Sandbox : anmol: Difference between revisions
(→SPECT) |
|||
| Line 59: | Line 59: | ||
*Parathyroid carcinoma | *Parathyroid carcinoma | ||
*Familial isloated hyperparathyroidism | *Familial isloated hyperparathyroidism | ||
*Radiation exposure (due to development of parathyroid adenoma or parathyroid hyperplasia) | *Radiation exposure (due to development of parathyroid adenoma or parathyroid hyperplasia) | ||
*Celiac disease | *Celiac disease | ||
===Genetic causes=== | ===Genetic causes=== | ||
*HRPT2 gene mutations: | *HRPT2 gene mutations: | ||
**HRPT2 gene code for parafibromin protein. | **HRPT2 gene code for parafibromin protein. | ||
**HRPT2 gene mutations are found in a type of familial hyperparathyroidism, hyperparathyroidism-jaw tumor (HPT-JT) syndrome. | **HRPT2 gene mutations are found in a type of familial hyperparathyroidism, hyperparathyroidism-jaw tumor (HPT-JT) syndrome. | ||
**HRTP2 gene mutations increases risk of parathyroid carcinoma. | **HRTP2 gene mutations increases risk of parathyroid carcinoma. | ||
*Cyclin D1 gene (CCND1)/PRAD1 gene: | *Cyclin D1 gene (CCND1)/PRAD1 gene: | ||
**PRAD1 (parathyroid adenoma 1) is a protooncogene located on chromosome 11q13. | **PRAD1 (parathyroid adenoma 1) is a protooncogene located on chromosome 11q13. | ||
**Cyclin D1 gene translocation and oncogene action observerd in 8% of adenomas | **Cyclin D1 gene translocation and oncogene action observerd in 8% of adenomas | ||
**Cyclin D1 gene overexpression is pbserved in 20% to 40% of parathyroid adenomas | **Cyclin D1 gene overexpression is pbserved in 20% to 40% of parathyroid adenomas | ||
*MEN1 gene:<ref name="pmid19373510">{{cite journal| author=Westin G, Björklund P, Akerström G| title=Molecular genetics of parathyroid disease. | journal=World J Surg | year= 2009 | volume= 33 | issue= 11 | pages= 2224-33 | pmid=19373510 | doi=10.1007/s00268-009-0022-6 | pmc= | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=19373510 | *MEN1 gene:<ref name="pmid19373510">{{cite journal| author=Westin G, Björklund P, Akerström G| title=Molecular genetics of parathyroid disease. | journal=World J Surg | year= 2009 | volume= 33 | issue= 11 | pages= 2224-33 | pmid=19373510 | doi=10.1007/s00268-009-0022-6 | pmc= | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=19373510 }} </ref> | ||
**MEN1 is a tumor supressor gene on chronosome 11q13. | **MEN1 is a tumor supressor gene on chronosome 11q13. | ||
**Somatic loss of single MEN1 allele is observed in 25% to 40% of sporadic parathyroid adenomas. | **Somatic loss of single MEN1 allele is observed in 25% to 40% of sporadic parathyroid adenomas. | ||
| Line 78: | Line 78: | ||
Causes of secondary hyperparathyroidism are as follows: | Causes of secondary hyperparathyroidism are as follows: | ||
===Common causes=== | ===Common causes=== | ||
*Chronic renal failure (leading to parathyroid hyperplasia) | *Chronic renal failure (leading to parathyroid hyperplasia) | ||
*Vitamin D deficiency | *Vitamin D deficiency | ||
===Less common causes=== | ===Less common causes=== | ||
*Severe calcium deficiency | *Severe calcium deficiency | ||
*Gastric bypass surgery, particularly roux-en-Y gastric bypass (RYGBP) | *Gastric bypass surgery, particularly roux-en-Y gastric bypass (RYGBP) | ||
*Malabsorption syndrome | *Malabsorption syndrome | ||
==Causes of tertiary hyperparathyroidism== | ==Causes of tertiary hyperparathyroidism== | ||
| Line 90: | Line 90: | ||
===Common causes=== | ===Common causes=== | ||
*Chronic renal failure (leading to parathyroid hyperplasia) | *Chronic renal failure (leading to parathyroid hyperplasia) | ||
*Renal transplant patients | *Renal transplant patients | ||
===Less common cause=== | ===Less common cause=== | ||
| Line 110: | Line 110: | ||
*Familial hypocalciuric hypercalcemia | *Familial hypocalciuric hypercalcemia | ||
*Hyperparathyroid-jaw tumor syndrome | *Hyperparathyroid-jaw tumor syndrome | ||
*Pancreatitis | *Pancreatitis | ||
=Natural history, Prognosis and Complications= | =Natural history, Prognosis and Complications= | ||
==Natural history== | ==Natural history== | ||
