Sandbox : anmol: Difference between revisions
| Line 202: | Line 202: | ||
*The sensitivity of sestamibi scintigraphy can be increased by using it concomitantly with neck ultrasound and/or SPECT. <ref name="pmid18794320">{{cite journal| author=Eslamy HK, Ziessman HA| title=Parathyroid scintigraphy in patients with primary hyperparathyroidism: 99mTc sestamibi SPECT and SPECT/CT. | journal=Radiographics | year= 2008 | volume= 28 | issue= 5 | pages= 1461-76 | pmid=18794320 | doi=10.1148/rg.285075055 | pmc= | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=18794320 }} </ref><ref name="pmid12153604">{{cite journal| author=Haber RS, Kim CK, Inabnet WB| title=Ultrasonography for preoperative localization of enlarged parathyroid glands in primary hyperparathyroidism: comparison with (99m)technetium sestamibi scintigraphy. | journal=Clin Endocrinol (Oxf) | year= 2002 | volume= 57 | issue= 2 | pages= 241-9 | pmid=12153604 | doi= | pmc= | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=12153604 }} </ref> | *The sensitivity of sestamibi scintigraphy can be increased by using it concomitantly with neck ultrasound and/or SPECT. <ref name="pmid18794320">{{cite journal| author=Eslamy HK, Ziessman HA| title=Parathyroid scintigraphy in patients with primary hyperparathyroidism: 99mTc sestamibi SPECT and SPECT/CT. | journal=Radiographics | year= 2008 | volume= 28 | issue= 5 | pages= 1461-76 | pmid=18794320 | doi=10.1148/rg.285075055 | pmc= | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=18794320 }} </ref><ref name="pmid12153604">{{cite journal| author=Haber RS, Kim CK, Inabnet WB| title=Ultrasonography for preoperative localization of enlarged parathyroid glands in primary hyperparathyroidism: comparison with (99m)technetium sestamibi scintigraphy. | journal=Clin Endocrinol (Oxf) | year= 2002 | volume= 57 | issue= 2 | pages= 241-9 | pmid=12153604 | doi= | pmc= | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=12153604 }} </ref> | ||
*The sensitivity of sestamibi scintigraphy is 80% - 90%.<ref name="pmid8678959">{{cite journal |vauthors=Chapuis Y, Fulla Y, Bonnichon P, Tarla E, Abboud B, Pitre J, Richard B |title=Values of ultrasonography, sestamibi scintigraphy, and intraoperative measurement of 1-84 PTH for unilateral neck exploration of primary hyperparathyroidism |journal=World J Surg |volume=20 |issue=7 |pages=835–9; discussion 839–40 |year=1996 |pmid=8678959 |doi= |url=}}</ref><ref name="pmid17685957">{{cite journal |vauthors=Prasannan S, Davies G, Bochner M, Kollias J, Malycha P |title=Minimally invasive parathyroidectomy using surgeon-performed ultrasound and sestamibi |journal=ANZ J Surg |volume=77 |issue=9 |pages=774–7 |year=2007 |pmid=17685957 |doi=10.1111/j.1445-2197.2007.04227.x |url=}}</ref><ref name="pmid20625763">{{cite journal |vauthors=Gómez-Ramírez J, Sancho-Insenser JJ, Pereira JA, Jimeno J, Munné A, Sitges-Serra A |title=Impact of thyroid nodular disease on 99mTc-sestamibi scintigraphy in patients with primary hyperparathyroidism |journal=Langenbecks Arch Surg |volume=395 |issue=7 |pages=929–33 |year=2010 |pmid=20625763 |doi=10.1007/s00423-010-0680-8 |url=}}</ref> | *The sensitivity of sestamibi scintigraphy is 80% - 90%.