Thyroid cancer: Difference between revisions
No edit summary |
|||
| (69 intermediate revisions by 12 users not shown) | |||
| Line 1: | Line 1: | ||
__NOTOC__ | |||
{{Thyroid cancer}} | {{Thyroid cancer}} | ||
{{ | {{CMG}}; {{AE}} {{MJM}}; {{Ammu}}{{SMP}}{{Sahar}} | ||
==Overview== | |||
== | Thyroid cancer refers to any of four kinds of [[tumor]]s of the [[thyroid]] gland which include [[Papillary thyroid cancer|papillary]], [[Follicular thyroid cancer|follicular]], [[Medullary thyroid cancer|medullary]] and [[Anaplastic thyroid cancer|anaplastic tumors]]. [[Papillary thyroid cancer|Papillary]] and [[Follicular thyroid cancer|follicular]] tumors are the most common and are usually [[benign tumor|benign]]. [[Papillary thyroid cancer|Papillary]] and [[Follicular thyroid cancer|follicular]] tumors have a slow growth and may recur, but are generally not fatal in patients under 45 years of age. [[Medullary thyroid cancer|Medullary]] and [[Anaplastic thyroid cancer|anaplastic tumors]] are [[cancer|malignant]]. [[Medullary]] tumors have a good prognosis if the are restricted to the thyroid gland and a poorer prognosis if [[metastasis]] occurs. [[Anaplastic thyroid cancer|Anaplastic tumors]] are fast-growing and respond poorly to therapy. | ||
[[Thyroid nodule|Thyroid nodules]] are diagnosed by [[ultrasound]] guided [[fine needle aspiration]] or frequently by [[thyroidectomy]] (surgical removal and subsequent [[Histology|histological]] examination). As the thyroid cancer can uptake [[iodine]], [[radioactive iodine]] is commonly used for the treatment of thyroid carcinomas. However, radioactive iodine therapy is accompanied by [[thyroxine]] therapy to ensure [[TSH]] suppression. | |||
[[ | |||
==Classification== | ==Classification== | ||
Thyroid cancers can be classified according to their pathological characteristics. The following variants can be distinguished (distribution over various subtypes may show regional variation): | Thyroid cancers can be classified according to their pathological characteristics. The following variants can be distinguished (distribution over various subtypes may show regional variation): | ||
* [[Papillary]] | * [[Papillary thyroid cancer]] (75%, including mixed papillary/follicular) | ||
* [[ | * [[Follicular thyroid cancer]] (16%) | ||
* [[Medullary]] | * [[Medullary thyroid cancer]] (5-7%) | ||
* [[Anaplastic]] | * [[Anaplastic thyroid cancer]] (3%) | ||
* [[Lymphoma]] (1 | * [[Primary thyroid lymphoma|Lymphoma]] (1%) | ||
{| align="center" | |||
|- | |||
| | |||
{{Familytree/start}} | |||
{{Familytree| | | | | | | | | | | | | | A01 | | | | | | | | | | | | | | | | | | |A01= Thyroid carcinoma}} | |||
{{Familytree|boxstyle=text-align: left;| | |,|-|-|-|v|-|-|-|v|-|-|-|^|-|-|-|v|-|-|-|v|-|-|-|.| | | | | | | | | | | | | |}} | |||
{{Familytree|boxstyle=text-align: left;| | B01 | | B02 | | B03 | | | | | | B04 | | B05 | | B06 | | | | | | | | | | | | | | | | |B01=[[Papillary thyroid cancer]]|B02=[[Follicular thyroid cancer]]|B03=[[Medullary thyroid cancer]]|B04= [[Anaplastic thyroid cancer]]|B05=[[Primary thyroid lymphoma|Lymphoma]]|B06= [[Miscellaneous]]}} | |||
{{Familytree|boxstyle=text-align: left;| | |!| | | |!| | | | | | | | | | | |!| | | | | | | |!| | | | | | | | | | | |}} | |||
{{Familytree|boxstyle=text-align: left;| | C01 | | C02 | | | | | | | | | | C03 | | | | | | C04 | | | | | | | | | | | | | | | | |C01= | |||
•Follicular variant<br> | |||
•Tall cell<br> | |||
•Diffuse sclerosing<br> | |||
•Encapsulated<br> | |||
•Columnar<br> | |||
|C02= | |||
•Minimally invasive<br> | |||
•Overtly invasive<br> | |||
== | |C03= | ||
[[ | •Small cell<br> | ||
•Giant cell<br> | |||
|C04= | |||
•Sarcoma<br> | |||
•Lymphoma<br> | |||
•Squamous cell carcinoma<br> | |||
•Mucoepidermoid carcinoma<br> | |||
•Plasma cell tumors<br> | |||
•Direct extension<br> | |||
•Kidney<br> | |||
•Melanoma<br> | |||
•Colon<br> | |||
}} | |||
{{Familytree/end}} | |||