*Primary hyperparathyroidism usually develops in the fifth decade of life, in post-menopausal women and starts as asymptomatic hypercalcemia in presence of increased parathyroid hormone. | *Primary hyperparathyroidism usually develops in the fifth decade of life, in post-menopausal women and starts as asymptomatic hypercalcemia in presence of increased parathyroid hormone. | ||
*If left untreated, some of patients with primary hyperparathyroidism may commonly develop marked hypercalcemia, marked hypercalciuria, cortical bone demineralization and nephrolithiasis. | *If left untreated, some of patients with primary hyperparathyroidism may commonly develop marked hypercalcemia, marked hypercalciuria, cortical bone demineralization and nephrolithiasis. | ||
*Secondary hyperparathyroidism arise in the early course of chronic renal failure. As renal failure progress, secondary hyperparathyroidism becomes more notable. | *Secondary hyperparathyroidism arise in the early course of chronic renal failure. As renal failure progress, secondary hyperparathyroidism becomes more notable. | ||
*Secondary hyperparathyroidism leads to vascular calcification due to elevated calcium and phosphorus levels. This is strongly associated with increase in morbidity and mortality. | *Secondary hyperparathyroidism leads to vascular calcification due to elevated calcium and phosphorus levels. This is strongly associated with increase in morbidity and mortality. | ||
*If left untreated, secondary hyperparathyroidism carries an increased risk of vascular calcification with increasing age and duration of dialysis in patients. | *If left untreated, secondary hyperparathyroidism carries an increased risk of vascular calcification with increasing age and duration of dialysis in patients. | ||
*Tertiary hyperparathyroidism usually develops in post renal transplant patients. | *Tertiary hyperparathyroidism usually develops in post renal transplant patients. | ||
*If left untreated, tertiary hyperparathyroidism in post renal transplant patients may carry the risk of amyloid deposition, calciphylaxis, destructive or erosive spondyloarthropathy, osteonecrosis, and musculoskeletal infections. | *If left untreated, tertiary hyperparathyroidism in post renal transplant patients may carry the risk of amyloid deposition, calciphylaxis, destructive or erosive spondyloarthropathy, osteonecrosis, and musculoskeletal infections. | ||
| Line 127: | Line 127: | ||
===Primary hyperparathyroidism=== | ===Primary hyperparathyroidism=== | ||
Majority of complications of primary hyperparathyroidism are due to hypercalcemia. Common complications of primary hyperparathyroidism include: | Majority of complications of primary hyperparathyroidism are due to hypercalcemia. Common complications of primary hyperparathyroidism include: | ||
*Bone related complication: | *Bone related complication: | ||
**Brown tumor | **Brown tumor | ||
**Osteitis fibrous cystica | **Osteitis fibrous cystica | ||
**Osteoporosis | **Osteoporosis | ||
*Cardiac complications: | *Cardiac complications: | ||
**Aortic and mitral valve calcification | **Aortic and mitral valve calcification | ||
**Calcific deposits in the myocardium | **Calcific deposits in the myocardium | ||
| Line 137: | Line 137: | ||
*Endocrine complications:<ref name="pmid22874807">{{cite journal |vauthors=Bai HX, Giefer M, Patel M, Orabi AI, Husain SZ |title=The association of primary hyperparathyroidism with pancreatitis |journal=J. Clin. Gastroenterol. |volume=46 |issue=8 |pages=656–61 |year=2012 |pmid=22874807 |pmc=4428665 |doi=10.1097/MCG.0b013e31825c446c |url=}}</ref> | *Endocrine complications:<ref name="pmid22874807">{{cite journal |vauthors=Bai HX, Giefer M, Patel M, Orabi AI, Husain SZ |title=The association of primary hyperparathyroidism with pancreatitis |journal=J. Clin. Gastroenterol. |volume=46 |issue=8 |pages=656–61 |year=2012 |pmid=22874807 |pmc=4428665 |doi=10.1097/MCG.0b013e31825c446c |url=}}</ref> | ||
**Pancreatitis | **Pancreatitis | ||
*Gastrointestinal complications: | *Gastrointestinal complications: | ||