<ref name="pmid8678959">{{cite journal |vauthors=Chapuis Y, Fulla Y, Bonnichon P, Tarla E, Abboud B, Pitre J, Richard B |title=Values of ultrasonography, sestamibi scintigraphy, and intraoperative measurement of 1-84 PTH for unilateral neck exploration of primary hyperparathyroidism |journal=World J Surg |volume=20 |issue=7 |pages=835–9; discussion 839–40 |year=1996 |pmid=8678959 |doi= |url=}}</ref><ref name="pmid17685957">{{cite journal |vauthors=Prasannan S, Davies G, Bochner M, Kollias J, Malycha P |title=Minimally invasive parathyroidectomy using surgeon-performed ultrasound and sestamibi |journal=ANZ J Surg |volume=77 |issue=9 |pages=774–7 |year=2007 |pmid=17685957 |doi=10.1111/j.1445-2197.2007.04227.x |url=}}</ref><ref name="pmid20625763">{{cite journal |vauthors=Gómez-Ramírez J, Sancho-Insenser JJ, Pereira JA, Jimeno J, Munné A, Sitges-Serra A |title=Impact of thyroid nodular disease on 99mTc-sestamibi scintigraphy in patients with primary hyperparathyroidism |journal=Langenbecks Arch Surg |volume=395 |issue=7 |pages=929–33 |year=2010 |pmid=20625763 |doi=10.1007/s00423-010-0680-8 |url=}}</ref> | ||
{| | |||
[[image:Parathyroid subtraction.jpg|center|thumb| | | | ||
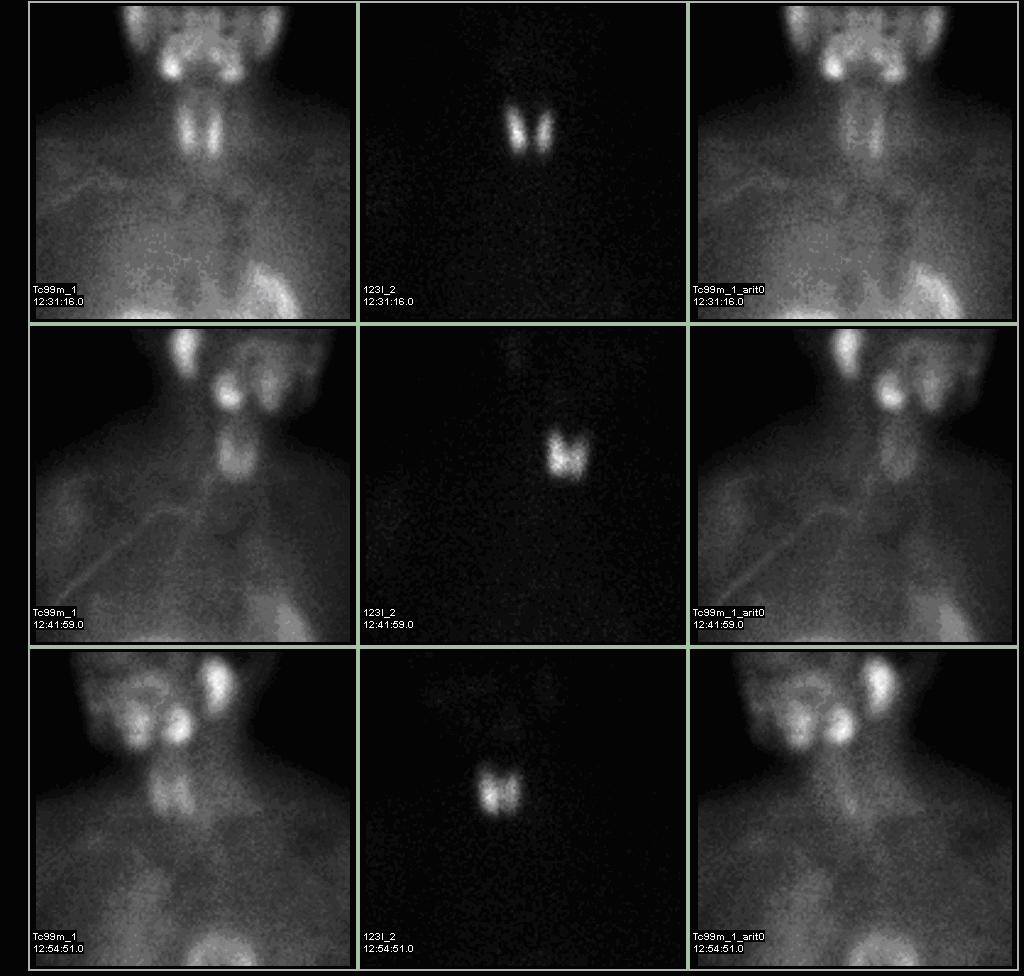
[[image:Parathyroid subtraction.jpg|center|thumb|450px|Dual tracer Tc-99m sestamibi scintigraphy - A nuclear medicine parathyroid scan demonstrates a parathyroid adenoma adjacent to the left inferior pole of the thyroid gland. The above study was performed with Technetium-Sestamibi (1st column) and Iodine-123 (2nd column) simultaneous imaging and the subtraction technique (3rd column). -- [https://commons.wikimedia.org/wiki/File%3AParathyroid_subtraction.jpg Source:Myohan at en.wikipedia, via Wikimedia Commons]]] | |||
| | |||
[[image:Sestamibi scan gif.gif|center|thumb|600px|Tc-99m sestamibi scan - Parathyroid adenomas typically retain activity on late scans after wash-out in the thyroid has occurred. - [https://radiopaedia.org/cases/16675 Source:Case courtesy of Dr Roberto Schubert, Radiopaedia.org, rID: 16675]]] | |||
=SPECT= | =SPECT= | ||
Revision as of 21:35, 6 September 2017
|
Hyperparathyroidism Microchapters |
|
Diagnosis |
|---|
|
Treatment |
|
Case Studies |
|
Sandbox : anmol On the Web |
|
American Roentgen Ray Society Images of Sandbox : anmol |
Editor-In-Chief: C. Michael Gibson, M.S., M.D. [1]; Associate Editor(s)-in-Chief: Anmol Pitliya, M.B.B.S. M.D.[2]
Classification
| Classification of hyperparathyridism | |||
|---|---|---|---|
| Features | Primary hyperparathyroidism | Secondary hyperparathyroidism | Tertiary hyperparathyroidism |
| Pathology | Hyperfunction of parathyroid cells due to hyperplasia, adenoma or carcinoma. | Physiological stimulation of parathyroid in response to hypocalcaemia. | Following long term physiological stimulation leading to hyperplasia. |
| Cause | |||
| Associations | May be associated with multiple endocrine neoplasia. | Usually due to chronic renal failure or other causes of Vitamin D deficiency. | Seen in chronic renal failure. |
| Serum calcium | High | Low/Normal | High |
| Serum phosphate | Low/Normal | High | High |
| Management | Usually surgery if symptomatic. Cincacalcet can be considered in those not fit for surgery. | Treatment of underlying cause. | Usually cinacalcet or surgery in those that don't respond. |
Causes
Genetic causes
- HRPT2 gene mutations:[1]
- HRPT2 gene code for parafibromin protein.
