Stomatitis pathophysiology
|
Stomatitis Microchapters |
|
Diagnosis |
|---|
|
Treatment |
|
Case Studies |
|
Stomatitis pathophysiology On the Web |
|
American Roentgen Ray Society Images of Stomatitis pathophysiology |
|
Risk calculators and risk factors for Stomatitis pathophysiology |
Editor-In-Chief: C. Michael Gibson, M.S., M.D. [1]; Associate Editor(s)-in-Chief: Sara Mehrsefat, M.D. [2], Usama Talib, BSc, MD [3]
Overview
Stomatitis is the inflammation of the mucosal surfaces in the mouth. Various factors can contribute to the pathogenesis of stomatitis depending on the type of stomatitis.[1]
Pathophysiology
Different mechanism are understood to cause different types of stomatitis:[1]
Infectious Causes
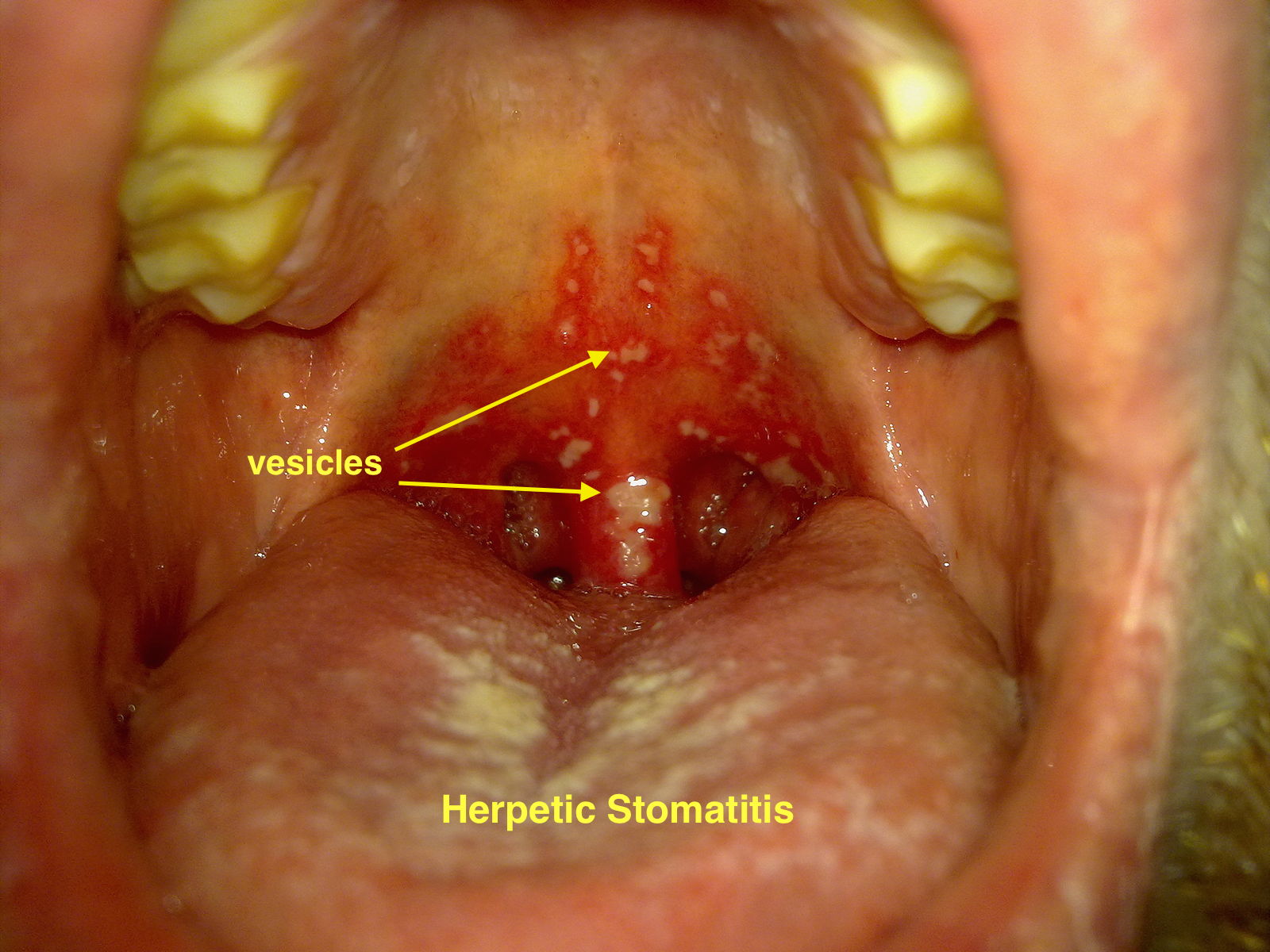
- Herpetic stomatitis:
- This type is causes by HSV-1 virus. It is caused by the destructive effect of the virus on the tissues in the form of break down of the infected cells. The infection may start as vesicles that are typically pin-head like and ultimately rupture, resulting ulceration. As a characteristic to the virus these ulcers are painful, irregular in appearance and often have a yellow-grey covering layer.