**Peptic ulcer disease | **Peptic ulcer disease | ||
*Metabolic complications: | *Metabolic complications:<ref name="pmid3878002">{{cite journal |vauthors=Corlew DS, Bryda SL, Bradley EL, DiGirolamo M |title=Observations on the course of untreated primary hyperparathyroidism |journal=Surgery |volume=98 |issue=6 |pages=1064–71 |year=1985 |pmid=3878002 |doi= |url=}}</ref><ref name="pmid11493580">{{cite journal| author=Lips P| title=Vitamin D deficiency and secondary hyperparathyroidism in the elderly: consequences for bone loss and fractures and therapeutic implications. | journal=Endocr Rev | year= 2001 | volume= 22 | issue= 4 | pages= 477-501 | pmid=11493580 | doi=10.1210/edrv.22.4.0437 | pmc= | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=11493580 }} </ref> | ||
**Hypercalcemic crisis | **Hypercalcemic crisis | ||
**Osteomalacia | **Osteomalacia | ||
*Neuromuscular complications: | *Neuromuscular complications: | ||
**Neuropathic muscle disease | **Neuropathic muscle disease | ||
*Pregnancy related complications: | *Pregnancy related complications: | ||
**Neonatal hypoparathyroidism | **Neonatal hypoparathyroidism | ||
*Psychiatric complications: | *Psychiatric complications: | ||
**Anxiety | **Anxiety | ||
**Cognitive dysfunction including verbal memory and nonverbal abstraction | **Cognitive dysfunction including verbal memory and nonverbal abstraction | ||
| Line 153: | Line 153: | ||
**Lack of concentration | **Lack of concentration | ||
**Sleep disturbances | **Sleep disturbances | ||
*Renal complications:<ref name="pmid12412783">{{cite journal |vauthors=Peacock M |title=Primary hyperparathyroidism and the kidney: biochemical and clinical spectrum |journal=J. Bone Miner. Res. |volume=17 Suppl 2 |issue= |pages=N87–94 |year=2002 |pmid=12412783 |doi= | *Renal complications:<ref name="pmid12412783">{{cite journal |vauthors=Peacock M |title=Primary hyperparathyroidism and the kidney: biochemical and clinical spectrum |journal=J. Bone Miner. Res. |volume=17 Suppl 2 |issue= |pages=N87–94 |year=2002 |pmid=12412783 |doi= |url=}}</ref> | ||
**Hypercalciuria | **Hypercalciuria | ||
**Nephrolithiasis | **Nephrolithiasis | ||
**Nephrocalcinosis | **Nephrocalcinosis | ||
**Renal insufficiency (impairement of GFR) | **Renal insufficiency (impairement of GFR) | ||
*Rheumatologic complications: | *Rheumatologic complications: | ||
**Gout | **Gout | ||
**Osteoarthritis | **Osteoarthritis | ||
| Line 165: | Line 165: | ||
===Secondary hyperparathyroidism=== | ===Secondary hyperparathyroidism=== | ||
Complications of secondary hyperparathyroidism includes: | Complications of secondary hyperparathyroidism includes: | ||
*Cardiovascular complications: | *Cardiovascular complications: | ||
**Impaired left ventricular diastolic function | **Impaired left ventricular diastolic function | ||
**Left ventricular hypertrophy | **Left ventricular hypertrophy | ||
*Hematologic complication: | *Hematologic complication: | ||
**Platlet function inhibition | **Platlet function inhibition | ||
*Metabolic complicattions: | *Metabolic complicattions: | ||
**Metabolic syndrome | **Metabolic syndrome | ||
*Musculoskeletal complications: | *Musculoskeletal complications: | ||
**Renal Osteodystrophy | **Renal Osteodystrophy | ||
***Brown cysts | ***Brown cysts | ||
| Line 179: | Line 179: | ||
***Osteoporosis | ***Osteoporosis | ||
***Osteosclerosis | ***Osteosclerosis | ||
*Neurologic complications: | *Neurologic complications: | ||
**Electroencephalogram abnormalities | **Electroencephalogram abnormalities | ||
**Uremic neuropathy | **Uremic neuropathy | ||
*Neuromuscular complications: | *Neuromuscular complications: | ||
**Neuropathic muscle disease | **Neuropathic muscle disease | ||
*System non-specific complications: | *System non-specific complications: | ||
**Metastatic calcifications | **Metastatic calcifications | ||
===Tertiary hyperparathyroidism=== | ===Tertiary hyperparathyroidism=== | ||