|} | |||
==Causes== | |||
* For more information on [[papillary thyroid cancer]] [[causes]], [[Papillary thyroid cancer causes|click here]]. | |||
* For more information on [[follicular thyroid cancer]] [[causes]], [[Follicular thyroid cancer causes|click here]]. | |||
* For more information on [[medullary thyroid cancer]] [[causes]], [[Medullary thyroid cancer causes|click here]]. | |||
* For more information on [[anaplastic thyroid cancer]] [[causes]], [[Anaplastic thyroid cancer causes|click here]]. | |||
* For more information on [[primary thyroid lymphoma]] [[causes]], [[Primary thyroid lymphoma|click here]]. | |||
=== | ==Differential diagnosis== | ||
Thyroid cancers should be [[Differential diagnosis|differentiated]] from one another and from various other [[diseases]]: | |||
{| border="3" | |||
|+ | |||
! style="background: #4479BA; width: 150px;" | {{fontcolor|#FFF| Disease Name}} | |||
! style="background: #4479BA; width: 150px;" | {{fontcolor|#FFF| Age of Onset}} | |||
! style="background: #4479BA; width: 150px;" | {{fontcolor|#FFF| Gender Preponderance}} | |||
! style="background: #4479BA; width: 150px;" | {{fontcolor|#FFF| Signs/Symptoms}} | |||
! style="background: #4479BA; width: 150px;" | {{fontcolor|#FFF| Imaging Feature(s)}} | |||
! style="background: #4479BA; width: 150px;" | {{fontcolor|#FFF| Macroscopic Feature(s)}} | |||
! style="background: #4479BA; width: 150px;" | {{fontcolor|#FFF| Microscopic Feature(s)}} | |||
! style="background: #4479BA; width: 150px;" | {{fontcolor|#FFF| Laboratory Findings(s)}} | |||
! style="background: #4479BA; width: 150px;" | {{fontcolor|#FFF| Other Feature(s)}} | |||
! style="background: #4479BA; width: 150px;" | {{fontcolor|#FFF| Microscopic Appearance}} | |||
|- | |||
! style="padding: 5px 5px; background: #DCDCDC; " align="left" |Papillary Thyroid Cancer<ref name="FaginMitsiades2008">{{cite journal|last1=Fagin|first1=James A.|last2=Mitsiades|first2=Nicholas|title=Molecular pathology of thyroid cancer: diagnostic and clinical implications|journal=Best Practice & Research Clinical Endocrinology & Metabolism|volume=22|issue=6|year=2008|pages=955–969|issn=1521690X|doi=10.1016/j.beem.2008.09.017}}</ref><ref name="Schlumberger1998">{{cite journal|last1=Schlumberger|first1=Martin Jean|title=Papillary and Follicular Thyroid Carcinoma|journal=New England Journal of Medicine|volume=338|issue=5|year=1998|pages=297–306|issn=0028-4793|doi=10.1056/NEJM199801293380506}}</ref><ref name="pmid20001718">{{cite journal |vauthors=Sipos JA |title=Advances in ultrasound for the diagnosis and management of thyroid cancer |journal=Thyroid |volume=19 |issue=12 |pages=1363–72 |date=December 2009 |pmid=20001718 |doi=10.1089/thy.2009.1608 |url=}}</ref> | |||
| style="padding: 5px 5px; background: #F5F5F5;" align="left" | | |||
* More common in the middle aged (30 - 50 years of age) | |||
| style="padding: 5px 5px; background: #F5F5F5;" align="left" | | |||
* More commonly affects women | |||
| style="padding: 5px 5px; background: #F5F5F5;" align="left" | | |||
*[[Asymptomatic]] [[thyroid]] [[mass]] or [[nodule]] | |||
*Compressive [[symptoms]], such as: | |||
*[[Dysphagia|Difficulty swallowing]]/[[Dyspnea|breathing]] | |||
*Persistent [[cough]] | |||
*[[Stridor]] | |||
*[[Vocal cord|Vocal chord]] [[paralysis]] | |||
*Rapid enlarging [[mass]] | |||
| style="padding: 5px 5px; background: #F5F5F5;" align="left" | | |||
* On [[ultrasound]] | |||
** [[Solitary]] [[mass]] with an irregular outline | |||
** Located in the sub-capsular region | |||
** High [[vascularity]] | |||
*[[Imaging]] features are not characteristic of this [[cancer]] | |||
| style="padding: 5px 5px; background: #F5F5F5;" align="left" | | |||
*[[Solitary]] hypoechogenic [[nodule]] with [[Lobule|lobulated]] margin which may extend into adjacent [[tissues]] | |||
*[[Calcification]] may be present or not | |||
| style="padding: 5px 5px; background: #F5F5F5;" align="left" | | |||