- HRPT2 gene mutations are found in a type of familial hyperparathyroidism, hyperparathyroidism-jaw tumor (HPT-JT) syndrome.
- HRTP2 gene mutations increases risk of parathyroid carcinoma.
- Cyclin D1 gene (CCND1)/PRAD1 gene:[2][3]
- PRAD1 (parathyroid adenoma 1) is a protooncogene located on chromosome 11q13.
- Cyclin D1 gene translocation and oncogene action observerd in 8% of adenomas
- Cyclin D1 gene overexpression is pbserved in 20% to 40% of parathyroid adenomas
- MEN1 gene:[2][4]
- MEN1 is a tumor supressor gene on chronosome 11q13.
- Somatic loss of single MEN1 allele is observed in 25% to 40% of sporadic parathyroid adenomas.
Pathogenesis
Associated conditions
- Hypercalcemia
- Chronic renal failure
- Osteitis fibrous cystica
- Osteoporosis
- Osteomalacia
- Osteoarthritis
- Brown tumor
- Multiple endocrine neoplasia type 1, type 2A, and type 4
- Familial isolated hyperparathyroidism
- Neonatal severe hyperparathyroidism
- Familial hypocalciuric hypercalcemia
- Hyperparathyroid-jaw tumor syndrome
- Pancreatitis[5]
Natural history, Prognosis and Complications
Natural history
- Primary hyperparathyroidism usually develops in the fifth decade of life, in post-menopausal women and starts as asymptomatic hypercalcemia in presence of increased parathyroid hormone.
- If left untreated, some of patients with primary hyperparathyroidism may commonly develop marked hypercalcemia, marked hypercalciuria, cortical bone demineralization and nephrolithiasis.[6][7]
- Secondary hyperparathyroidism arise in the early course of chronic renal failure. As renal failure progress, secondary hyperparathyroidism becomes more notable.[8]
- Secondary hyperparathyroidism leads to vascular calcification due to elevated calcium and phosphorus levels. This is strongly associated with increase in morbidity and mortality.[9]
- If left untreated, secondary hyperparathyroidism carries an increased risk of vascular calcification with increasing age and duration of dialysis in patients.
- Tertiary hyperparathyroidism usually develops in post renal transplant patients.[10]
- If left untreated, tertiary hyperparathyroidism in post renal transplant patients may carry the risk of amyloid deposition, calciphylaxis, destructive or erosive spondyloarthropathy, osteonecrosis, and musculoskeletal infections.
Complications
Primary hyperparathyroidism
Majority of complications of primary hyperparathyroidism are due to hypercalcemia. Common complications of primary hyperparathyroidism include:
- Bone related complication:[11][12]
- Brown tumor
- Osteitis fibrous cystica
- Osteoporosis
- Cardiac complications:[13]
- Aortic and mitral valve calcification
- Calcific deposits in the myocardium
- Left ventricular hypertrophy
- Endocrine complications:[5]
- Pancreatitis
- Gastrointestinal complications:[14]
- Peptic ulcer disease
- Metabolic complications:[15][16][14][17]
- Hypercalcemic crisis
- Osteomalacia
- Neuromuscular complications:
- Neuropathic muscle disease
- Pregnancy related complications:[18]
- Neonatal hypoparathyroidism
- Psychiatric complications:[19][20][21]
- Anxiety
- Cognitive dysfunction including verbal memory and nonverbal abstraction
- Depression
- Irritability
- Lack of concentration
- Sleep disturbances
- Renal complications:[6][22][23]
- Hypercalciuria
- Nephrolithiasis
- Nephrocalcinosis
- Renal insufficiency (impairement of GFR)
- Rheumatologic complications:[24][25][26]
- Gout
- Osteoarthritis
- Pseudogout
Secondary hyperparathyroidism
Complications of secondary hyperparathyroidism includes:
- Cardiovascular complications:[27]
- Impaired left ventricular diastolic function
- Left ventricular hypertrophy
- Hematologic complication:[28]
- Platlet function inhibition
- Metabolic complicattions:[29][30]
- Metabolic syndrome
- Musculoskeletal complications:[31][32][33]
- Renal Osteodystrophy
- Brown cysts
- Osteitis fibrosa cystica
- Osteoporosis
- Osteosclerosis
- Renal Osteodystrophy
- Neurologic complications:[34][35]
- Electroencephalogram abnormalities
- Uremic neuropathy
- Neuromuscular complications:[36]
- Neuropathic muscle disease
- System non-specific complications:[37]
- Metastatic calcifications
Tertiary hyperparathyroidism
Complications of tertiary hyperparathyroidism post renal transplantation includes:[10]
- Metabolic complications:[38]
- Calciphylaxis
- Musculoskeletal complications:
- Musculoskeletal infections
- Osteonecrosis
- Neuromuscular complications:[39]
- Neuropathic muscle disease
- Renal complications:[40]
- Nephrolithiasis
- Rheumatologic complications:[41]
- Destructive or erosive spondyloarthropathy
- System non-specific complications:
- Amyloid deposition
- Metastatic calcifications
Prognosis
- Prognosis of primary hyperparathyroidism is generally excellent after parathyroidectomy.
