Tension pneumothorax resident survival guide: Difference between revisions
Rim Halaby (talk | contribs) |
Rim Halaby (talk | contribs) |
||
| Line 83: | Line 83: | ||
❑ Recent invasive procedures<br> | ❑ Recent invasive procedures<br> | ||
:❑ [[Thoracentesis]]<br> | :❑ [[Thoracentesis]]<br> | ||
:❑ [[Central venous catheter]] | :❑ [[Central venous catheter]] <br> | ||
:❑ [[Bronchoscopy]]<br> | :❑ [[Bronchoscopy]]<br> | ||
:❑ [[Biopsy|Pleural biopsy]]<br> | :❑ [[Biopsy|Pleural biopsy]]<br> | ||
| Line 114: | Line 114: | ||
'''Inspection'''<BR> | '''Inspection'''<BR> | ||
❑ Enlargement of the involved side <BR> | ❑ Enlargement of the involved side of the chest <BR> | ||
❑ [[Intercostal space]] widening on the affected side<br> | ❑ [[Intercostal space]] widening on the affected side<br> | ||
'''Palpation'''<BR> | '''Palpation'''<BR> | ||
Revision as of 14:50, 5 April 2014
Editor-In-Chief: C. Michael Gibson, M.S., M.D. [1]; Associate Editor(s)-in-Chief: Mohamed Moubarak, M.D. [2]; Twinkle Singh, M.B.B.S. [3]
Synonyms and keywords: Collapsed lung; air around the lung; air outside the lung
| Tension Pneumothorax Resident Survival Guide Microchapters |
|---|
| Overview |
| Causes |
| FIRE |
| Diagnosis |
| Treatment |
| Do's |
| Don'ts |
Overview
Tension pneumothorax is a life threatening condition that results from the accumulation of air in the pleural cavity. Air enters the intrapleural space as a result of the disruption in the parietal pleura, visceral pleura or tracheobronchial tree. This disruption leads to the formation of a one way valve which allows the air to enter in the pleural cavity (during inspiration) but prevents its escape (during expiration). Subsequently, pressure inside the pleural cavity rises above the atmospheric pressure and results in respiratory and cardiovascular failure. Tension pneumothorax can occur as a result of trauma, ventilation or resuscitation.[1] The cardinal symptoms and signs of tension pneumothorax are severe dyspnea, chest pain, hypotension, hypoxia, tachycardia and jugular vein distention. Tension pneumothorax should be managed immediately with emergency needle decompression followed by insertion of a chest tube.
Causes
Life Threatening Causes
Tension pneumothorax is a life-threatening condition and must be treated as such irrespective of the underlying cause.
Common Causes
- Asthma
- Central venous catheter
- Cardiopulmonary resuscitation
- Chronic obstructive pulmonary disease
- Emphysema
- Mechanical ventilation
- Trauma[1]
Click here for the complete list of causes.
FIRE: Focused Initial Rapid Evaluation
The aim of FIRE is to identify urgent conditions that require immediate intervention in suspected tension pneumothorax.[1]
Boxes in red signify that an urgent management is needed.
Identify cardinal findings that increase the pretest probability of tension pneumothorax: ❑ Chest pain ❑ Dyspnea ❑ Hypoxia ❑ Hypotension ❑ Tachycardia ❑ Jugular venous distension ❑ Absent breath sounds on the affected side | |||||||||||||||||||||||||||||||||||||||||
❑ High probability of tension pneumothorax | ❑ Low probability of tension pneumothorax and patient is hemodynamically stable | ||||||||||||||||||||||||||||||||||||||||
❑ Proceed with immediate needle decompression in the 2nd intercostal space at the midclavicular line of the affected hemithorax | |||||||||||||||||||||||||||||||||||||||||