- After the lesions resolve, the virus travels though the nerves to the nerve cells and goes into a latent stage. It can then reactivate when the person becomes immunocompromised and cause symptoms.[2]
- Encephalitis associated with herpetic stomatitis is due to the interaction of HSV-1 with Toll-like receptor 2 or TLR2.
- Zoster stomatitis or chicken pox:
- Zoster stomatitis is caused by VZV.
- The vesicles of zoster stomatitis are found in a cluster on one side of the hard palate. The vesicles can also be found the buccal mucosa, gingival tissue and the tongue.
- Noma or Gangrenous stomatitis:
- Gangrenous stomatitis is also known as Noma or 'cancrum doris'. Noma or gangrenous stomatitis is focal and destructive infection caused by Borrelia vincentii, Fusobacterium and Bacteroides. It is an acute infection of the tissues in the orofacial region. Immunocompromised individuals are predisposed to develop this condition. Noma or gangrenous stomatitis is more common in children. The infection can begin as a spot or vesicle on the gingival surface of the mandibular molars and premolars. This spot or vesicle is red initially and painful and develops into an ulcer. The lesion has cone shaped expansion with bone, teeth and tissue underneath being exposed after the soft tissue sloughs off.[3]
- Bovine papular stomatitis:
- Bovine papular stomatitis is a zoonotic disease. It is caused by bovine papular stomatitis virus, starting as a single lesion and becoming a nodular mass ultimately. The virus has chemokine binding proteins that prevent the neutrophils and monocytes from migrating to the site of the pathology.[4][5]
- Trench mouth or Acute necrotizing ulcerative gingivitis:
- Trench mouth also known as vincent's angina, presents as ulceration and severe oral pain accompanied by gingival necrosis. It is characterised by acute onset of bad breath and the ulceration and destruction of the part of gum tissue present between the teeth. The scrapings from the necrotic ulcer contains fibrin, leukocytes, erythrocytes, bacteria and necrotic tissue. Fever and lymphadenopapthy may accompany.[6][7]
- Hand Foot and Mouth disease:
- It is also called enteroviral vesicular stomatitis with exanthem. It is caused by coxsackie virus group A and involves maculopapular rash on the skin of the hands , the feet and the mouth including vesicles and ulcers on the tongue, gums, buccal mucosa and the soft palate.[8]
- Candidal Stomatitis:
- Candidal stomatitis is also known as oral candidiasis. It can occur exclusively or as part of systemic candidiasis in immunocompromised individuals. It can be can present a hyperplastic or erythematous pictures due to the invasion by the virus. Glossitis has also been noticed.[9]
- HIV:
- Ulcers in the mouth are very common presentation for HIV-1 infected individuals. The ulcers are superficial and have a clear demarcation. Autoimmune deficiency is thought to be the pathogenic factor behind the oral ulcers and stomatitis related to HIV.[10][11][12]
Non-infectious Types
- Aphthous stomatitis:
- It is the most common cause of oral ulcers. A definitive pathogenesis does not exist for aphthous stomatitis, but the proposed mechanism involves immune system abnormalities and the presence of autoimmune antibodies. It is thought to be caused by some types of cytokine and T cell accumulation manifesting as a defective cell mediated arm of the immunity. It presents as round ulcers with a grey base. Recurrence is very common in aphthous ulcers.[13][14][15]
- It may take the following forms:
- Major aphthous stomatitis
- This type can last up to a few months and involves tonsils and the soft palate as well. It can subside for long intervals and then reappear.
- Minor aphthous stomatitis
- This is the characteristic form of aphthous stomatitis; it is characterized by yellow-grey, painful minute ulcers in the anterior oral cavity in the buccal and oral mucosa with raised margins. They can last from a few days up to 2 weeks.