Complications of tertiary hyperparathyroidism post renal transplantation includes:<ref name="pmid12714225">{{cite journal |vauthors=Jevtic V |title=Imaging of renal osteodystrophy |journal=Eur J Radiol |volume=46 |issue=2 |pages=85–95 |year=2003 |pmid=12714225 |doi= 10.1016/S0720-048X(03)00072-X|url=http://www.sciencedirect.com/science/article/pii/S0720048X0300072X?via%3Dihub}}</ref> | Complications of tertiary hyperparathyroidism post renal transplantation includes:<ref name="pmid12714225">{{cite journal |vauthors=Jevtic V |title=Imaging of renal osteodystrophy |journal=Eur J Radiol |volume=46 |issue=2 |pages=85–95 |year=2003 |pmid=12714225 |doi= 10.1016/S0720-048X(03)00072-X|url=http://www.sciencedirect.com/science/article/pii/S0720048X0300072X?via%3Dihub}}</ref> | ||
*Metabolic complications: | *Metabolic complications: | ||
**Calciphylaxis | **Calciphylaxis | ||
*Musculoskeletal complications: | *Musculoskeletal complications: | ||
**Musculoskeletal infections | **Musculoskeletal infections | ||
**Osteonecrosis | **Osteonecrosis | ||
*Neuromuscular complications: | *Neuromuscular complications: | ||
**Neuropathic muscle disease | **Neuropathic muscle disease | ||
*Renal complications: | *Renal complications: | ||
**Nephrolithiasis | **Nephrolithiasis | ||
*Rheumatologic complications: | *Rheumatologic complications: | ||
**Destructive or erosive spondyloarthropathy | **Destructive or erosive spondyloarthropathy | ||
*System non-specific complications: | *System non-specific complications: | ||
| Line 212: | Line 212: | ||
*Hyperphosphatemia and metastatic calcification results due elevated product of serum calcium and serum phosphorus. Both conditions are present in patients with secondary hyperparathyroidism in presence of end stage renal disease. This leads to a significant increase in morbidity and mortality. Aggressive control of hyperphosphatemia may improve prognosis<ref name="pmid9531176">{{cite journal |vauthors=Block GA, Hulbert-Shearon TE, Levin NW, Port FK |title=Association of serum phosphorus and calcium x phosphate product with mortality risk in chronic hemodialysis patients: a national study |journal=Am. J. Kidney Dis. |volume=31 |issue=4 |pages=607–17 |year=1998 |pmid=9531176 |doi= |url=}}</ref>. | *Hyperphosphatemia and metastatic calcification results due elevated product of serum calcium and serum phosphorus. Both conditions are present in patients with secondary hyperparathyroidism in presence of end stage renal disease. This leads to a significant increase in morbidity and mortality. Aggressive control of hyperphosphatemia may improve prognosis<ref name="pmid9531176">{{cite journal |vauthors=Block GA, Hulbert-Shearon TE, Levin NW, Port FK |title=Association of serum phosphorus and calcium x phosphate product with mortality risk in chronic hemodialysis patients: a national study |journal=Am. J. Kidney Dis. |volume=31 |issue=4 |pages=607–17 |year=1998 |pmid=9531176 |doi= |url=}}</ref>. | ||
*Prognosis of tertiary hyperparathyroidism is generally good after resection of abnormal hyperplastic gland. | *Prognosis of tertiary hyperparathyroidism is generally good after resection of abnormal hyperplastic gland. | ||
=ECG= | =ECG= | ||
There are no CT scan findings associated with hyperparathyroidism. However, a CT scan may be helpful in the diagnosis of cardiac complications of hyperparathyroidism. | There are no CT scan findings associated with hyperparathyroidism. However, a CT scan may be helpful in the diagnosis of cardiac complications of hyperparathyroidism. | ||
Findings on ECG are due to hypercalcemia and includes: | Findings on ECG are due to hypercalcemia and includes: | ||
*ST segment - ST segment is short in patients with hyperparathyroidism when compared to normocalcemic patients. This represents a decrease in systolic interval. | *ST segment - ST segment is short in patients with hyperparathyroidism when compared to normocalcemic patients. This represents a decrease in systolic interval. | ||
*QRS complex - QRS complex has an increased amplitudein patients with hyperparathyroidism when compared to normocalcemic patients. This represents an increase in ventricular muscle mass. | *QRS complex - QRS complex has an increased amplitudein patients with hyperparathyroidism when compared to normocalcemic patients. This represents an increase in ventricular muscle mass. | ||
| Line 226: | Line 226: | ||
|- | |- | ||
| | | | ||
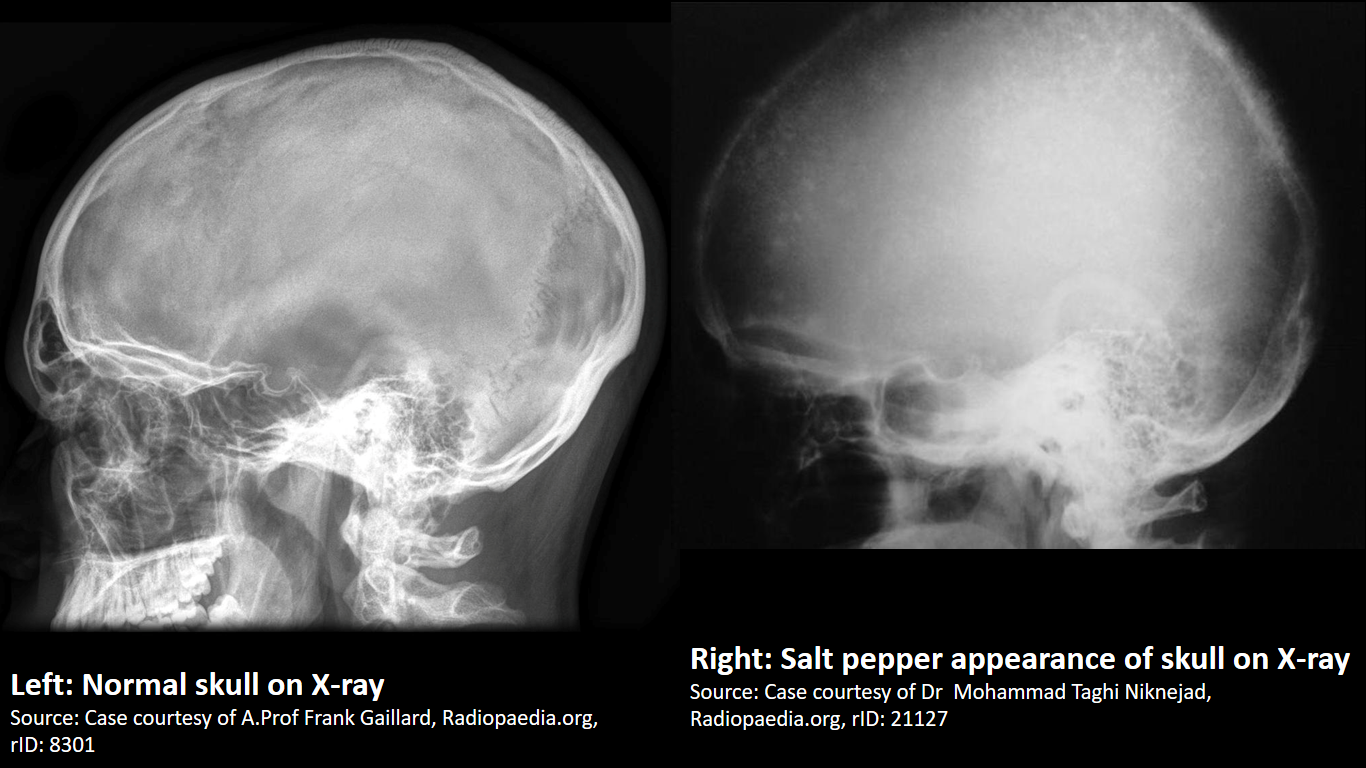
