Thyroid adenoma pathophysiology
|
Thyroid adenoma Microchapters |
|
Diagnosis |
|---|
|
Treatment |
|
Case Studies |
|
Thyroid adenoma pathophysiology On the Web |
|
American Roentgen Ray Society Images of Thyroid adenoma pathophysiology |
|
Risk calculators and risk factors for Thyroid adenoma pathophysiology |
Editor-In-Chief: C. Michael Gibson, M.S., M.D. [3]; Associate Editor(s)-in-Chief: Ammu Susheela, M.D. [4]
Overview
Thyroid adenoma arises from epithelial cells of thyroid gland, that are normally involved in secretion of thyroxine hormone. The most common gene involved in the pathogenesis of thyroid adenoma is THADA gene.
Pathogenesis
Thyroid adenoma are lumps which commonly arise within an otherwise normal thyroid gland.[1] They indicate a thyroid neoplasm.
- Sometimes a thyroid nodule presents as a fluid-filled cavity called a thyroid cyst. Often, solid components are mixed with the fluid. Thyroid cysts most commonly result from degenerating thyroid adenomas, which are benign, but they occasionally contain malignant solid components.[2]
- A thyroid adenoma may be clinically silent, or it may be a "functional" tumor, producing excessive thyroid hormone. In this case, it may result in symptomatic hyperthyroidism, and may be referred to as a toxic thyroid adenoma.
Colloid Nodules
Colloid nodules are non-neoplastic benign nodules occurring within the thyroid gland. They form the vast majority of nodular thyroid disease. Colloid nodules are composed of irregularly enlarged follicles containing abundant colloid. Some colloid nodules can be cystic (cystic colloid nodule), and may contain areas of necrosis, hemorrhage, and calcification. Colloid nodule may be single or multiple and can vary considerably in size.[3]
Genetics
- The target gene associated with thyroid adenoma has been identified and referred to as thyroid adenoma associated (THADA) gene.[4][5]
- In thyroid adenomas, protein associated with THADA was frequently found to be truncated.
- While competing with the full-length protein translated from the normal allele of THADA the altered protein derived from the truncated gene might lead to an impaired induction of apoptosis, and subsequently give rise to an increased cell proliferation leading to benign thyroid tumors with 2p21 translocations, without significant changes of the expression level.
Associated Conditions
Gross Pathology
Thyroid follicular adenoma ranges in diameter from 3 cm on an average, but sometimes is larger (up to 10 cm) or smaller. The typical thyroid adenoma is solitary, spherical and encapsulated lesion that is well demarcated from the surrounding parenchyma. The color ranges from gray-white to red-brown, depending upon
- The cellularity of the adenoma
- The colloid content
-
Follicular Adenoma of the Thyroid Gland
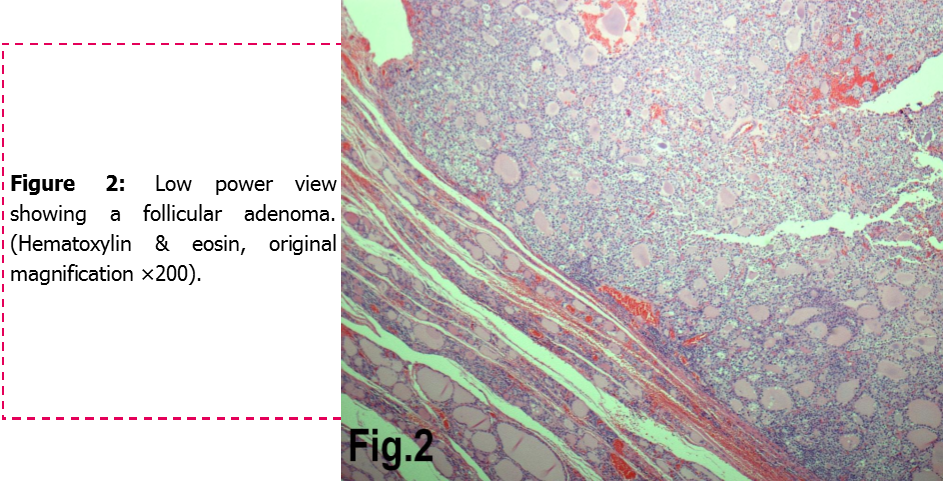
Microscopic Pathology
- Areas of hemorrhage, fibrosis, calcification, and cystic change, similar to what is found in multinodular goiters, are common in thyroid (follicular) adenoma, particularly in larger lesions.
- Encapsulated tumors without evidence of infiltration
- Colloid nodules are distinguished by an apparently gelatinous mass of colloid both surrounding and contained within follicular cells. Colloid nodules are not surrounded by a fibrous capsule of compressed tissue. However, they are surrounded by flattened epithelial cells.[6] Both the number of cells and the type of colloid may vary considerably.[7]
-
Follicular adenoma of the thyroid gland
-
Histology of the encapsulated tumor. (a) Photomicrograph showing an encapsulated tumor composed of cells arranged in microfollicular, glandular and trabecular patterns (hematoxylin and eosin; 100×). (b) High power photomicrograph showing the microfollicles containing inspissated colloid resembling hyaline globules and separated by eosinophilic extracellular hyaline material. (hematoxylin and eosin; 100×).[8]
Histopathological Video
Video
{{#ev:youtube|iVANfjos88Q}}
Reference
- ↑ "New York Thyroid Center: Thyroid Nodules".
- ↑ mayoclinic.com > Thyroid nodules Feb. 22, 2011
- ↑ Colloid nodule (thyroid). Radiopedia 2015. http://radiopaedia.org/articles/colloid-nodule-thyroid-1 Accessed on October,7, 2015
- ↑ Rippe V, Drieschner N, Meiboom M, Murua Escobar H, Bonk U, Belge G; et al. (2003). "Identification of a gene rearranged by 2p21 aberrations in thyroid adenomas". Oncogene. 22 (38): 6111–4. doi:10.1038/sj.onc.1206867. PMID 12955091.
- ↑ Kloth, Lars; Belge, Gazanfer; Burchardt, Käte; Loeschke, Siegfried; Wosniok, Werner; Fu, Xin; Nimzyk, Rolf; Mohamed, Salah A; Drieschner, Norbert; Rippe, Volkhard; Bullerdiek, Jörn (2011). "Decrease in thyroid adenoma associated (THADA) expression is a marker of dedifferentiation of thyroid tissue". BMC Clinical Pathology. 11 (1): 13. doi:10.1186/1472-6890-11-13. ISSN 1472-6890.
- ↑ Dr. Alpha Tsui (10 October 2010). "Thyroid cytology" (PDF). thyroidmanager.org. Retrieved 26 September 2011.
- ↑ Diana S. Dean, M.D. Hossein Gharib, M.D. (10 October 2010). "Fine-Needle Aspiration Biopsy of the Thyroid Gland, Chapter 6d". thyroidmanager.org. Retrieved 26 September 2011.
- ↑ Image courtesy of Dr Frank Gaillard. [1] (original file[2]).Creative Commons BY-SA-NC