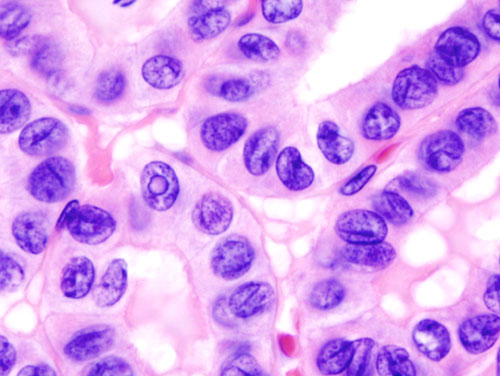
* Empty-appearing [[nuclei]] with central clearing (Orphan Annie eye) | |||
*[[Psammoma body|Psammoma bodies]] | |||
| style="padding: 5px 5px; background: #F5F5F5;" align="left" | | |||
*[[Thyroid function test|Thyroid function tests]] can be normal | |||
*Serum [[thyroglobulin]] can be used as a [[tumor marker]] | |||
| style="padding: 5px 5px; background: #F5F5F5;" align="left" | | |||
* History of [[radiation]] to the [[head]] and [[neck]] | |||
*[[BRAF]] and/or [[RET gene|RET]] [[mutation]] may be present | |||
*The most common type of thyroid cancer | |||
| style="padding: 5px 5px; background: #F5F5F5;" align="left" |[[Image:Thyroid papillary carcinoma histopathology (3).jpg|thumb|none|200px|Source:Wikimedia commons ]] | |||
|- | |||
! style="padding: 5px 5px; background: #DCDCDC; " align="left" |Follicular Thyroid Cancer<ref name="Schlumberger1998">{{cite journal|last1=Schlumberger|first1=Martin Jean|title=Papillary and Follicular Thyroid Carcinoma|journal=New England Journal of Medicine|volume=338|issue=5|year=1998|pages=297–306|issn=0028-4793|doi=10.1056/NEJM199801293380506}}</ref><ref name="pmid20001718">{{cite journal |vauthors=Sipos JA |title=Advances in ultrasound for the diagnosis and management of thyroid cancer |journal=Thyroid |volume=19 |issue=12 |pages=1363–72 |date=December 2009 |pmid=20001718 |doi=10.1089/thy.2009.1608 |url=}}</ref><ref name="pmid2019455">{{cite journal |vauthors=Pettersson B, Adami HO, Wilander E, Coleman MP |title=Trends in thyroid cancer incidence in Sweden, 1958-1981, by histopathologic type |journal=Int. J. Cancer |volume=48 |issue=1 |pages=28–33 |date=April 1991 |pmid=2019455 |doi=10.1002/ijc.2910480106 |url=}}</ref> | |||
| style="padding: 5px 5px; background: #F5F5F5;" align="left" | | |||
* Peak [[incidence]] at 40 - 60 years of age | |||
| style="padding: 5px 5px; background: #F5F5F5;" align="left" | | |||
* More commonly affects women | |||
| style="padding: 5px 5px; background: #F5F5F5;" align="left" | | |||
*[[Asymptomatic]] [[thyroid]] [[mass]] or [[nodule]] | |||
*Compressive [[symptoms]], such as: | |||
*[[Difficulty swallowing]]/[[Dyspnea|breathing]] | |||
*Persistent [[cough]] | |||
*[[Stridor]] | |||
*[[Vocal cord|Vocal chord]] [[paralysis]] | |||
*Rapid enlarging [[mass]] | |||
| style="padding: 5px 5px; background: #F5F5F5;" align="left" | | |||
* On [[ultrasound]]: | |||
**Solid hypoechoic [[nodule]] with a peripheral halo indicating [[fibrous capsule]] | |||
**Irregular margin | |||
*[[Imaging]] features are not characteristic of this [[cancer]] | |||
| style="padding: 5px 5px; background: #F5F5F5;" align="left" | | |||
* Single encapsulated [[nodule]] | |||
* Thick and irregular [[capsule]] | |||
* Can be [[cystic]] or [[hemorrhage|hemorrhagic]] in appearance | |||
| style="padding: 5px 5px; background: #F5F5F5;" align="left" | | |||
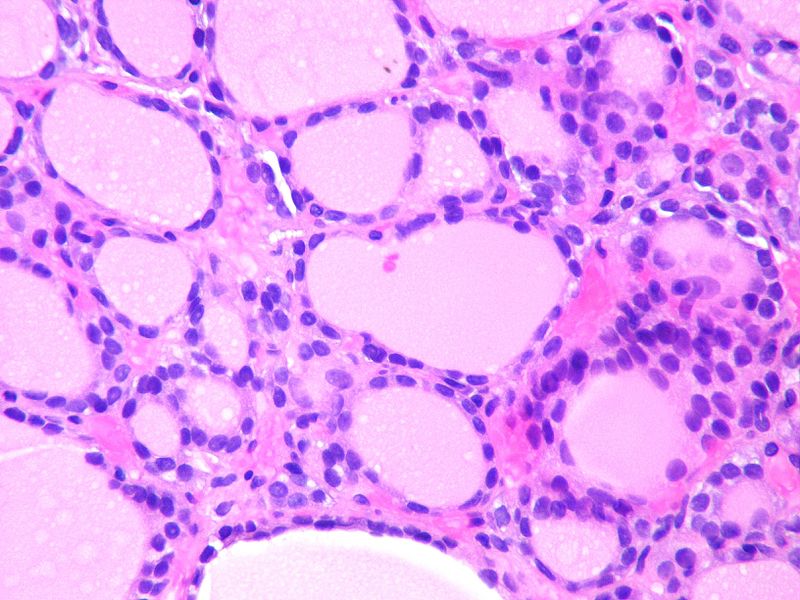
* Invades [[thyroid]] [[capsule]] and [[vasculature]] | |||
* Uniform [[Follicle|follicles]] <br /> | |||
| style="padding: 5px 5px; background: #F5F5F5;" align="left" | | |||
*[[Thyroid function test|Thyroid function tests]] can be normal | |||
* Serum [[thyroglobulin]] can be used as a [[tumor marker]] | |||
| style="padding: 5px 5px; background: #F5F5F5;" align="left" | | |||
*[[RASA3|RAS]] [[mutation]] may be present | |||
*[[PAX8]]-[[PPAR|PPARγ]] [[Translocation|translocations]] | |||
| style="padding: 5px 5px; background: #F5F5F5;" align="left" |[[Image:Metastatic follicular thyroid carcinoma - Case 264.jpg|thumb|none|200px|Source:Wikimedia common ]] | |||
|- | |||