- Herpetiform stomatitis
- Major aphthous stomatitis
- Chemotherapy-associated stomatitis:
- The chemotherapy causes RNA and DNA damage by the reactive oxygen species leading to an excessive production of inflammatory cytokines. These cytokines cause inflammation thus causing breaks in the epithelium.
- Denture stomatitis:
- Denture stomatitis effects upto 67% of denture wearers. It moct commonly affects the palatal mucosa.[16] The material used in fillings and dentures are porous because of the chemicals used and to give it a better grip. Pathogens like candida albicans can colonize such suitable sites, leading to an inflammatory response and thus denture stomatitis. The irritating effect of the foreign denture material can also contribute to the pathogenesis.[17][18]
- Pyostomatitis vegetans:
- Pyostomatitis vegetans is characterized by numerous painless, yellow, superficial pinpoint pustules with edema of the mucosa of the mouth. It is found in patients with ulcerative colitis. The vesicles can combine and involve the vermillion border of the upper as well as the lower lips. Snail track ulcerations are characteristic of pyostomatitis vegetans.[19][20]
- The involvement of skin along with the oral mucosa is characteristic of an entity called pyodermatitis pyostomatitis vegetans.[21]
- Nicotinic stomatitis:
- As the name indicates, nicotinic stomatitis is caused by use of nicotine in cigarette or pipe smokers. It normally occurs on the hard palate of individuals who use pipes to smoke. The pathogenesis is explained by the heat and not the tobacco, and thus there is no malignant potential. The condition improves within 1 to 2 weeks of smoking cessation.[22][23][24]
- Contact stomatitis:
Genetics
Though the genetics of stomatitis have not been studied extensively, it is understood that genetic polymorphisms are associated with the occurrence of stomatitis. Inherited epidermolysis bullosa is a known inherited disease and is associated with weak epithelium. [26]
Associated Conditions
The following conditions can be associated with stomatitis.[2][27][1]
- Dentures
- Folate deficiency
- Herpes
- Oropharyngeal candidiasis
- Vitamin B12 deficiency
- Chemotherapy
- Immunodeficiency
- Diabetes
- HIV
- Hand, foot and mouth disease
- Candidiasis
- Syphilis
- Chicken pox
Gross Pathology
The gross pathology of stomatitis can vary from redness and inflammation to presence of vesicles or pustules. Oral candidiasis for example may present a hyperplastic picture, erythematous picture or whitish pseudomembrane (thrush).
Herpetic Stomatitis
Aphthous stomatitis

Microscopic Pathology
The microscopic pathology helps to confirm the diagnosis and to differentiate different types of stomatitis.[30]
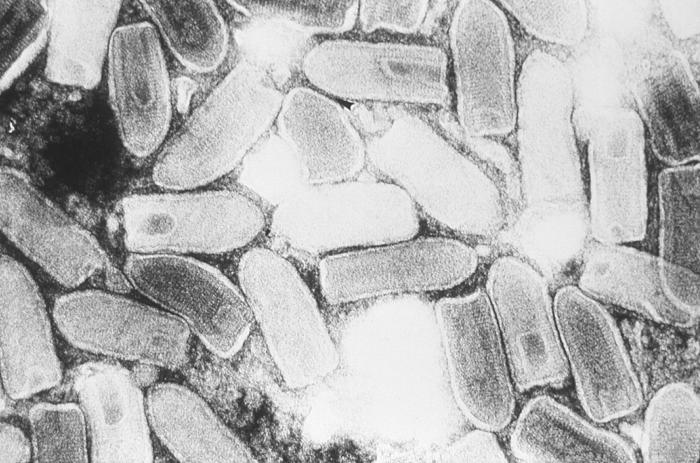
Vesicular stomatitis virus
References
- ↑ 1.0 1.1 1.2 Sonis ST (2004). "The pathobiology of mucositis". Nat Rev Cancer. 4 (4): 277–84. doi:10.1038/nrc1318. PMID 15057287.
- ↑ 2.0 2.1 Kolokotronis A, Doumas S (2006). "Herpes simplex virus infection, with particular reference to the progression and complications of primary herpetic gingivostomatitis". Clin Microbiol Infect. 12 (3): 202–11. doi:10.1111/j.1469-0691.2005.01336.x. PMID 16451405.
