Thyroid adenoma pathophysiology: Difference between revisions
No edit summary |
No edit summary |
||
| Line 31: | Line 31: | ||
==Reference== | ==Reference== | ||
{{Reflist|2}} | {{Reflist|2}} | ||
[[Category:Disease]] | |||
[[Category:Endocrinology]] | |||
Revision as of 05:11, 12 October 2015
|
Thyroid adenoma Microchapters |
|
Diagnosis |
|---|
|
Treatment |
|
Case Studies |
|
Thyroid adenoma pathophysiology On the Web |
|
American Roentgen Ray Society Images of Thyroid adenoma pathophysiology |
|
Risk calculators and risk factors for Thyroid adenoma pathophysiology |
Editor-In-Chief: C. Michael Gibson, M.S., M.D. [1]; Associate Editor(s)-in-Chief: Ammu Susheela, M.D. [2]
Overview
Pathogenesis
A thyroid adenoma may be clinically silent, or it may be a "functional" tumor, producing excessive thyroid hormone. In this case, it may result in symptomatic hyperthyroidism, and may be referred to as a toxic thyroid adenoma. Careful pathological examination may be necessary to distinguish a thyroid adenoma from a minimally invasive follicular thyroid carcinoma.
Colloid Nodules
Colloid nodules (CN) are non-neoplastic benign nodules occurring within the thyroid gland. They form the vast majority of nodular thyroid disease. Colloid nodules are composed of irregularly enlarged follicles containing abundant colloid. Some colloid nodules can be cystic (cystic colloid nodule), and may contain areas of necrosis, haemorrhage and/or calcification. Colloid nodule may be single or multiple and can vary considerably in size.[1]
Genetics
Associated Conditions
Gross Pathology
Thyroid follicular adenoma ranges in diameter from 3 cm on an average, but sometimes is larger (up to 10 cm) or smaller. The typical thyroid adenoma is solitary, spherical and encapsulated lesion that is well demarcated from the surrounding parenchyma. The color ranges from gray-white to red-brown, depending upon
- the cellularity of the adenoma
- the colloid content.
-
ADRENAL GLAND: BILATERAL PHEOCHROMOCYTOMA Cross section of bilateral pheochromocytomas from a 30-year-old man with MEN syndrome type IIa. The right adrenal tumor weighed 168 g and the left 220 g. Note the distinct multinodular, multicentric pattern of growth on both sides
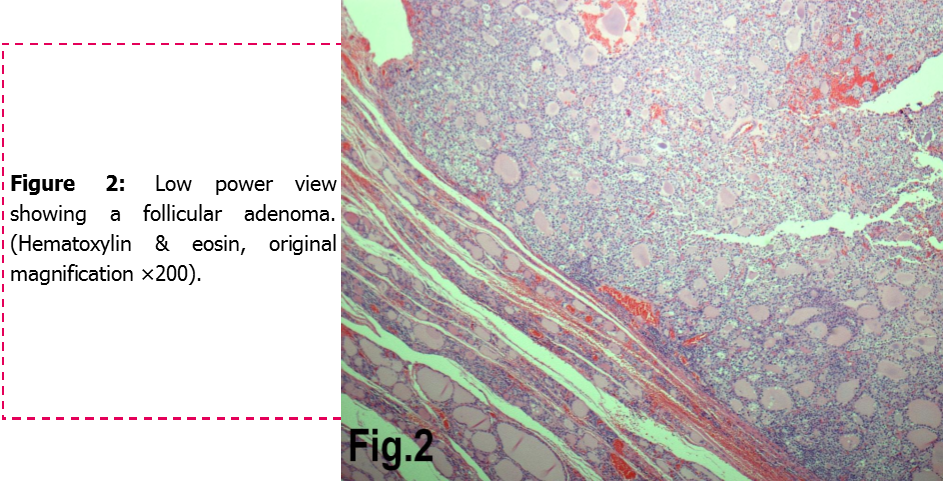
Microscopic Pathology
- Areas of hemorrhage, fibrosis, calcification, and cystic change, similar to what is found in multinodular goiters, are common in thyroid (follicular) adenoma, particularly in larger lesions.
- Encapsulated tumors without evidence of infiltration
-
Follicular Adenoma of the Thyroid Gland
Histopathological Video
Video
{{#ev:youtube|iVANfjos88Q}}
Reference
- ↑ Colloid nodule (thyroid). Radiopedia 2015. http://radiopaedia.org/articles/colloid-nodule-thyroid-1 Accessed on October,7, 2015