! style="padding: 5px 5px; background: #DCDCDC;" align="left" |Medullary Thyroid Cancer<ref name="pmid6690009">{{cite journal |vauthors=Busnardo B, Girelli ME, Simioni N, Nacamulli D, Busetto E |title=Nonparallel patterns of calcitonin and carcinoembryonic antigen levels in the follow-up of medullary thyroid carcinoma |journal=Cancer |volume=53 |issue=2 |pages=278–85 |date=January 1984 |pmid=6690009 |doi=10.1002/1097-0142(19840115)53:2<278::aid-cncr2820530216>3.0.co;2-z |url=}}</ref><ref name="pmid10699905">{{cite journal |vauthors=Kebebew E, Ituarte PH, Siperstein AE, Duh QY, Clark OH |title=Medullary thyroid carcinoma: clinical characteristics, treatment, prognostic factors, and a comparison of staging systems |journal=Cancer |volume=88 |issue=5 |pages=1139–48 |date=March 2000 |pmid=10699905 |doi=10.1002/(sici)1097-0142(20000301)88:5<1139::aid-cncr26>3.0.co;2-z |url=}}</ref><ref name="HofstraLandsvater1994">{{cite journal|last1=Hofstra|first1=Robert M. W.|last2=Landsvater|first2=Rudy M.|last3=Ceccherini|first3=Isabella|last4=Stulp|first4=Rein P.|last5=Stelwagen|first5=Tineke|last6=Luo|first6=Yin|last7=Pasini|first7=Barbara|last8=Hoppener|first8=Jo W. M.|last9=van Amstel|first9=Hans Kristian Ploos|last10=Romeo|first10=Giovanni|last11=Lips|first11=Cornells J. M.|last12=Buys|first12=Charles H. C. M.|title=A mutation in the RET proto-oncogene associated with multiple endocrine neoplasia type 2B and sporadic medullary thyroid carcinoma|journal=Nature|volume=367|issue=6461|year=1994|pages=375–376|issn=0028-0836|doi=10.1038/367375a0}}</ref><ref name="pmid20001718">{{cite journal |vauthors=Sipos JA |title=Advances in ultrasound for the diagnosis and management of thyroid cancer |journal=Thyroid |volume=19 |issue=12 |pages=1363–72 |date=December 2009 |pmid=20001718 |doi=10.1089/thy.2009.1608 |url=}}</ref> | |||
==== | | style="padding: 5px 5px; background: #F5F5F5;" align="left" | | ||
*[[Incidence]] increases with age | |||
* More common in the 3rd to 4th decades of life | |||
| style="padding: 5px 5px; background: #F5F5F5;" align="left" | | |||
* Both genders are affected equally | |||
| style="padding: 5px 5px; background: #F5F5F5;" align="left" | | |||
*[[Solitary]] [[thyroid nodule]] | |||
* Mostly affects upper [[Lobe (anatomy)|lobe]] of [[thyroid gland]] | |||
* Possible [[systemic]] [[symptoms]] due to [[Hormone|hormonal]] [[secretion]] by the [[tumor]] | |||
*[[Cervical]] [[lymphadenopathy]] | |||
| style="padding: 5px 5px; background: #F5F5F5;" align="left" | | |||
*On [[ultrasound]]: | |||
**[[Solitary]] hypoechoic [[nodule]] with or without [[calcification]] | |||
*[[Imaging]] features are not characteristic of this [[cancer]] | |||
| style="padding: 5px 5px; background: #F5F5F5;" align="left" | | |||
* Single non-encapsulated mass | |||
* Gray-tan color | |||
| style="padding: 5px 5px; background: #F5F5F5;" align="left" | | |||
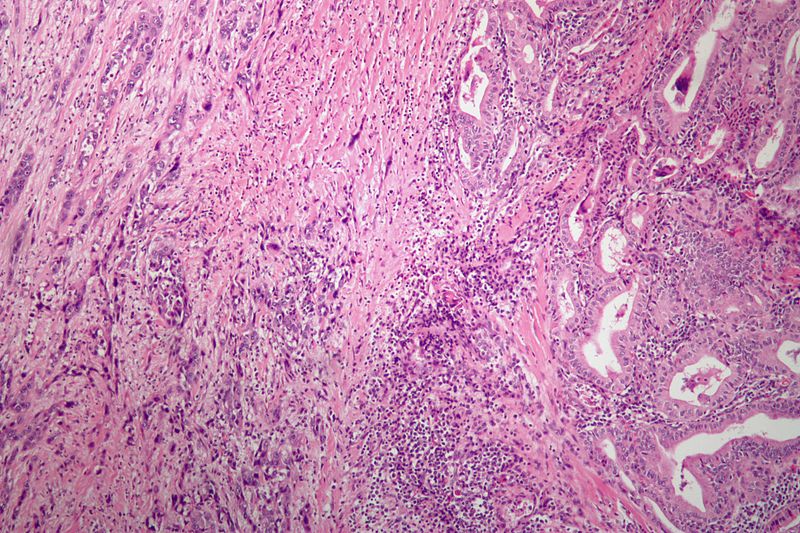
* Sheets of [[cells]] in an [[amyloid]] [[stroma]] | |||
| style="padding: 5px 5px; background: #F5F5F5;" align="left" | | |||
*[[Secretion|Secretes]] [[calcitonin]] | |||
*Normal [[thyroid function test|thyroid function tests]] | |||
*[[Carcinoembryonic antigen]] ([[CEA]]) may be used as a [[tumor marker]] | |||
*Rarely negative for [[calcitonin]] | |||
| style="padding: 5px 5px; background: #F5F5F5;" align="left" | | |||
* Can be part of [[MEN syndromes|MEN 2A]] and [[Multiple endocrine neoplasia type 2|2B syndrome]] | |||
* Can be associated with [[RET gene|RET]] [[mutation]] | |||
| style="padding: 5px 5px; background: #F5F5F5;" align="left" |[[File:Thyroid MedullaryCarcinoma SpindleCell LP PA.JPG|thumb|none|200px|Source:Wikimedia common ]] | |||
|- | |||