- ↑ Mandell; Gouglas, Gordon; Bennett, John. Principles and Practice of Infectious Diseases. Harvard Medical School: WILEY MEDICAL. p. 383. ISBN 0-471-87643-7. Unknown parameter
|firs1t=ignored (help) - ↑ Sharif S, Nakatani Y, Wise L, Corbett M, Real NC, Stuart GS; et al. (2016). "A Broad-Spectrum Chemokine-Binding Protein of Bovine Papular Stomatitis Virus Inhibits Neutrophil and Monocyte Infiltration in Inflammatory and Wound Models of Mouse Skin". PLoS One. 11 (12): e0168007. doi:10.1371/journal.pone.0168007. PMC 5148066. PMID 27936239.
- ↑ Mandell; Gouglas, Gordon; Bennett, John. Principles and Practice of Infectious Diseases. Harvard Medical School: WILEY MEDICAL. p. 988. ISBN 0-471-87643-7. Unknown parameter
|firs1t=ignored (help) - ↑ Hu J, Kent P, Lennon JM, Logan LK (2015). "Acute necrotising ulcerative gingivitis in an immunocompromised young adult". BMJ Case Rep. 2015. doi:10.1136/bcr-2015-211092. PMID 26376700.
- ↑ Mizrahi Y (2014). "[NUG--necrotizing ulcerative gingivitis: a review]". Refuat Hapeh Vehashinayim (1993). 31 (3): 41–7, 62. PMID 25219100.
- ↑ ROBINSON CR, RHODES AJ (1961). "Vesicular exanthem and stomatitis. Report of an epidemic due to Coxsacke virus Group A, Type 16". N Engl J Med. 265: 1104–5. doi:10.1056/NEJM196111302652207. PMID 14492892.
- ↑ Zhou PR, Hua H, Liu XS (2017). "Quantity of Candida Colonies in Saliva: A Diagnostic Evaluation for Oral Candidiasis". Chin J Dent Res. 20 (1): 27–32. doi:10.3290/j.cjdr.a37739. PMID 28232964.
- ↑ Lapins J, Gaines H, Lindbäck S, Lidbrink P, Emtestam L (1997). "Skin and mucosal characteristics of symptomatic primary HIV-1 infection". AIDS Patient Care STDS. 11 (2): 67–70. doi:10.1089/apc.1997.11.67. PMID 11361765.
- ↑ Sarti GM, Haddy RI, Schaffer D, Kihm J (1990). "Black hairy tongue". Am Fam Physician. 41 (6): 1751–5. PMID 2190456.
- ↑ Ramírez-Amador V, Esquivel-Pedraza L, Sierra-Madero J, Anaya-Saavedra G, González-Ramírez I, Ponce-de-León S (2003). "The Changing Clinical Spectrum of Human Immunodeficiency Virus (HIV)-Related Oral Lesions in 1,000 Consecutive Patients: A 12-Year Study in a Referral Center in Mexico". Medicine (Baltimore). 82 (1): 39–50. PMID 12544709.
- ↑ Ship JA (1996). "Recurrent aphthous stomatitis. An update". Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 81 (2): 141–7. PMID 8665304.
- ↑ Dalghous AM, Freysdottir J, Fortune F (2006). "Expression of cytokines, chemokines, and chemokine receptors in oral ulcers of patients with Behcet's disease (BD) and recurrent aphthous stomatitis is Th1-associated, although Th2-association is also observed in patients with BD". Scand J Rheumatol. 35 (6): 472–5. PMID 17343257.
- ↑ Murray LN, Amedee RG (2000). "Recurrent aphthous stomatitis". J La State Med Soc. 152 (1): 10–4. PMID 10668310.
- ↑ Arendorf TM, Walker DM (1987). "Denture stomatitis: a review". J Oral Rehabil. 14 (3): 217–27. PMID 3298586.
- ↑ Abduljabbar T, Al-Askar M, Baig MK, AlSowygh ZH, Kellesarian SV, Vohra F (2017). "Efficacy of photodynamic therapy in the inactivation of oral fungal colonization among cigarette smokers and non-smokers with denture stomatitis". Photodiagnosis Photodyn Ther. doi:10.1016/j.pdpdt.2017.01.182. PMID 28130176.
- ↑ Marinoski J, Bokor-Bratić M, Čanković M (2014). "Is denture stomatitis always related with candida infection? A case control study". Med Glas (Zenica). 11 (2): 379–84. PMID 25082257.