- The complications of primary hyperparathyroidism resolves after the treatment.
- Untreated complication of primary hyperparathyroidism may be fatal.[14]
- Effective treatment can reduce morbidity and mortality associated with uncontrolled secondary hyperparathyroidism.[9]
- Hyperphosphatemia and metastatic calcification results due elevated product of serum calcium and serum phosphorus. Both conditions are present in patients with secondary hyperparathyroidism in presence of end stage renal disease. This leads to a significant increase in morbidity and mortality. Aggressive control of hyperphosphatemia may improve prognosis[37].
- Prognosis of tertiary hyperparathyroidism is generally good after resection of abnormal hyperplastic gland.[42]
ECG
There are no CT scan findings associated with hyperparathyroidism. However, a CT scan may be helpful in the diagnosis of cardiac complications of hyperparathyroidism. Findings on ECG are due to hypercalcemia and includes:[43]
- ST segment - ST segment is short in patients with hyperparathyroidism when compared to normocalcemic patients. This represents a decrease in systolic interval.
- QRS complex - QRS complex has an increased amplitudein patients with hyperparathyroidism when compared to normocalcemic patients. This represents an increase in ventricular muscle mass.
- T wave - T wave is prolonged in patients with hyperparathyroidism when compared to normocalcemic patients.
X-ray
CT scan
MRI
Ultrasound
TC-99m Sestamibi Scintigraphy
- Technetium-99m-methoxyisobutylisonitrile (99mTc-sestamibi or MIBI) scintigraphy is the most popular investigation for preoperative localization of hyper-functioning parathyroid glands.[44]
- Most of the sestamibi is retained in mitochondria of thyroid and abnormal parathyroid tissue and is a function of mitochondrial activity.[45]
- The basis of this "single-isotope, double-phase technique" is that sestamibi washes out of the thyroid more rapidly than from abnormal parathyroid tissue.[46]
- Multiple planar images are obtained, typically one shortly after injection of 99mTc-sestamibi and another after two hours to identify the foci of retained sestamibi showing hyper-functioning parathyroid tissue.
- As all parathyroid lesions does not retain sestamibi nor all thyroid tissue washes out quickly, subtraction imaging may be beneficial.[47]
- Subtraction technique uses dual contrast Tc-99m sestamibi along with iodine-123 or 99m-technicium pertechnetate which is taken by thyroid tissue only. Iodine-123/99m-technicium pertechnetate images of thyroid are later digitally subtracted from Tc-99m sestamibi images leading to visualization of parathyroid tissue only.[48]
- Presence of solid thyroid nodule is the most common cause of false positive results. Other causes of false positive results may include thyroid carcinoma, lymphoma, and lymphadenopathy.
- The sensitivity of sestamibi scintigraphy can be increased by using it concomitantly with neck ultrasound and/or SPECT. [49][50]
- The sensitivity of sestamibi scintigraphy is 80% - 90%.[51][52][53]
 |
 SPECT
PET
DXA
Other diagnostic studiesIntraoperative parathyroid hormone (IOPTH)
Technique for intraoperative parathyroid hormone (IOPTH) monitoring
Super Selective Venous SamplingSelective arteriography
Angiography
References |
- ↑ Shattuck TM, Välimäki S, Obara T, Gaz RD, Clark OH, Shoback D; et al. (2003). "Somatic and germ-line mutations of the HRPT2 gene in sporadic parathyroid carcinoma". N Engl J Med. 349 (18): 1722–9. doi:10.1056/NEJMoa031237. PMID 14585940.
- ↑ 2.0 2.1 Westin G, Björklund P, Akerström G (2009). "Molecular genetics of parathyroid disease". World J Surg. 33 (11): 2224–33. doi:10.1007/s00268-009-0022-6. PMID 19373510.
- ↑ Hsi ED, Zukerberg LR, Yang WI, Arnold A (1996). "Cyclin D1/PRAD1 expression in parathyroid adenomas: an immunohistochemical study". J Clin Endocrinol Metab. 81 (5): 1736–9. doi:10.1210/jcem.81.5.8626826. PMID 8626826.
- ↑ Agarwal SK, Kester MB, Debelenko LV, Heppner C, Emmert-Buck MR, Skarulis MC; et al. (1997). "Germline mutations of the MEN1 gene in familial multiple endocrine neoplasia type 1 and related states". Hum Mol Genet. 6 (7): 1169–75. PMID 9215689.
- ↑ 5.0 5.1 Bai HX, Giefer M, Patel M, Orabi AI, Husain SZ (2012). "The association of primary hyperparathyroidism with pancreatitis". J. Clin. Gastroenterol. 46 (8): 656–61. doi:10.1097/MCG.0b013e31825c446c. PMC 4428665. PMID 22874807.
- ↑ 6.0 6.1 Peacock M (2002). "Primary hyperparathyroidism and the kidney: biochemical and clinical spectrum". J. Bone Miner. Res. 17 Suppl 2: N87–94. PMID 12412783.
