Subarachnoid hemorrhage CT: Difference between revisions
No edit summary |
No edit summary |
||
| Line 7: | Line 7: | ||
==CT== | ==CT== | ||
The mainstay of diagnosis of suarachnoid hemorrhage is noncontrast head computed tomography (CT), with or without lumbar puncture. | The mainstay of diagnosis of suarachnoid hemorrhage is noncontrast head computed tomography (CT), with or without lumbar puncture. | ||
The diagnosis of subarachnoid hemorrhage cannot be made on clinical grounds alone. [[Medical imaging]] is usually required to confirm or exclude bleeding. The modality of choice is [[computed tomography]] | The diagnosis of subarachnoid hemorrhage cannot be made on clinical grounds alone. [[Medical imaging]] is usually required to confirm or exclude bleeding. | ||
(CT/CAT) of the brain. | *The modality of choice is [[computed tomography]] (CT/CAT) of the brain. | ||
* | *The [[Sensitivity (tests)|sensitivity]] of CT in the first 3 days after aSAH is very high (close to 100%) | ||
**The sensitivity of CT to the presence of subarachnoid blood is strongly influenced by both the amount of blood and the time since the hemorrhage | |||
*Subarachnoid hemorrhage appears as a high-attenuating, amorphous substance that fills the normally dark CSF-filled subarachnoid spaces. | *Subarachnoid hemorrhage appears as a high-attenuating, amorphous substance that fills the normally dark CSF-filled subarachnoid spaces. | ||
*These findings are most evident in the largest subarachnoid spaces, such as the suprasellar cistern and Sylvian fissures. | *These findings are most evident in the largest subarachnoid spaces, such as the suprasellar cistern and Sylvian fissures. | ||
| Line 17: | Line 17: | ||
**The initial high-attenuation of blood and clot tend to decrease, and these appear as intermediate gray. | **The initial high-attenuation of blood and clot tend to decrease, and these appear as intermediate gray. | ||
**These findings can be isointense relative to normal brain parenchyma. | **These findings can be isointense relative to normal brain parenchyma. | ||
*In addition to detecting Subarachnoid hemorrhage, CT is useful in localizing the source of bleeding. | *In addition to detecting Subarachnoid hemorrhage, CT is useful in localizing the source of bleeding | ||
The sensitivity of CT to the presence of subarachnoid blood is strongly influenced by both the amount of blood and the time since the haemorrhage. | |||
The diagnosis is suspected when hyperattenuating material is seen filling the subarachnoid space. Most commonly this is apparent around the circle of Willis, on account of the majority of berry aneurysms occurring in this region (~65%), or in the Sylvian fissure (~30%) ref needed. | |||
Small amounts of blood can sometimes be appreciated pooling in the interpeduncular fossa, appearing as a small hyperdense triangle, or within the occipital horns of the lateral ventricles 5. | |||
Subarachnoid haemorrhages are grouped into four categories according to the amount of blood by the Fisher Grade.<ref>{{cite journal |author=Fisher C, Kistler J, Davis J |title=Relation of cerebral vasospasm to subarachnoid hemorrhage visualized by computerized tomographic scanning |journal=Neurosurgery |volume=6 |issue=1 |pages=1-9 |year=1980 |pmid=7354892}}</ref> | |||
{| style="bo[[Link title]]rder: 0px; font-size: 90%; margin: 3px;" align=center | |||
|+ | |||
! style="background: #4479BA; width: 250px;" | {{fontcolor|#FFF|Grading}} | |||
! style="background: #4479BA; width: 400px;" | {{fontcolor|#FFF|Amount of blood shown on initial CT scans}} | |||
|- | |||
| style="padding: 5px 5px; background: #DCDCDC;" | '''Grade 1''' | |||
| style="padding: 5px 5px; background: #F5F5F5;" | | |||
*No hemorrhage evident | |||
|- | |||
| style="padding: 5px 5px; background: #DCDCDC;" | '''Grade 2''' | |||
| style="padding: 5px 5px; background: #F5F5F5;" | | |||
*Subarachnoid hemorrhage less than 1 mm thick | |||
*No clots | |||
|- | |||
| style="padding: 5px 5px; background: #DCDCDC;" | '''Grade 3''' | |||
| style="padding: 5px 5px; background: #F5F5F5;" | | |||
*Subarachnoid hemorrhage more than 1 mm thick | |||
*localised clots | |||
|- | |||
| style="padding: 5px 5px; background: #DCDCDC;" | '''Grade 4''' | |||
| style="padding: 5px 5px; background: #F5F5F5;" | | |||
*Subarachnoid hemorrhage of any thickness with intra-ventricular hemorrhage (IVH) or parenchymal extension or absent blood in basal cisterns | |||
|} | |||
[http://www.radswiki.net Images courtesy of RadsWiki] | [http://www.radswiki.net Images courtesy of RadsWiki] | ||
Revision as of 15:16, 12 December 2016
|
Subarachnoid Hemorrhage Microchapters |
|
Diagnosis |
|---|
|
Treatment |
|
AHA/ASA Guidelines for the Management of Aneurysmal Subarachnoid Hemorrhage (2012)
|
|
Case Studies |
|
Subarachnoid hemorrhage CT On the Web |
|
American Roentgen Ray Society Images of Subarachnoid hemorrhage CT |
|
Risk calculators and risk factors for Subarachnoid hemorrhage CT |
Editor-In-Chief: C. Michael Gibson, M.S., M.D. [1]; Associate Editor(s)-In-Chief: Cafer Zorkun, M.D., Ph.D. [2]; Sara Mehrsefat, M.D. [3]
Overview
CT
The mainstay of diagnosis of suarachnoid hemorrhage is noncontrast head computed tomography (CT), with or without lumbar puncture. The diagnosis of subarachnoid hemorrhage cannot be made on clinical grounds alone. Medical imaging is usually required to confirm or exclude bleeding.