! style="padding: 5px 5px; background: #DCDCDC;" align="left" |Anaplastic Thyroid Cancer<ref name="pmid21772843">{{cite journal |vauthors=Nagaiah G, Hossain A, Mooney CJ, Parmentier J, Remick SC |title=Anaplastic thyroid cancer: a review of epidemiology, pathogenesis, and treatment |journal=J Oncol |volume=2011 |issue= |pages=542358 |date=2011 |pmid=21772843 |pmc=3136148 |doi=10.1155/2011/542358 |url=}}</ref><ref name="pmid2794956">{{cite journal |vauthors=Chang TC, Liaw KY, Kuo SH, Chang CC, Chen FW |title=Anaplastic thyroid carcinoma: review of 24 cases, with emphasis on cytodiagnosis and leukocytosis |journal=Taiwan Yi Xue Hui Za Zhi |volume=88 |issue=6 |pages=551–6 |date=June 1989 |pmid=2794956 |doi= |url=}}</ref><ref name="pmid1695118">{{cite journal |vauthors=Venkatesh YS, Ordonez NG, Schultz PN, Hickey RC, Goepfert H, Samaan NA |title=Anaplastic carcinoma of the thyroid. A clinicopathologic study of 121 cases |journal=Cancer |volume=66 |issue=2 |pages=321–30 |date=July 1990 |pmid=1695118 |doi=10.1002/1097-0142(19900715)66:2<321::aid-cncr2820660221>3.0.co;2-a |url=}}</ref> | |||
| style="padding: 5px 5px; background: #F5F5F5;" align="left" | | |||
* More common among older individuals | |||
*[[Mean]] age at [[diagnosis]] is 65 years | |||
| style="padding: 5px 5px; background: #F5F5F5;" align="left" | | |||
* More commonly affects women | |||
| style="padding: 5px 5px; background: #F5F5F5;" align="left" | | |||
* Rapidly enlarging [[thyroid]] [[mass]] | |||
* May manifest with compressive [[symptoms]] | |||
*Can present with [[signs]]/[[symptoms]] of [[metastasis]] | |||
*Constitutional [[symptoms]] may be present | |||
*Hard [[Nodule (medicine)|nodular]] [[goiter]] without [[tenderness]] | |||
| style="padding: 5px 5px; background: #F5F5F5;" align="left" | | |||
* On [[ultrasound]]: | |||
** Solid hypoechoic [[nodule]] with a peripheral halo indicating [[fibrous capsule]] | |||
** Irregular margin | |||
*[[Imaging]] features are not characteristic of this [[cancer]] | |||
| style="padding: 5px 5px; background: #F5F5F5;" align="left" | | |||
* Solid [[tumor]] with areas of [[necrosis]] and [[hemorrhage]] | |||
*[[Infiltration (medical)|Infiltrative]] pattern | |||
| style="padding: 5px 5px; background: #F5F5F5;" align="left" | | |||
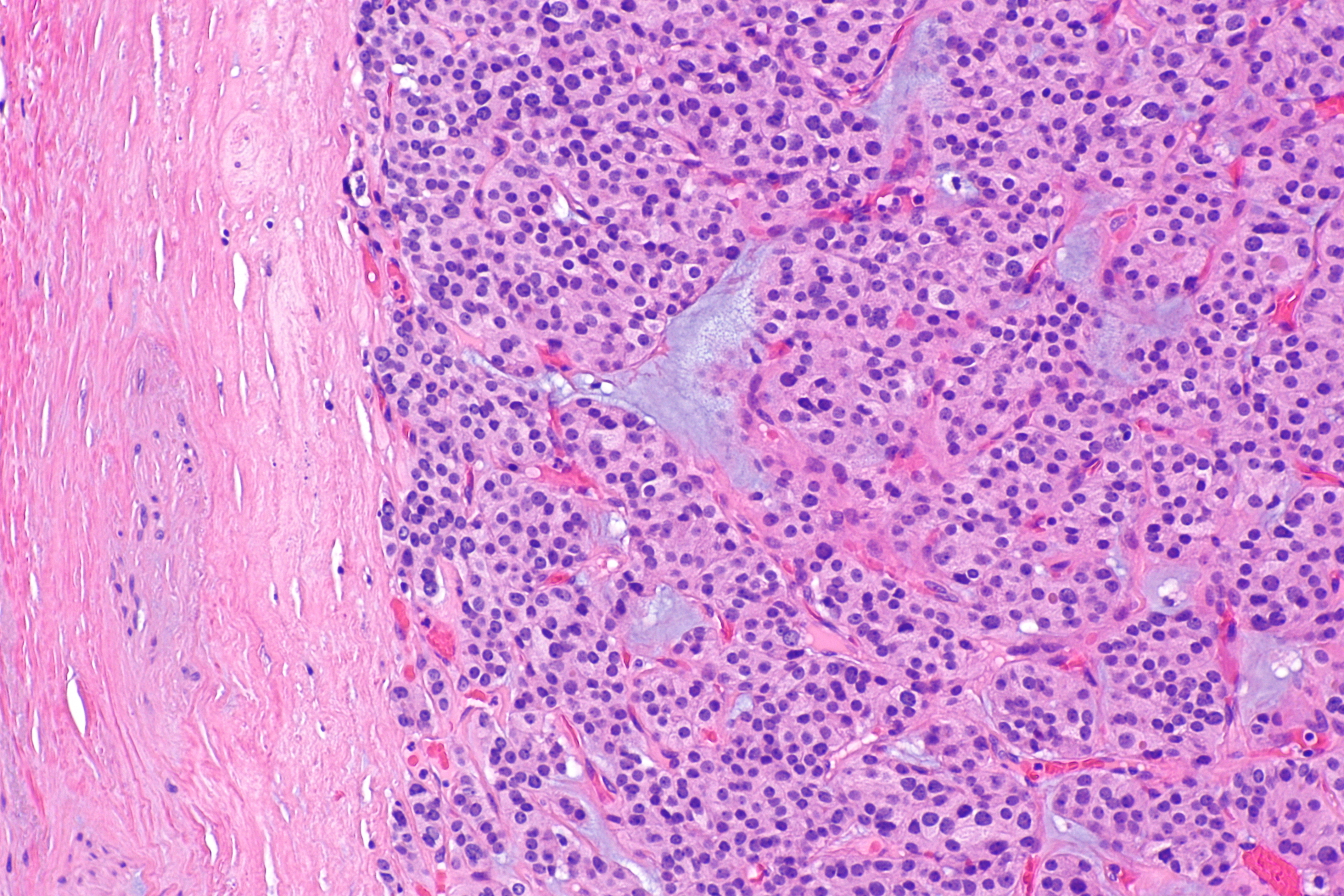
* Undifferentiated, devastatingly aggressive variant of [[Papillary thyroid cancer|papillary]]/[[follicular thyroid cancer]] | |||
| style="padding: 5px 5px; background: #F5F5F5;" align="left" | | |||
* Normal [[thyroid function test|thyroid function tests]] | |||
| style="padding: 5px 5px; background: #F5F5F5;" align="left" | | |||
* Poor [[prognosis]] | |||
* May be associated with [[TP53]] [[mutation]] | |||
| style="padding: 5px 5px; background: #F5F5F5;" align="left" |[[File:Anaplastic thyroid carcinoma low mag.jpg|thumb|none|200px|Source:Wikimedia common ]] | |||
|- | |||
! style="padding: 5px 5px; background: #DCDCDC;" align="left" |Follicular Adenoma<ref name="MathurOlson2014">{{cite journal|last1=Mathur|first1=Aarti|last2=Olson|first2=Matthew T.|last3=Zeiger|first3=Martha A.|title=Follicular Lesions of the Thyroid|journal=Surgical Clinics of North America|volume=94|issue=3|year=2014|pages=499–513|issn=00396109|doi=10.1016/j.suc.2014.02.005}}</ref> | |||
| style="padding: 5px 5px; background: #F5F5F5;" align="left" | | |||
* More commonly affects individuals older than 50 years of age | |||
| style="padding: 5px 5px; background: #F5F5F5;" align="left" | | |||
* More commonly affects women | |||
| style="padding: 5px 5px; background: #F5F5F5;" align="left" | | |||
*[[Asymptomatic]] or [[symptoms]] of [[hyperthyroidism]] | |||
| style="padding: 5px 5px; background: #F5F5F5;" align="left" | | |||
* Solitary [[nodule]] which may show echogenicity or not | |||
| style="padding: 5px 5px; background: #F5F5F5;" align="left" | | |||
* Solitary, spherical, and encapsulated [[lesion]] | |||
* Well demarcated from the surrounding [[parenchyma]] | |||
| style="padding: 5px 5px; background: #F5F5F5;" align="left" | | |||
* Uniform [[Follicle|follicles]] | |||
* Absence of capsular or [[vascular]] invasion | |||
| style="padding: 5px 5px; background: #F5F5F5;" align="left" | | |||
* Functional [[adenoma]]: | |||
** Elevated T3, T4 | |||
** Decreased TSH | |||
| style="padding: 5px 5px; background: #F5F5F5;" align="left" | | |||
* May be considered functional or hot | |||
* May be considered non-functional or cold | |||