Finding in primary hyperparathyroidism includes: | Finding in primary hyperparathyroidism includes: | ||
*Subperiosteal bone resorption | *Subperiosteal bone resorption | ||
**Classically affects the radial aspects of the proximal and middle phalanges of the 2nd and 3rd fingers | **Classically affects the radial aspects of the proximal and middle phalanges of the 2nd and 3rd fingers | ||
| Line 251: | Line 251: | ||
*Chondrocalcinosis | *Chondrocalcinosis | ||
X-ray is the preferred imaging for diagnosis of secondary hyperparathyroidism as majority of findings are radiological. | X-ray is the preferred imaging for diagnosis of secondary hyperparathyroidism as majority of findings are radiological. | ||
Findings in secondary and tertiary hyperparathyroidism are often associated with the osteosclerosis of renal osteodystrophy, and the osteomalacia of vitamin D deficiency: | Findings in secondary and tertiary hyperparathyroidism are often associated with the osteosclerosis of renal osteodystrophy, and the osteomalacia of vitamin D deficiency: | ||
*Subperiosteal bone resorption | *Subperiosteal bone resorption | ||
| Line 283: | Line 283: | ||
=CT scan= | =CT scan= | ||
*Good quality preoperative evaluation favors post operative results. | *Good quality preoperative evaluation favors post operative results. | ||
*4-Dimentional CT scan is an investigation for preoperative localizing of hyperfunctioning pituitary gland. | *4-Dimentional CT scan is an investigation for preoperative localizing of hyperfunctioning pituitary gland. | ||
*4D-CT may be used for preoperative localization of hyper-functioning parathyroid glands in hyperparathyroidism. 4D-CT is significantly more sensitive than sestamibi imaging and ultrasound for precise (quadrant) localization of hyper-functioning parathyroid glands. | *4D-CT may be used for preoperative localization of hyper-functioning parathyroid glands in hyperparathyroidism. 4D-CT is significantly more sensitive than sestamibi imaging and ultrasound for precise (quadrant) localization of hyper-functioning parathyroid glands. | ||
*The name 4D-CT refers to 3-dimensional CT scanning plus additional dimension of changes observed with respect to time as perfusion of contrast occurs. The principle is similar to CT angiography. | *The name 4D-CT refers to 3-dimensional CT scanning plus additional dimension of changes observed with respect to time as perfusion of contrast occurs. The principle is similar to CT angiography. | ||
*4D-CT provides extremely detailed images of neck in multiple planes and enables the visualization of difference in hyper-functioning parathyroid gland compared with normal parathyroid glands and other structures in the neck on the basis on perfusion characteristics ( rapid uptake and washout). | *4D-CT provides extremely detailed images of neck in multiple planes and enables the visualization of difference in hyper-functioning parathyroid gland compared with normal parathyroid glands and other structures in the neck on the basis on perfusion characteristics ( rapid uptake and washout). | ||
*4D-CT has a sensitive of 88% in preoperative lateralizing hyper-functioning parathyroid glands to one side of neck when compared to sestamibi imaging (68% to 86% sensitive) and ultrasound (61% to 88% sensitive). | *4D-CT has a sensitive of 88% in preoperative lateralizing hyper-functioning parathyroid glands to one side of neck when compared to sestamibi imaging (68% to 86% sensitive) and ultrasound (61% to 88% sensitive). | ||
*4D-CT has a sensitive of 79-88% in preoperative localizing the hyper-functioning parathyroid gland to the correct quadrant of the neck (right inferior, right superior, left inferior, or left superior) when compared to sestamibi imaging (33% to 40% sensitive) and ultrasound (29% to 48% sensitive). | *4D-CT has a sensitive of 79-88% in preoperative localizing the hyper-functioning parathyroid gland to the correct quadrant of the neck (right inferior, right superior, left inferior, or left superior) when compared to sestamibi imaging (33% to 40% sensitive) and ultrasound (29% to 48% sensitive). | ||
