Thalassemia laboratory findings
|
Thalassemia Microchapters |
|
Diagnosis |
|---|
|
Treatment |
|
Case Studies |
|
Thalassemia laboratory findings On the Web |
|
American Roentgen Ray Society Images of Thalassemia laboratory findings |
|
Risk calculators and risk factors for Thalassemia laboratory findings |
Please help WikiDoc by adding more content here. It's easy! Click here to learn about editing.
Editor-In-Chief: C. Michael Gibson, M.S., M.D. [1]
Overview
Laboratory Findings
- Low hemoglobin: Low hemoglobin, or anemia, is always found in patients with thalassemia. This is a defining and required laboratory feature of all thalassmias.
- Elevated red blood cell mass: This is a somewhat unique feature of thalassemia. A low hemoglobin plus elevated red blood cell mass should prompt a clinician to consider thalassemia as the cause of anemia. In contrast, patients with iron-deficiency anemia have low hemoglobin but do not have elevated red blood cell mass.
- Elevated lactate dehydrogenase (LDH): This is due to hemolysis, in which intracellular contents (such as LDH) are released into the circulation.
- Indirect, or unconjugated, hyperbilirubinemia: This is due to hemolysis, in which breaskdown products of heme are released into the bloodstream.
- Low haptoglobin: This is due to hemolysis, in which free hemoglobin in the circulation binds to and reduces the level of haptoglobin.
- Elevated reticulocyte count: This is due to a bone marrow compensatory response to low hemoglobin levels from thalassemia. Reticulocytes are precursors of red blood cells and thus an elevated reticulocyte count signifies an adequate compensatory attempt to produce more red blood cells.
- Abnormal bands on hemoglobin electrophoresis: Hemoglobin electrophoresis is the gold standard diagnostic test for thalassemia. In normal persons, a hemoglobin electrophoresis will show a strong band corresponding to hemoglobin A (tetramer of 2 alpha-globin chains and 2 beta-globin chains) and a weak band corresponding to hemoglobin A2 (tetramer of 2 alpha-globin chains and 2 delta-globin chains). In thalassemia, various other bands can be present on electrophoresis. These include tetramers of gamma-globin chains (such as in Hb Barts) or tetramers of beta-globin chains (such as in HbH disease).
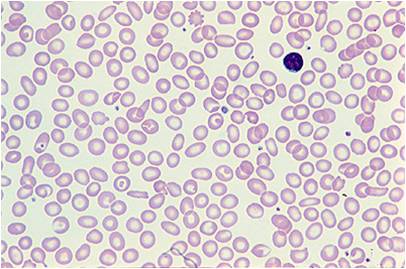
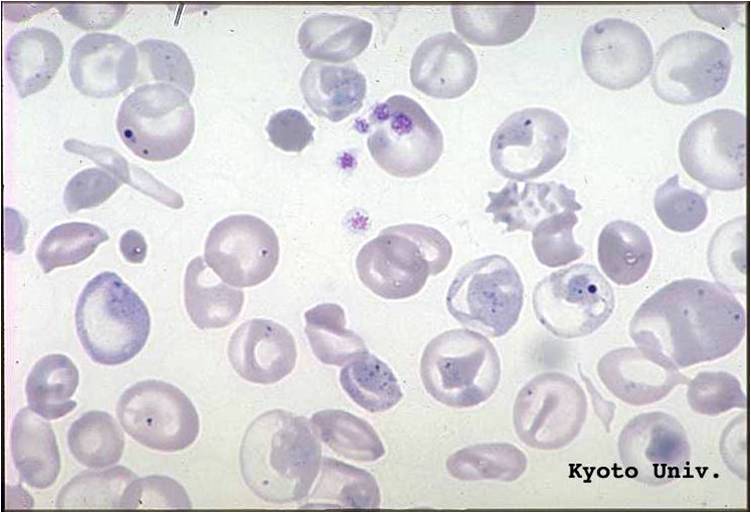
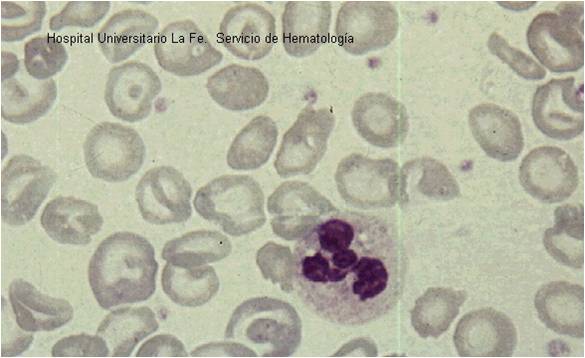
Peripheral Smear
(Images shown below are courtesy of Melih Aktan MD, Istanbul Medical Faculty - Turkey, and Kyoto University - Japan, and Hospital Universitario La Fe Servicio Hematologia)