- ↑ Silverberg SJ, Shane E, de la Cruz L, Dempster DW, Feldman F, Seldin D, Jacobs TP, Siris ES, Cafferty M, Parisien MV (1989). "Skeletal disease in primary hyperparathyroidism". J. Bone Miner. Res. 4 (3): 283–91. doi:10.1002/jbmr.5650040302. PMID 2763869.
- ↑ Nikodimopoulou M, Liakos S (2011). "Secondary hyperparathyroidism and target organs in chronic kidney disease". Hippokratia. 15 (Suppl 1): 33–8. PMC 3139677. PMID 21897756.
- ↑ 9.0 9.1 Cunningham J, Locatelli F, Rodriguez M (2011). "Secondary hyperparathyroidism: pathogenesis, disease progression, and therapeutic options". Clin J Am Soc Nephrol. 6 (4): 913–21. doi:10.2215/CJN.06040710. PMID 21454719.
- ↑ 10.0 10.1 Jevtic V (2003). "Imaging of renal osteodystrophy". Eur J Radiol. 46 (2): 85–95. doi:10.1016/S0720-048X(03)00072-X. PMID 12714225.
- ↑ Bandeira F, Cusano NE, Silva BC, Cassibba S, Almeida CB, Machado VC, Bilezikian JP (2014). "Bone disease in primary hyperparathyroidism". Arq Bras Endocrinol Metabol. 58 (5): 553–61. PMC 4315357. PMID 25166047.
- ↑ Mazzuoli GF, D'Erasmo E, Pisani D (1998). "Primary hyperparathyroidism and osteoporosis". Aging (Milano). 10 (3): 225–31. PMID 9801732.
- ↑ Stefenelli T, Abela C, Frank H, Koller-Strametz J, Globits S, Bergler-Klein J, Niederle B (1997). "Cardiac abnormalities in patients with primary hyperparathyroidism: implications for follow-up". J. Clin. Endocrinol. Metab. 82 (1): 106–12. doi:10.1210/jcem.82.1.3666. PMID 8989242.
- ↑ 14.0 14.1 14.2 Corlew DS, Bryda SL, Bradley EL, DiGirolamo M (1985). "Observations on the course of untreated primary hyperparathyroidism". Surgery. 98 (6): 1064–71. PMID 3878002.
- ↑ Fitzpatrick LA, Bilezikian JP (1987). "Acute primary hyperparathyroidism". Am. J. Med. 82 (2): 275–82. PMID 3812520.
- ↑ Ahmad S, Kuraganti G, Steenkamp D (2015). "Hypercalcemic crisis: a clinical review". Am. J. Med. 128 (3): 239–45. doi:10.1016/j.amjmed.2014.09.030. PMID 25447624.
- ↑ Lips P (2001). "Vitamin D deficiency and secondary hyperparathyroidism in the elderly: consequences for bone loss and fractures and therapeutic implications". Endocr Rev. 22 (4): 477–501. doi:10.1210/edrv.22.4.0437. PMID 11493580.
- ↑ Poomthavorn P, Ongphiphadhanakul B, Mahachoklertwattana P (2008). "Transient neonatal hypoparathyroidism in two siblings unmasking maternal normocalcemic hyperparathyroidism". Eur. J. Pediatr. 167 (4): 431–4. doi:10.1007/s00431-007-0528-6. PMID 17569990.
- ↑ Walker MD, McMahon DJ, Inabnet WB, Lazar RM, Brown I, Vardy S, Cosman F, Silverberg SJ (2009). "Neuropsychological features in primary hyperparathyroidism: a prospective study". J. Clin. Endocrinol. Metab. 94 (6): 1951–8. doi:10.1210/jc.2008-2574. PMC 2690425. PMID 19336505.
- ↑ Espiritu RP, Kearns AE, Vickers KS, Grant C, Ryu E, Wermers RA (2011). "Depression in primary hyperparathyroidism: prevalence and benefit of surgery". J. Clin. Endocrinol. Metab. 96 (11): E1737–45. doi:10.1210/jc.2011-1486. PMID 21917870.
- ↑ McAllion SJ, Paterson CR (1989). "Psychiatric morbidity in primary hyperparathyroidism". Postgrad Med J. 65 (767): 628–31. PMC 2429194. PMID 2608590.
- ↑ Lila AR, Sarathi V, Jagtap V, Bandgar T, Menon PS, Shah NS (2012). "Renal manifestations of primary hyperparathyroidism". Indian J Endocrinol Metab. 16 (2): 258–62. doi:10.4103/2230-8210.93745. PMC 3313745. PMID 22470864.
- ↑ Tassone F, Gianotti L, Emmolo I, Ghio M, Borretta G (2009). "Glomerular filtration rate and parathyroid hormone secretion in primary hyperparathyroidism". J. Clin. Endocrinol. Metab. 94 (11): 4458–61. doi:10.1210/jc.2009-0587. PMID 19808852.
- ↑ Michael JW, Schlüter-Brust KU, Eysel P (2010). "The epidemiology, etiology, diagnosis, and treatment of osteoarthritis of the knee". Dtsch Arztebl Int. 107 (9): 152–62. doi:10.3238/arztebl.2010.0152. PMC 2841860. PMID 20305774.