*4D-CT has a specificity of 75-100% in preoperative localizing the hyper-functioning parathyroid gland. | *4D-CT has a specificity of 75-100% in preoperative localizing the hyper-functioning parathyroid gland. | ||
*4D-CT enables an improved planning preoperativively, particularly in case of reoperation. | *4D-CT enables an improved planning preoperativively, particularly in case of reoperation. | ||
*A modified technique of 4D-CT/Ultrasound (Mod 4D-CT/US) has a sensitivity of 94% and specificity of 96% for lateralizing the hyperfunctioning parathyroid glands to one side of the neck. Mod 4D-CT/US has a sensitivity of 82% and specificity of 93% for localizing the hyper-functioning parathyroid gland to the correct quadrant of the neck (right inferior, right superior, left inferior, or left superior). Mod 4D-CT/US has a positive predictive vaue of 92% for single-gland disease and 75% for multi-gland disease.Mod 4D-CT/US has a negative predictive value of 73% for single-gland disease and 92% multi-gland disease. | *A modified technique of 4D-CT/Ultrasound (Mod 4D-CT/US) has a sensitivity of 94% and specificity of 96% for lateralizing the hyperfunctioning parathyroid glands to one side of the neck. Mod 4D-CT/US has a sensitivity of 82% and specificity of 93% for localizing the hyper-functioning parathyroid gland to the correct quadrant of the neck (right inferior, right superior, left inferior, or left superior). Mod 4D-CT/US has a positive predictive vaue of 92% for single-gland disease and 75% for multi-gland disease.Mod 4D-CT/US has a negative predictive value of 73% for single-gland disease and 92% multi-gland disease. | ||
*The major disadvantage of 4D-CT is significant radiation exposure associated with scanning the patient multiple times. | *The major disadvantage of 4D-CT is significant radiation exposure associated with scanning the patient multiple times. | ||
=MRI= | =MRI= | ||
| Line 299: | Line 299: | ||
=Sestamibi scintigraphy= | =Sestamibi scintigraphy= | ||
*Technetium-99m-methoxyisobutylisonitrile (99mTc-sestamibi or MIBI) scintigraphy is the most popular investigation for preoperative localization of hyper-functioning parathyroid glands. | *Technetium-99m-methoxyisobutylisonitrile (99mTc-sestamibi or MIBI) scintigraphy is the most popular investigation for preoperative localization of hyper-functioning parathyroid glands. | ||
*Most of the sestamibi is retained in mitochondria of thyroid and abnormal parathyroid tissue and is a function of mitochondrial activity. | *Most of the sestamibi is retained in mitochondria of thyroid and abnormal parathyroid tissue and is a function of mitochondrial activity. | ||
*The basis of this "single-isotope, double-phase technique" is that sestamibi washes out of the thyroid more rapidly than from abnormal parathyroid tissue. | *The basis of this "single-isotope, double-phase technique" is that sestamibi washes out of the thyroid more rapidly than from abnormal parathyroid tissue. | ||
*As all parathyroid lesions does not retain sestamibi nor all thyroid tissue washes out quickly, subtraction imaging may be beneficial. | *As all parathyroid lesions does not retain sestamibi nor all thyroid tissue washes out quickly, subtraction imaging may be beneficial. | ||
{| class="wikitable" | |||
! colspan="4" |Factors influencing Sestamibi-SPECT scan | |||
|- | |||
| colspan="2" |Biological factors | |||
| | |||
|Sensitivity | |||
|- | |||
|Biochemical factors | |||
|Serum calcium | |||
|Higher calcium | |||
|Increased | |||
|- | |||
| | |||
|Serum Parathyroid hormone | |||
|Higher | |||
|Increased | |||
|- | |||
| | |||
|Vitamin D | |||
| | |||
| | |||
|- | |||
| | |||
| | |||
| | |||
| | |||
|} | |||
==References== | ==References== | ||
<references /> | |||
Revision as of 15:54, 31 August 2017
|
Hyperparathyroidism Microchapters |
|
Diagnosis |
|---|
|
Treatment |
|
Case Studies |
|
Sandbox : anmol On the Web |
|
American Roentgen Ray Society Images of Sandbox : anmol |
Editor-In-Chief: C. Michael Gibson, M.S., M.D. [1]; Associate Editor(s)-in-Chief: Anmol Pitliya, M.B.B.S. M.D.[2]
Classification
| Classification of hyperparathyridism | |||
|---|---|---|---|