| style="padding: 5px 5px; background: #F5F5F5;" align="left" |[[File:Follicular adenoma -- intermed mag.jpg|thumb|none|200px|Source:Wikimedia common ]] | |||
|- | |||
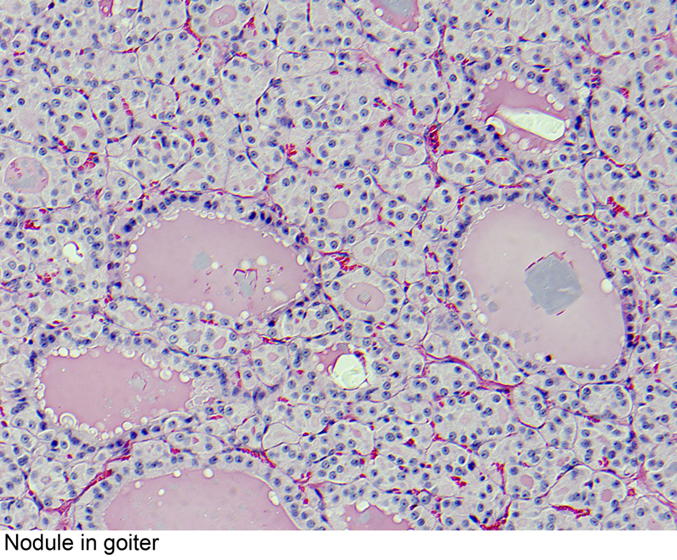
! style="padding: 5px 5px; background: #DCDCDC;" align="left" |Multinodular Goiter<ref name="pmid8197088">{{cite journal |vauthors=Bronshteĭn ME, Makarov AD, Artemova AM, Bazarova EN, Kozlov GI |title=[Morphology of the thyroid tissue in multinodular euthyroid goiter] |language=Russian |journal=Probl Endokrinol (Mosk) |volume=40 |issue=2 |pages=36–9 |date=1994 |pmid=8197088 |doi= |url=}}</ref> | |||
| style="padding: 5px 5px; background: #F5F5F5;" align="left" | | |||
* Commonly affects individuals older than 60 years of age | |||
| style="padding: 5px 5px; background: #F5F5F5;" align="left" | | |||
* More commonly affects women | |||
| style="padding: 5px 5px; background: #F5F5F5;" align="left" | | |||
*[[Thyroid]] enlargement | |||
*[[Signs]]/[[symptoms]] of [[Hypothyroidism|hypo]]/[[hyperthyroidism]] | |||
| style="padding: 5px 5px; background: #F5F5F5;" align="left" | | |||
* Multiple [[nodules]] with different echogenicity | |||
*[[Calcification]] may be present | |||
| style="padding: 5px 5px; background: #F5F5F5;" align="left" | | |||
* Multiple [[Thyroid nodule|thyroid nodules]] | |||
| style="padding: 5px 5px; background: #F5F5F5;" align="left" | | |||
* Variable sized [[Follicle|follicles]] | |||
* Some may show [[papillary]] [[Projection areas|projections]] without [[nuclear]] characteristics of [[papillary thyroid cancer]] | |||
| style="padding: 5px 5px; background: #F5F5F5;" align="left" | | |||
*[[Classification|Classified]] as toxic and non-toxic | |||
**'''Toxic:''' [[Hyperthyroidism]] | |||
**'''Non-toxic:''' Normal [[thyroid function test|thyroid function tests]] | |||
| style="padding: 5px 5px; background: #F5F5F5;" align="left" | | |||
*[[Benign]] [[condition]] | |||
| style="padding: 5px 5px; background: #F5F5F5;" align="left" |[[File:ThyroidnodularSatturwar08.jpg|thumb|none|200px|Source:pathology outline, case courtesy of Dr. Swati Satturwar]] | |||
|- | |||
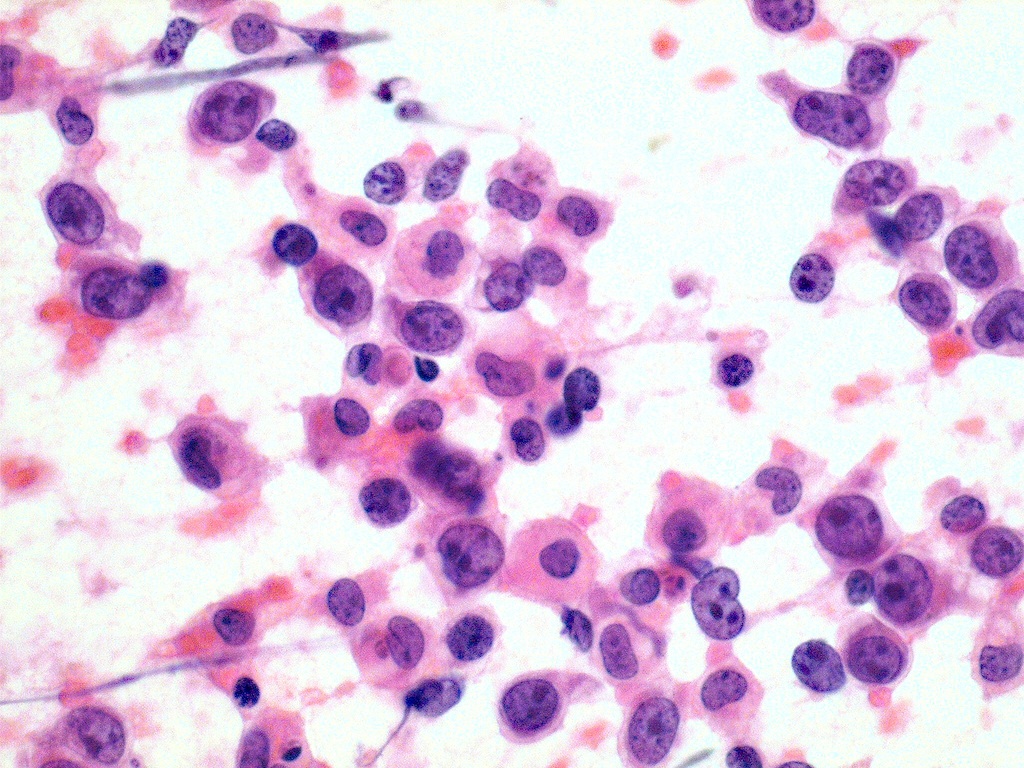
! style="padding: 5px 5px; background: #DCDCDC; " align="left" |Thyroid Lymphoma<ref name="pmid8838117">{{cite journal |vauthors=Pedersen RK, Pedersen NT |title=Primary non-Hodgkin's lymphoma of the thyroid gland: a population based study |journal=Histopathology |volume=28 |issue=1 |pages=25–32 |date=January 1996 |pmid=8838117 |doi= |url=}}</ref> | |||
<ref name="pmid3141260">{{cite journal |vauthors=Hyjek E, Isaacson PG |title=Primary B cell lymphoma of the thyroid and its relationship to Hashimoto's thyroiditis |journal=Hum. Pathol. |volume=19 |issue=11 |pages=1315–26 |date=November 1988 |pmid=3141260 |doi=10.1016/s0046-8177(88)80287-9 |url=}}</ref><ref name="pmid3759532">{{cite journal |vauthors=Tupchong L, Hughes F, Harmer CL |title=Primary lymphoma of the thyroid: clinical features, prognostic factors, and results of treatment |journal=Int. J. Radiat. Oncol. Biol. Phys. |volume=12 |issue=10 |pages=1813–21 |date=October 1986 |pmid=3759532 |doi=10.1016/0360-3016(86)90324-x |url=}}</ref><ref name="pmid17042683">{{cite journal |vauthors=Ota H, Ito Y, Matsuzuka F, Kuma S, Fukata S, Morita S, Kobayashi K, Nakamura Y, Kakudo K, Amino N, Miyauchi A |title=Usefulness of ultrasonography for diagnosis of malignant lymphoma of the thyroid |journal=Thyroid |volume=16 |issue=10 |pages=983–7 |date=October 2006 |pmid=17042683 |doi=10.1089/thy.2006.16.983 |url=}}</ref> | |||
| style="padding: 5px 5px; background: #F5F5F5;" align="left" | | |||
* Affects [[Adult|adults]] or elderly | |||
| style="padding: 5px 5px; background: #F5F5F5;" align="left" | | |||
* More common among women | |||
| style="padding: 5px 5px; background: #F5F5F5;" align="left" | | |||
* Rapidly enlarging mass/[[nodule]] of [[thyroid]] | |||
* Compressive [[symptoms]] may be present | |||