- ↑ Hochberg, Marc (2015). "204. Primary hyperparathyroidism: rheumatologic manifestations and bone disease". Rheumatology. Philadelphia, PA: Mosby/Elsevier. p. 1668. ISBN 9780323091381.
- ↑ Rubin MR, Silverberg SJ (2002). "Rheumatic manifestations of primary hyperparathyroidism and parathyroid hormone therapy". Curr Rheumatol Rep. 4 (2): 179–85. PMID 11890884.
- ↑ Strózecki P, Adamowicz A, Nartowicz E, Odrowaz-Sypniewska G, Włodarczyk Z, Manitius J (2001). "Parathormon, calcium, phosphorus, and left ventricular structure and function in normotensive hemodialysis patients". Ren Fail. 23 (1): 115–26. PMID 11256521.
- ↑ Remuzzi G, Benigni A, Dodesini P, Schieppati A, Livio M, Poletti E, Mecca G, de Gaetano G (1981). "Parathyroid hormone inhibits human platelet function". Lancet. 2 (8259): 1321–3. doi:10.1016/S0140-6736(81)91343-X. PMID 6118720.
- ↑ Saab G, Whaley-Connell A, Bombeck A, Kurella Tamura M, Li S, Chen SC, McFarlane SI, Sowers JR, Norris K, Bakris GL, McCullough PA (2011). "The Association between Parathyroid Hormone Levels and the Cardiorenal Metabolic Syndrome in Non-Diabetic Chronic Kidney Disease". Cardiorenal Med. 1 (2): 123–130. doi:10.1159/000327149. PMC 3101512. PMID 22258399.
- ↑ Hjelmesæth, Jøran; Hofsø, Dag; Aasheim, Erlend T; Jenssen, Trond; Moan, Johan; Hager, Helle; Røislien, Jo; Bollerslev, Jens (2009). "Parathyroid hormone, but not vitamin D, is associated with the metabolic syndrome in morbidly obese women and men: a cross-sectional study". Cardiovascular Diabetology. 8 (1): 7. doi:10.1186/1475-2840-8-7. ISSN 1475-2840.
- ↑ Spaulding CM, Young G (1997). "Osteitis fibrosa cystica and chronic renal failure". J Am Podiatr Med Assoc. 87 (5): 238–40. doi:10.7547/87507315-87-5-238. PMID 9158318.
- ↑ Eastwood JB (1977). "Renal osteodystrophy--a radiological review". CRC Crit Rev Diagn Imaging. 9 (1): 77–104. PMID 328228.
- ↑ Adams JE (1999). "Renal bone disease: radiological investigation". Kidney Int. Suppl. 73: S38–41. PMID 10633462.
- ↑ Goldstein DA, Feinstein EI, Chui LA, Pattabhiraman R, Massry SG (1980). "The relationship between the abnormalities in electroencephalogram and blood levels of parathyroid hormone in dialysis patients". J. Clin. Endocrinol. Metab. 51 (1): 130–4. doi:10.1210/jcem-51-1-130. PMID 6892917.
- ↑ Avram MM, Feinfeld DA, Huatuco AH (1978). "Search for the uremic toxin. Decreased motor-nerve conduction velocity and elevated parathyroid hormone in uremia". N. Engl. J. Med. 298 (18): 1000–3. doi:10.1056/NEJM197805042981805. PMID 205786.
- ↑ Mallette LE, Patten BM, Engel WK (1975). "Neuromuscular disease in secondary hyperparathyroidism". Ann. Intern. Med. 82 (4): 474–83. PMID 47234.
- ↑ 37.0 37.1 Block GA, Hulbert-Shearon TE, Levin NW, Port FK (1998). "Association of serum phosphorus and calcium x phosphate product with mortality risk in chronic hemodialysis patients: a national study". Am. J. Kidney Dis. 31 (4): 607–17. PMID 9531176.
- ↑ Barbur MA, Kurjak M, Becker K (1997). "[Systematic calciphylaxis in chronic renal failure: fulminant course after kidney transplantation]". Pathologe (in German). 18 (6): 453–8. PMID 9451734.
- ↑ Gerhardt RE, Zeitlin EL (1978). "Neuromuscular disease in tertiary hyperparathyroidism". Arch. Intern. Med. 138 (6): 1013–5. PMID 646555.
- ↑ Kim H, Cheigh JS, Ham HW (2001). "Urinary stones following renal transplantation". Korean J. Intern. Med. 16 (2): 118–22. PMC 4531707. PMID 11590898.
- ↑ Adler JS, Cameron DC (1989). "Erosive spondylo-arthropathy and tertiary hyperparathyroidism". Australas Radiol. 33 (1): 90–2. PMID 2712794.
- ↑ Nichol PF, Starling JR, Mack E, Klovning JJ, Becker BN, Chen H (2002). "Long-term follow-up of patients with tertiary hyperparathyroidism treated by resection of a single or double adenoma". Ann. Surg. 235 (5): 673–8, discussion 678–80. PMC 1422493. PMID 11981213.
- ↑ Lind L, Ljunghall S (1994). "Serum calcium and the ECG in patients with primary hyperparathyroidism". J Electrocardiol. 27 (2): 99–103. PMID 8201301.
- ↑ Palestro CJ, Tomas MB, Tronco GG (2005). "Radionuclide imaging of the parathyroid glands". Semin Nucl Med. 35 (4): 266–76. doi:10.1053/j.semnuclmed.2005.06.001. PMID 16150247.