❑ Insert chest drain immediately after needle decompression | |||||||||||||||||||||||||||||||||||||||||
Complete Diagnostic Approach
Shown below is an algorithm depicting the diagnostic approach to tension pneumothorax based on the 2010 British Thoracic Society Pleural Disease Guideline. Tension pneumothorax requires immediate intervention. It should be diagnosed based on the history and physical examination findings. [1]
Abberviations: DVT: Deep venous thrombosis; CT: Computed tomography
Characterize the symptoms: ❑ Dyspnea | |||||||||||||||||||||||||||
Identify the precipitating factors: ❑ Recent invasive procedures ❑ Mechanical ventilation | |||||||||||||||||||||||||||
Examine the patient: Appearance of the patient Vital signs ❑ Tachycardia Skin ❑ Cyanosis Neck ❑ Jugular venous distension (absent in severe hypotension) Respiratory examination: Inspection Additional findings in ventilated patients: ❑ Decreased oxygen saturation | |||||||||||||||||||||||||||
Consider alternative diagnosis:
| |||||||||||||||||||||||||||
| ❑ High probability of tension pneumothorax | ❑ Low probability of tension pneumothorax and patient is hemodynamically stable | ||||||||||||||||||||||||||
| ❑ Proceed with immediate needle decompression | |||||||||||||||||||||||||||
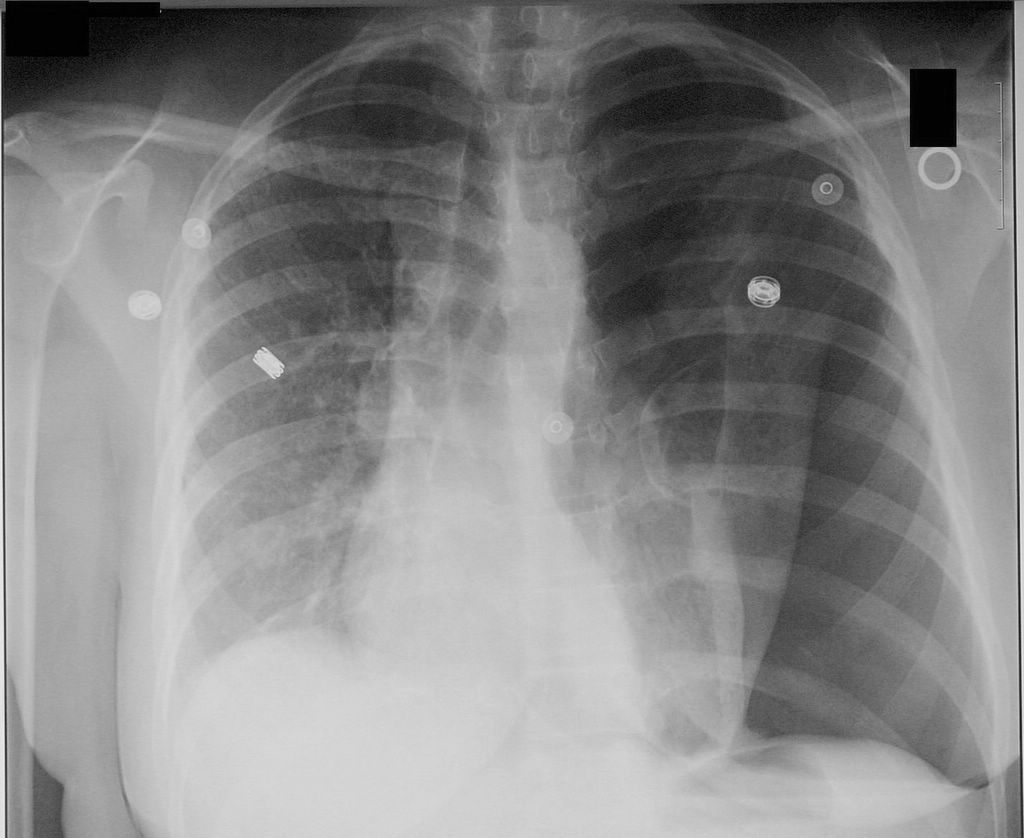
Order imaging studies: ❑ Order chest X-ray looking for:
| |||||||||||||||||||||||||||
Treatment
Perform emergency needle decompression:[1] ❑ Wear a gown, face mask and eye shield
Don't remove the catheter, until the chest drain is inserted and is functioning properly. | |||||||||||||||||||||||||||||||||||||
Insert a chest drain immediately after needle decompression: ❑ Make sure that the following equipments are available:
❑ Administer adequate analgesics | |||||||||||||||||||||||||||||||||||||
Follow up: ❑ Make sure the patient is followed up by a chest physician | |||||||||||||||||||||||||||||||||||||
Do's
- Suspect tension pneumothorax with blunt and penetrating trauma to the chest.
- Immediately cover penetrating chest wounds with an occlusive or pressure bandage in trauma patients with tension pneumothorax.
- Suspect tension pneumothorax among patients on mechanical ventilation who develop a rapid onset of hemodynamic instability or cardiac arrest and require an increase in the peak inspiratory pressure.
- Order serial chest radiographs every 6 hours on the first day following chest trauma to rule out pneumothorax.[2]
- Administer adequate analgesia to patients before chest tube insertion because the procedure is extremely painful.
- Refer the patient to a respiratory specialist within 24 hours of admission.
- Order a chest X-ray before chest tube removal to confirm the re-expansion of the affected lung.
Don'ts
- Don't remove the needle from the 2nd intercostal space unless the patient is stable.
- Don't use large bore chest drains.[1]
- Don't leave the chest drain more than 7 days, as it will increase the risk of infection.
References
- ↑ 1.0 1.1 1.2 1.3 1.4 1.5 1.6 MacDuff A, Arnold A, Harvey J, BTS Pleural Disease Guideline Group (2010). "Management of spontaneous pneumothorax: British Thoracic Society Pleural Disease Guideline 2010". Thorax. 65 Suppl 2: ii18–31. doi:10.1136/thx.2010.136986. PMID 20696690.
- ↑ 2.0 2.1 Sharma A, Jindal P (2008). "Principles of diagnosis and management of traumatic pneumothorax". J Emerg Trauma Shock. 1 (1): 34–41. doi:10.4103/0974-2700.41789. PMC 2700561. PMID 19561940.
<headertabs />