* [[B symptoms|Constitiutional symptoms]] can be present in 10% | |||
*[[Physical examination|P/E]]:Firm, hard [[thyroid]] | |||
* Fixed to the nearby structures | |||
* Immobile even during swallowing | |||
* [[Cervical]] or [[supraclavicular]] [[lymphadenopathy]] may be present | |||
| style="padding: 5px 5px; background: #F5F5F5;" align="left" | | |||
* On [[ultrasound]]: | |||
**Hypoechogenic appearance | |||
**Difficult to distinguish from [[Chronic (medical)|chronic]] [[thyroiditis]] | |||
| style="padding: 5px 5px; background: #F5F5F5;" align="left" | | |||
* [[Thyroid nodule]]/mass | |||
== | *Fixed to adjacent [[tissue]] | ||
*Firm texture | |||
| style="padding: 5px 5px; background: #F5F5F5;" align="left" | | |||
* It is of [[B cell]] lineage in the majority of cases | |||
* Dffuse, large [[B-cell lymphoma|B-cell lymphomas]] is the most common subtype | |||
* [[Marginal zone lymphoma]] is the second most common type | |||
| style="padding: 5px 5px; background: #F5F5F5;" align="left" | | |||
* No specific test | |||
* Some [[Patient|patients]] may have [[hypothyroidism]] | |||
*[[Patient|Patients]] can also have [[antibody|antibodies]] against [[thyroid peroxidase]] or [[thyroglobulin]] | |||
| style="padding: 5px 5px; background: #F5F5F5;" align="left" | | |||
* Preexisting [[Chronic (medical)|chronic]] [[Hashimoto's thyroiditis|autoimmune (Hashimoto's) thyroiditis]] is a known [[risk factor]] for this [[condition]] | |||
| style="padding: 5px 5px; background: #F5F5F5;" align="left" |[[File:Thyroid lymphoma large cell type fine needle aspiration biop.jpeg|thumb|none|200px|Source:pathology outline, case courtesy of Dr. Mark R. Wick]] | |||
|} | |||
# | |||
= | |||
==References== | ==References== | ||
{{Reflist|2}} | |||
| | |||
[[Category:Endocrinology]] | |||
[[Category:Oncology]] | |||
{{ | {{WH}} | ||
{{ | {{WS}} | ||
Latest revision as of 15:19, 26 September 2019
|
Thyroid Cancer Main Page |
Editor-In-Chief: C. Michael Gibson, M.S., M.D. [1]; Associate Editor(s)-in-Chief: Michael Maddaleni, B.S.; Ammu Susheela, M.D. [2]Seyedmahdi Pahlavani, M.D. [3] Sahar Memar Montazerin, M.D.[4]
Overview
Thyroid cancer refers to any of four kinds of tumors of the thyroid gland which include papillary, follicular, medullary and anaplastic tumors. Papillary and follicular tumors are the most common and are usually benign. Papillary and follicular tumors have a slow growth and may recur, but are generally not fatal in patients under 45 years of age. Medullary and anaplastic tumors are malignant. Medullary tumors have a good prognosis if the are restricted to the thyroid gland and a poorer prognosis if metastasis occurs. Anaplastic tumors are fast-growing and respond poorly to therapy. Thyroid nodules are diagnosed by ultrasound guided fine needle aspiration or frequently by thyroidectomy (surgical removal and subsequent histological examination). As the thyroid cancer can uptake iodine, radioactive iodine is commonly used for the treatment of thyroid carcinomas. However, radioactive iodine therapy is accompanied by thyroxine therapy to ensure TSH suppression.
Classification
Thyroid cancers can be classified according to their pathological characteristics. The following variants can be distinguished (distribution over various subtypes may show regional variation):
- Papillary thyroid cancer (75%, including mixed papillary/follicular)
- Follicular thyroid cancer (16%)
- Medullary thyroid cancer (5-7%)
- Anaplastic thyroid cancer (3%)
- Lymphoma (1%)
| |||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
Causes
- For more information on papillary thyroid cancer causes, click here.
- For more information on follicular thyroid cancer causes, click here.
- For more information on medullary thyroid cancer causes, click here.
- For more information on anaplastic thyroid cancer causes, click here.
- For more information on primary thyroid lymphoma causes, click here.