- ↑ Hetrakul N, Civelek AC, Stagg CA, Udelsman R (2001). "In vitro accumulation of technetium-99m-sestamibi in human parathyroid mitochondria". Surgery. 130 (6): 1011–8. doi:10.1067/msy.2001.118371. PMID 11742331.
- ↑ Taillefer R, Boucher Y, Potvin C, Lambert R (1992). "Detection and localization of parathyroid adenomas in patients with hyperparathyroidism using a single radionuclide imaging procedure with technetium-99m-sestamibi (double-phase study)". J Nucl Med. 33 (10): 1801–7. PMID 1328564.
- ↑ Thulé P, Thakore K, Vansant J, McGarity W, Weber C, Phillips LS (1994). "Preoperative localization of parathyroid tissue with technetium-99m sestamibi 123I subtraction scanning". J Clin Endocrinol Metab. 78 (1): 77–82. doi:10.1210/jcem.78.1.8288719. PMID 8288719.
- ↑ Ryhänen EM, Schildt J, Heiskanen I, Väisänen M, Ahonen A, Löyttyniemi E; et al. (2015). "(99m)Technetium Sestamibi-(123)Iodine Scintigraphy Is More Accurate Than (99m)Technetium Sestamibi Alone before Surgery for Primary Hyperparathyroidism". Int J Mol Imaging. 2015: 391625. doi:10.1155/2015/391625. PMC 4333274. PMID 25722888.
- ↑ Eslamy HK, Ziessman HA (2008). "Parathyroid scintigraphy in patients with primary hyperparathyroidism: 99mTc sestamibi SPECT and SPECT/CT". Radiographics. 28 (5): 1461–76. doi:10.1148/rg.285075055. PMID 18794320.
- ↑ Haber RS, Kim CK, Inabnet WB (2002). "Ultrasonography for preoperative localization of enlarged parathyroid glands in primary hyperparathyroidism: comparison with (99m)technetium sestamibi scintigraphy". Clin Endocrinol (Oxf). 57 (2): 241–9. PMID 12153604.
- ↑ Chapuis Y, Fulla Y, Bonnichon P, Tarla E, Abboud B, Pitre J, Richard B (1996). "Values of ultrasonography, sestamibi scintigraphy, and intraoperative measurement of 1-84 PTH for unilateral neck exploration of primary hyperparathyroidism". World J Surg. 20 (7): 835–9, discussion 839–40. PMID 8678959.
- ↑ Prasannan S, Davies G, Bochner M, Kollias J, Malycha P (2007). "Minimally invasive parathyroidectomy using surgeon-performed ultrasound and sestamibi". ANZ J Surg. 77 (9): 774–7. doi:10.1111/j.1445-2197.2007.04227.x. PMID 17685957.
- ↑ Gómez-Ramírez J, Sancho-Insenser JJ, Pereira JA, Jimeno J, Munné A, Sitges-Serra A (2010). "Impact of thyroid nodular disease on 99mTc-sestamibi scintigraphy in patients with primary hyperparathyroidism". Langenbecks Arch Surg. 395 (7): 929–33. doi:10.1007/s00423-010-0680-8. PMID 20625763.
- ↑ Billotey C, Sarfati E, Aurengo A, Duet M, Mündler O, Toubert ME; et al. (1996). "Advantages of SPECT in technetium-99m-sestamibi parathyroid scintigraphy". J Nucl Med. 37 (11): 1773–8. PMID 8917173.
- ↑ Civelek AC, Ozalp E, Donovan P, Udelsman R (2002). "Prospective evaluation of delayed technetium-99m sestamibi SPECT scintigraphy for preoperative localization of primary hyperparathyroidism". Surgery. 131 (2): 149–57. PMID 11854692.
- ↑ Strand SE, Ivanovic M, Erlandsson K, Franceschi D, Button T, Sjögren K; et al. (1994). "Small animal imaging with pinhole single-photon emission computed tomography". Cancer. 73 (3 Suppl): 981–4. PMID 8306288.
- ↑ Jaszczak RJ, Li J, Wang H, Zalutsky MR, Coleman RE (1994). "Pinhole collimation for ultra-high-resolution, small-field-of-view SPECT". Phys Med Biol. 39 (3): 425–37. PMID 15551591.
- ↑ Schachter PP, Issa N, Shimonov M, Czerniak A, Lorberboym M (2004). "Early, postinjection MIBI-SPECT as the only preoperative localizing study for minimally invasive parathyroidectomy". Arch Surg. 139 (4): 433–7. doi:10.1001/archsurg.139.4.433. PMID 15078713.
- ↑ Perez-Monte JE, Brown ML, Shah AN, Ranger NT, Watson CG, Carty SE; et al. (1996). "Parathyroid adenomas: accurate detection and localization with Tc-99m sestamibi SPECT". Radiology. 201 (1): 85–91. doi:10.1148/radiology.201.1.8816526. PMID 8816526.
- ↑ Spanu A, Falchi A, Manca A, Marongiu P, Cossu A, Pisu N; et al. (2004). "The usefulness of neck pinhole SPECT as a complementary tool to planar scintigraphy in primary and secondary hyperparathyroidism". J Nucl Med. 45 (1): 40–8. PMID 14734671.