- ↑ Magliocca KR, Fitzpatrick SG (2017). "Autoimmune Disease Manifestations in the Oral Cavity". Surg Pathol Clin. 10 (1): 57–88. doi:10.1016/j.path.2016.11.001. PMID 28153136.
- ↑ Pellicer Z, Santiago JM, Rodriguez A, Alonso V, Antón R, Bosca MM (2012). "Management of cutaneous disorders related to inflammatory bowel disease". Ann Gastroenterol. 25 (1): 21–26. PMC 3959344. PMID 24713996.
- ↑ Matias Fde A, Rosa DJ, Carvalho MT, Castañon MC (2011). "Pyodermatitis-pyostomatitis vegetans: case report and review of medical literature". An Bras Dermatol. 86 (4 Suppl 1): S137–40. PMID 22068794.
- ↑ "Oral pathology quiz. Case number 2. Nicotine stomatitis". J N J Dent Assoc. 81 (1): 15, 19. 2010. PMID 20455505.
- ↑ Dreyer WP, de Waal J (2009). "Oral medicine case book 23. Case 1--snuff dipper's lesion, Case 2--nicotinic stomatitis". SADJ. 64 (10): 490–1. PMID 20306871 : 20306871 Check
|pmid=value (help). - ↑ Taybos G (2003). "Oral changes associated with tobacco use". Am J Med Sci. 326 (4): 179–82. PMID 14557730.
- ↑ Larsen KR, Johansen JD, Reibel J, Zachariae C, Pedersen AM (2017). "Symptomatic oral lesions may be associated with contact allergy to substances in oral hygiene products". Clin Oral Investig. doi:10.1007/s00784-017-2053-y. PMID 28084550.
- ↑ Gomes CC, Gomez RS, Zina LG, Amaral FR (2016). "Recurrent aphthous stomatitis and Helicobacter pylori". Med Oral Patol Oral Cir Bucal. 21 (2): e187–91. PMC 4788798. PMID 26827061.
- ↑ R. Morgan, J. Tsang, N. Harrington & L. Fook (2001). "Survey of hospital doctors' attitudes and knowledge of oral conditions in older patients". Postgraduate medical journal. 77 (908): 392–394. PMID 11375454. Unknown parameter
|month=ignored (help) - ↑ title="By Klaus D. Peter, Gummersbach, Germany (Own work) [CC BY 3.0 de (http://creativecommons.org/licenses/by/3.0/de/deed.en)], via Wikimedia Commons" href="https://commons.wikimedia.org/wiki/File%3AStomatitis_herpetica.jpg"><img width="512" alt="Stomatitis herpetica" src="https://upload.wikimedia.org/wikipedia/commons/thumb/8/84/Stomatitis_herpetica.jpg/512px-Stomatitis_herpetica.jpg"
- ↑ title="By Farhan 9909 (Own work) [CC BY-SA 4.0 (http://creativecommons.org/licenses/by-sa/4.0)], via Wikimedia Commons" href="https://commons.wikimedia.org/wiki/File%3AAphthous_stomatitis_on_the_labial_mucosa.jpg"><img width="512" alt="Aphthous stomatitis on the labial mucosa" src="https://upload.wikimedia.org/wikipedia/commons/thumb/d/d3/Aphthous_stomatitis_on_the_labial_mucosa.jpg/512px-Aphthous_stomatitis_on_the_labial_mucosa.jpg"
- ↑ title="By Klaus D. Peter, Gummersbach, Germany (Own work) [CC BY 3.0 de (http://creativecommons.org/licenses/by/3.0/de/deed.en)], via Wikimedia Commons" href="https://commons.wikimedia.org/wiki/File%3AStomatitis_herpetica.jpg"><img width="512" alt="Stomatitis herpetica" src="https://upload.wikimedia.org/wikipedia/commons/thumb/8/84/Stomatitis_herpetica.jpg/512px-Stomatitis_herpetica.jpg"
- ↑ title="By Klaus D. Peter, Gummersbach, Germany (Own work) [CC BY 3.0 de (http://creativecommons.org/licenses/by/3.0/de/deed.en)], via Wikimedia Commons" href="https://commons.wikimedia.org/wiki/File%3AStomatitis_herpetica.jpg"><img width="512" alt="Stomatitis herpetica" src="https://upload.wikimedia.org/wikipedia/commons/thumb/8/84/Stomatitis_herpetica.jpg/512px-Stomatitis_herpetica.jpg"