Differential diagnosis
Thyroid cancers should be differentiated from one another and from various other diseases:
| Disease Name | Age of Onset | Gender Preponderance | Signs/Symptoms | Imaging Feature(s) | Macroscopic Feature(s) | Microscopic Feature(s) | Laboratory Findings(s) | Other Feature(s) | Microscopic Appearance |
|---|---|---|---|---|---|---|---|---|---|
| Papillary Thyroid Cancer[1][2][3] |
|
|
|
|
|
|
|
 | |
| Follicular Thyroid Cancer[2][3][4] |
|
|
|
|
|
|
|
|
 |
| Medullary Thyroid Cancer[5][6][7][3] |
|
|
|
|
|
|
|
 | |
| Anaplastic Thyroid Cancer[8][9][10] |
|
|
|
|
|
|
 | ||
| Follicular Adenoma[11] |
|
|
|
|
|
|
 | ||
| Multinodular Goiter[12] |
|
|
|
|
|
|
|
 | |
| Thyroid Lymphoma[13] |
|
|
|
|
|
|
|
|
 |
References
- ↑ Fagin, James A.; Mitsiades, Nicholas (2008). "Molecular pathology of thyroid cancer: diagnostic and clinical implications". Best Practice & Research Clinical Endocrinology & Metabolism. 22 (6): 955–969. doi:10.1016/j.beem.2008.09.017. ISSN 1521-690X.
- ↑ 2.0 2.1 Schlumberger, Martin Jean (1998). "Papillary and Follicular Thyroid Carcinoma". New England Journal of Medicine. 338 (5): 297–306. doi:10.1056/NEJM199801293380506. ISSN 0028-4793.
- ↑ 3.0 3.1 3.2 Sipos JA (December 2009). "Advances in ultrasound for the diagnosis and management of thyroid cancer". Thyroid. 19 (12): 1363–72. doi:10.1089/thy.2009.1608. PMID 20001718.
- ↑ Pettersson B, Adami HO, Wilander E, Coleman MP (April 1991). "Trends in thyroid cancer incidence in Sweden, 1958-1981, by histopathologic type". Int. J. Cancer. 48 (1): 28–33. doi:10.1002/ijc.2910480106. PMID 2019455.
- ↑ Busnardo B, Girelli ME, Simioni N, Nacamulli D, Busetto E (January 1984). "Nonparallel patterns of calcitonin and carcinoembryonic antigen levels in the follow-up of medullary thyroid carcinoma". Cancer. 53 (2): 278–85. doi:10.1002/1097-0142(19840115)53:2<278::aid-cncr2820530216>3.0.co;2-z. PMID 6690009.
- ↑ Kebebew E, Ituarte PH, Siperstein AE, Duh QY, Clark OH (March 2000). "Medullary thyroid carcinoma: clinical characteristics, treatment, prognostic factors, and a comparison of staging systems". Cancer. 88 (5): 1139–48. doi:10.1002/(sici)1097-0142(20000301)88:5<1139::aid-cncr26>3.0.co;2-z. PMID 10699905.
- ↑ Hofstra, Robert M. W.; Landsvater, Rudy M.; Ceccherini, Isabella; Stulp, Rein P.; Stelwagen, Tineke; Luo, Yin; Pasini, Barbara; Hoppener, Jo W. M.; van Amstel, Hans Kristian Ploos; Romeo, Giovanni; Lips, Cornells J. M.; Buys, Charles H. C. M. (1994). "A mutation in the RET proto-oncogene associated with multiple endocrine neoplasia type 2B and sporadic medullary thyroid carcinoma". Nature. 367 (6461): 375–376. doi:10.1038/367375a0. ISSN 0028-0836.
- ↑ Nagaiah G, Hossain A, Mooney CJ, Parmentier J, Remick SC (2011). "Anaplastic thyroid cancer: a review of epidemiology, pathogenesis, and treatment". J Oncol. 2011: 542358. doi:10.1155/2011/542358. PMC 3136148. PMID 21772843.
- ↑ Chang TC, Liaw KY, Kuo SH, Chang CC, Chen FW (June 1989). "Anaplastic thyroid carcinoma: review of 24 cases, with emphasis on cytodiagnosis and leukocytosis". Taiwan Yi Xue Hui Za Zhi. 88 (6): 551–6. PMID 2794956.
- ↑ Venkatesh YS, Ordonez NG, Schultz PN, Hickey RC, Goepfert H, Samaan NA (July 1990). "Anaplastic carcinoma of the thyroid. A clinicopathologic study of 121 cases". Cancer. 66 (2): 321–30. doi:10.1002/1097-0142(19900715)66:2<321::aid-cncr2820660221>3.0.co;2-a. PMID 1695118.
- ↑ Mathur, Aarti; Olson, Matthew T.; Zeiger, Martha A. (2014). "Follicular Lesions of the Thyroid". Surgical Clinics of North America. 94 (3): 499–513. doi:10.1016/j.suc.2014.02.005. ISSN 0039-6109.
- ↑ Bronshteĭn ME, Makarov AD, Artemova AM, Bazarova EN, Kozlov GI (1994). "[Morphology of the thyroid tissue in multinodular euthyroid goiter]". Probl Endokrinol (Mosk) (in Russian). 40 (2): 36–9. PMID 8197088.
- ↑ Pedersen RK, Pedersen NT (January 1996). "Primary non-Hodgkin's lymphoma of the thyroid gland: a population based study". Histopathology. 28 (1): 25–32. PMID 8838117.
- ↑ Hyjek E, Isaacson PG (November 1988). "Primary B cell lymphoma of the thyroid and its relationship to Hashimoto's thyroiditis". Hum. Pathol. 19 (11): 1315–26. doi:10.1016/s0046-8177(88)80287-9. PMID 3141260.
- ↑ Tupchong L, Hughes F, Harmer CL (October 1986). "Primary lymphoma of the thyroid: clinical features, prognostic factors, and results of treatment". Int. J. Radiat. Oncol. Biol. Phys. 12 (10): 1813–21. doi:10.1016/0360-3016(86)90324-x. PMID 3759532.
- ↑ Ota H, Ito Y, Matsuzuka F, Kuma S, Fukata S, Morita S, Kobayashi K, Nakamura Y, Kakudo K, Amino N, Miyauchi A (October 2006). "Usefulness of ultrasonography for diagnosis of malignant lymphoma of the thyroid". Thyroid. 16 (10): 983–7. doi:10.1089/thy.2006.16.983. PMID 17042683.