| Features | Primary hyperparathyroidism | Secondary hyperparathyroidism | Tertiary hyperparathyroidism |
| Pathology | Hyperfunction of parathyroid cells due to hyperplasia, adenoma or carcinoma. | Physiological stimulation of parathyroid in response to hypocalcaemia. | Following long term physiological stimulation leading to hyperplasia. |
| Cause | |||
| Associations | May be associated with multiple endocrine neoplasia. | Usually due to chronic renal failure or other causes of Vitamin D deficiency. | Seen in chronic renal failure. |
| Serum calcium | High | Low/Normal | High |
| Serum phosphate | Low/Normal | High | High |
| Management | Usually surgery if symptomatic. Cincacalcet can be considered in those not fit for surgery. | Treatment of underlying cause. | Usually cinacalcet or surgery in those that don't respond. |
Causes
Overview
Hyperparathyroidism is caused by an increase in concentration of parathyroid hormone in serum. There are three type of hyperparathyroidism including primary, secondary and tertiary hyperparathyroidism. The are an array of different causes for all types of hyperparathyroidism.
Causes of Primary hyperparathyroidism
Causes of primary hyperparathyroidism are as follows:
Common causes
- Parathyroid adenoma
- Usually single gland affected
- Sometimes multiple gland affected
Less common causes
- Parathyroid hyperplasia
- Parathyroid carcinoma
- Familial isloated hyperparathyroidism
- Radiation exposure (due to development of parathyroid adenoma or parathyroid hyperplasia)
- Celiac disease
Genetic causes
- HRPT2 gene mutations:
- HRPT2 gene code for parafibromin protein.
- HRPT2 gene mutations are found in a type of familial hyperparathyroidism, hyperparathyroidism-jaw tumor (HPT-JT) syndrome.
- HRTP2 gene mutations increases risk of parathyroid carcinoma.
- Cyclin D1 gene (CCND1)/PRAD1 gene:
- PRAD1 (parathyroid adenoma 1) is a protooncogene located on chromosome 11q13.
- Cyclin D1 gene translocation and oncogene action observerd in 8% of adenomas
- Cyclin D1 gene overexpression is pbserved in 20% to 40% of parathyroid adenomas
- MEN1 gene:[1]
- MEN1 is a tumor supressor gene on chronosome 11q13.
- Somatic loss of single MEN1 allele is observed in 25% to 40% of sporadic parathyroid adenomas.
Causes of secondary hyperparathyroidism
Causes of secondary hyperparathyroidism are as follows:
Common causes
- Chronic renal failure (leading to parathyroid hyperplasia)
- Vitamin D deficiency
Less common causes
- Severe calcium deficiency
- Gastric bypass surgery, particularly roux-en-Y gastric bypass (RYGBP)
- Malabsorption syndrome
Causes of tertiary hyperparathyroidism
Causes of tertiary hyperparathyroidism are as follows:
Common causes
- Chronic renal failure (leading to parathyroid hyperplasia)
- Renal transplant patients
Less common cause
- Long standing celiac disease[2]
Pathogenesis
Associated conditions
- Hypercalcemia
- Chronic renal failure
- Osteitis fibrous cystica
- Osteoporosis
- Osteomalacia
- Osteoarthritis
- Brown tumor
- Multiple endocrine neoplasia type 1, type 2A, and type 4
- Familial isolated hyperparathyroidism
- Neonatal severe hyperparathyroidism
- Familial hypocalciuric hypercalcemia
- Hyperparathyroid-jaw tumor syndrome
- Pancreatitis
Natural history, Prognosis and Complications
Natural history
- Primary hyperparathyroidism usually develops in the fifth decade of life, in post-menopausal women and starts as asymptomatic hypercalcemia in presence of increased parathyroid hormone.
- If left untreated, some of patients with primary hyperparathyroidism may commonly develop marked hypercalcemia, marked hypercalciuria, cortical bone demineralization and nephrolithiasis.
- Secondary hyperparathyroidism arise in the early course of chronic renal failure. As renal failure progress, secondary hyperparathyroidism becomes more notable.
- Secondary hyperparathyroidism leads to vascular calcification due to elevated calcium and phosphorus levels. This is strongly associated with increase in morbidity and mortality.
- If left untreated, secondary hyperparathyroidism carries an increased risk of vascular calcification with increasing age and duration of dialysis in patients.