- The modality of choice is computed tomography (CT/CAT) of the brain.
- The sensitivity of CT in the first 3 days after aSAH is very high (close to 100%)
- The sensitivity of CT to the presence of subarachnoid blood is strongly influenced by both the amount of blood and the time since the hemorrhage
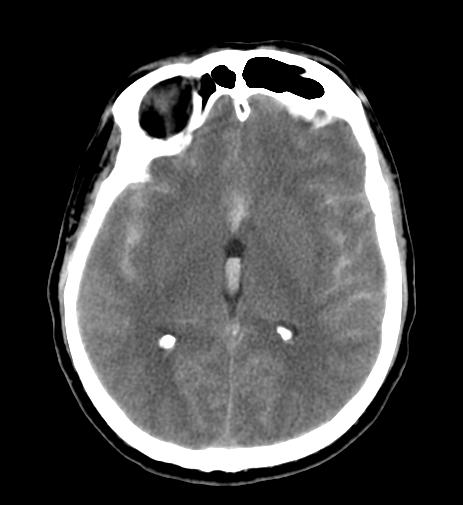
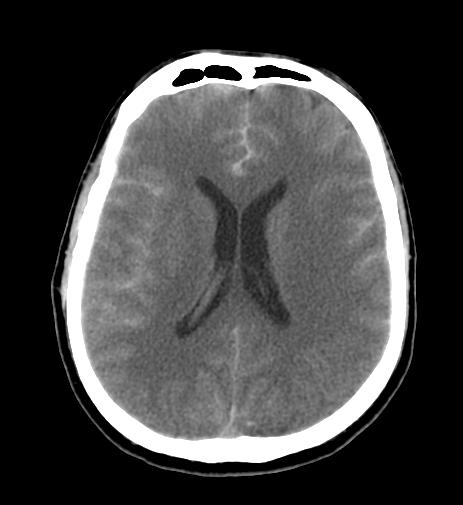
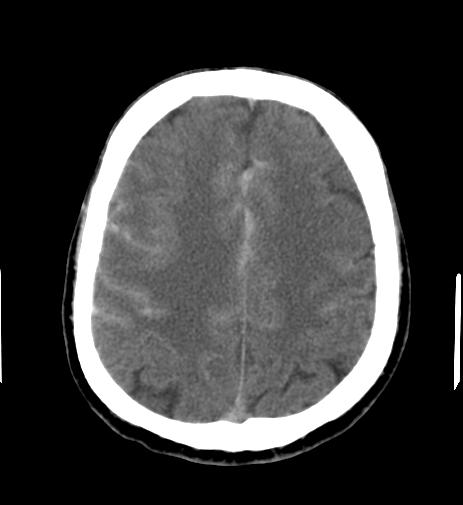
- Subarachnoid hemorrhage appears as a high-attenuating, amorphous substance that fills the normally dark CSF-filled subarachnoid spaces.
- These findings are most evident in the largest subarachnoid spaces, such as the suprasellar cistern and Sylvian fissures.
- Acute Subarachnoid hemorrhage is typically 50-60 HU.
- When CT scanning is performed several days to weeks after the initial bleed, the findings are more subtle.
- The initial high-attenuation of blood and clot tend to decrease, and these appear as intermediate gray.
- These findings can be isointense relative to normal brain parenchyma.
- In addition to detecting Subarachnoid hemorrhage, CT is useful in localizing the source of bleeding
The sensitivity of CT to the presence of subarachnoid blood is strongly influenced by both the amount of blood and the time since the haemorrhage.
The diagnosis is suspected when hyperattenuating material is seen filling the subarachnoid space. Most commonly this is apparent around the circle of Willis, on account of the majority of berry aneurysms occurring in this region (~65%), or in the Sylvian fissure (~30%) ref needed.
Small amounts of blood can sometimes be appreciated pooling in the interpeduncular fossa, appearing as a small hyperdense triangle, or within the occipital horns of the lateral ventricles 5.
Subarachnoid haemorrhages are grouped into four categories according to the amount of blood by the Fisher Grade.[1]
| Grading | Amount of blood shown on initial CT scans |
|---|---|
| Grade 1 |
|
| Grade 2 |
|
| Grade 3 |
|
| Grade 4 |
|
-
CT: Diffuse subarachnoid hemorrhage
-
CT: Diffuse subarachnoid hemorrhage
-
CT: Diffuse subarachnoid hemorrhage
-
CT: Diffuse subarachnoid hemorrhage
Once a subarachnoid hemorrhage is confirmed, the next question is about its origin. CT angiography (using radiocontrast) to identify aneurysms is generally the first step, as invasive angiography (injecting radiocontrast through a catheter advanced to the brain arteries) has a small rate of complications but is useful if there are plans to obliterate the source of bleeding, such as an aneurysm, at the same time.