- ↑ Carlier T, Oudoux A, Mirallié E, Seret A, Daumy I, Leux C, Bodet-Milin C, Kraeber-Bodéré F, Ansquer C (2008). "99mTc-MIBI pinhole SPECT in primary hyperparathyroidism: comparison with conventional SPECT, planar scintigraphy and ultrasonography". Eur. J. Nucl. Med. Mol. Imaging. 35 (3): 637–43. doi:10.1007/s00259-007-0625-9. PMC 2964350. PMID 17960377.
- ↑ Nguyen BD (1999). "Parathyroid imaging with Tc-99m sestamibi planar and SPECT scintigraphy". Radiographics. 19 (3): 601–14, discussion 615-6. doi:10.1148/radiographics.19.3.g99ma10601. PMID 10336191.
- ↑ Lindqvist V, Jacobsson H, Chandanos E, Bäckdahl M, Kjellman M, Wallin G (2009). "Preoperative 99Tc(m)-sestamibi scintigraphy with SPECT localizes most pathologic parathyroid glands". Langenbecks Arch Surg. 394 (5): 811–5. doi:10.1007/s00423-009-0536-2. PMID 19578871.
- ↑ Wimmer G, Profanter C, Kovacs P, Sieb M, Gabriel M, Putzer D; et al. (2010). "CT-MIBI-SPECT image fusion predicts multiglandular disease in hyperparathyroidism". Langenbecks Arch Surg. 395 (1): 73–80. doi:10.1007/s00423-009-0545-1. PMID 19705144.
- ↑ Tang BN, Moreno-Reyes R, Blocklet D, Corvilain B, Cappello M, Delpierre I; et al. (2008). "Accurate pre-operative localization of pathological parathyroid glands using 11C-methionine PET/CT". Contrast Media Mol Imaging. 3 (4): 157–63. doi:10.1002/cmmi.243. PMID 18781582.
- ↑ Weber T, Maier-Funk C, Ohlhauser D, Hillenbrand A, Cammerer G, Barth TF; et al. (2013). "Accurate preoperative localization of parathyroid adenomas with C-11 methionine PET/CT". Ann Surg. 257 (6): 1124–8. doi:10.1097/SLA.0b013e318289b345. PMID 23478517.
- ↑ Traub-Weidinger T, Mayerhoefer ME, Koperek O, Mitterhauser M, Duan H, Karanikas G; et al. (2014). "11C-methionine PET/CT imaging of 99mTc-MIBI-SPECT/CT-negative patients with primary hyperparathyroidism and previous neck surgery". J Clin Endocrinol Metab. 99 (11): 4199–205. doi:10.1210/jc.2014-1267. PMID 25029418.
- ↑ Wood K, Dhital S, Chen H, Sippel RS (2012). "What is the utility of distal forearm DXA in primary hyperparathyroidism?". Oncologist. 17 (3): 322–5. doi:10.1634/theoncologist.2011-0285. PMC 3316917. PMID 22258698.
- ↑ Nussbaum SR, Thompson AR, Hutcheson KA, Gaz RD, Wang CA (1988). "Intraoperative measurement of parathyroid hormone in the surgical management of hyperparathyroidism". Surgery. 104 (6): 1121–7. PMID 3194839.
- ↑ Bergenfelz A, Isaksson A, Ahrén B (1994). "Intraoperative monitoring of intact PTH during surgery for primary hyperparathyroidism". Langenbecks Arch Chir. 379 (1): 50–3. PMID 8145618.
- ↑ Irvin III, George L.; Dembrow, Victor D.; Prudhomme, David L. (December 1993). "Clinical usefulness of an intraoperative "quick parathyroid hormone" assay". Surgery. 114 (6): 1019–1023.
- ↑ Bergenfelz A, Isaksson A, Lindblom P, Westerdahl J, Tibblin S (1998). "Measurement of parathyroid hormone in patients with primary hyperparathyroidism undergoing first and reoperative surgery". Br J Surg. 85 (8): 1129–32. doi:10.1046/j.1365-2168.1998.00824.x. PMID 9718013.
- ↑ Boggs JE, Irvin GL, Molinari AS, Deriso GT (1996). "Intraoperative parathyroid hormone monitoring as an adjunct to parathyroidectomy" (PDF). Surgery. 120 (6): 954–8. doi:10.1016/S0039-6060(96)80040-7. PMID 8957480.
- ↑ Westerdahl J, Lindblom P, Bergenfelz A (2002). "Measurement of intraoperative parathyroid hormone predicts long-term operative success". Arch Surg. 137 (2): 186–90. doi:10.1001/archsurg.137.2.186. PMID 11822958.
- ↑ Powell AC, Alexander HR, Chang R, Marx SJ, Skarulis M, Pingpank JF; et al. (2009). "Reoperation for parathyroid adenoma: a contemporary experience". Surgery. 146 (6): 1144–55. doi:10.1016/j.surg.2009.09.015. PMC 3467310. PMID 19958942.
- ↑ Miller DL, Chang R, Doppman JL, Norton JA (1989). "Localization of parathyroid adenomas: superselective arterial DSA versus superselective conventional angiography". Radiology. 170 (3 Pt 2): 1003–6. doi:10.1148/radiology.170.3.2644666. PMID 2644666.