P.; Guyton, Robert A.; O’Gara, Patrick T.; Ruiz, Carlos E.; Skubas, Nikolaos J.; Sorajja, Paul; Sundt, Thoralf M.; Thomas, James D. (2014). "2014 AHA/ACC Guideline for the Management of Patients With Valvular Heart Disease: Executive Summary". Circulation. 129 (23): 2440–2492. doi:10.1161/CIR.0000000000000029. ISSN 0009-7322.
- ↑ Nishimura, Rick A.; Otto, Catherine M.; Bonow, Robert O.; Carabello, Blase A.; Erwin, John P.; Guyton, Robert A.; O’Gara, Patrick T.; Ruiz, Carlos E.; Skubas, Nikolaos J.; Sorajja, Paul; Sundt, Thoralf M.; Thomas, James D. (2014). "2014 AHA/ACC Guideline for the Management of Patients With Valvular Heart Disease". Circulation. 129 (23). doi:10.1161/CIR.0000000000000031. ISSN 0009-7322.