- Tertiary hyperparathyroidism usually develops in post renal transplant patients.
- If left untreated, tertiary hyperparathyroidism in post renal transplant patients may carry the risk of amyloid deposition, calciphylaxis, destructive or erosive spondyloarthropathy, osteonecrosis, and musculoskeletal infections.
Complications
Primary hyperparathyroidism
Majority of complications of primary hyperparathyroidism are due to hypercalcemia. Common complications of primary hyperparathyroidism include:
- Bone related complication:
- Brown tumor
- Osteitis fibrous cystica
- Osteoporosis
- Cardiac complications:
- Aortic and mitral valve calcification
- Calcific deposits in the myocardium
- Left ventricular hypertrophy
- Endocrine complications:[3]
- Pancreatitis
- Gastrointestinal complications:
- Peptic ulcer disease
- Metabolic complications:[4][5]
- Hypercalcemic crisis
- Osteomalacia
- Neuromuscular complications:
- Neuropathic muscle disease
- Pregnancy related complications:
- Neonatal hypoparathyroidism
- Psychiatric complications:
- Anxiety
- Cognitive dysfunction including verbal memory and nonverbal abstraction
- Depression
- Irritability
- Lack of concentration
- Sleep disturbances
- Renal complications:[6]
- Hypercalciuria
- Nephrolithiasis
- Nephrocalcinosis
- Renal insufficiency (impairement of GFR)
- Rheumatologic complications:
- Gout
- Osteoarthritis
- Pseudogout
Secondary hyperparathyroidism
Complications of secondary hyperparathyroidism includes:
- Cardiovascular complications:
- Impaired left ventricular diastolic function
- Left ventricular hypertrophy
- Hematologic complication:
- Platlet function inhibition
- Metabolic complicattions:
- Metabolic syndrome
- Musculoskeletal complications:
- Renal Osteodystrophy
- Brown cysts
- Osteitis fibrosa cystica
- Osteoporosis
- Osteosclerosis
- Renal Osteodystrophy
- Neurologic complications:
- Electroencephalogram abnormalities
- Uremic neuropathy
- Neuromuscular complications:
- Neuropathic muscle disease
- System non-specific complications:
- Metastatic calcifications
Tertiary hyperparathyroidism
Complications of tertiary hyperparathyroidism post renal transplantation includes:[7]
- Metabolic complications:
- Calciphylaxis
- Musculoskeletal complications:
- Musculoskeletal infections
- Osteonecrosis
- Neuromuscular complications:
- Neuropathic muscle disease
- Renal complications:
- Nephrolithiasis
- Rheumatologic complications:
- Destructive or erosive spondyloarthropathy
- System non-specific complications:
- Amyloid deposition
- Metastatic calcifications
Prognosis
- Prognosis of primary hyperparathyroidism is generally excellent after parathyroidectomy.
- The complications of primary hyperparathyroidism resolves after the treatment.
- Untreated complication of primary hyperparathyroidism may be fatal.[4]
- Effective treatment can reduce morbidity and mortality associated with uncontrolled secondary hyperparathyroidism.[8]
- Hyperphosphatemia and metastatic calcification results due elevated product of serum calcium and serum phosphorus. Both conditions are present in patients with secondary hyperparathyroidism in presence of end stage renal disease. This leads to a significant increase in morbidity and mortality. Aggressive control of hyperphosphatemia may improve prognosis[9].
- Prognosis of tertiary hyperparathyroidism is generally good after resection of abnormal hyperplastic gland.
ECG
There are no CT scan findings associated with hyperparathyroidism. However, a CT scan may be helpful in the diagnosis of cardiac complications of hyperparathyroidism. Findings on ECG are due to hypercalcemia and includes:
- ST segment - ST segment is short in patients with hyperparathyroidism when compared to normocalcemic patients. This represents a decrease in systolic interval.
- QRS complex - QRS complex has an increased amplitudein patients with hyperparathyroidism when compared to normocalcemic patients. This represents an increase in ventricular muscle mass.
- T wave - T wave is prolonged in patients with hyperparathyroidism when compared to normocalcemic patients.
X-ray
|
Finding in primary hyperparathyroidism includes:
X-ray is the preferred imaging for diagnosis of secondary hyperparathyroidism as majority of findings are radiological. Findings in secondary and tertiary hyperparathyroidism are often associated with the osteosclerosis of renal osteodystrophy, and the osteomalacia of vitamin D deficiency:
| |
 |
 |
 |
 |
CT scan
- Good quality preoperative evaluation favors post operative results.
- 4-Dimentional CT scan is an investigation for preoperative localizing of hyperfunctioning pituitary gland.
- 4D-CT may be used for preoperative localization of hyper-functioning parathyroid glands in hyperparathyroidism. 4D-CT is significantly more sensitive than sestamibi imaging and ultrasound for precise (quadrant) localization of hyper-functioning parathyroid glands.
- The name 4D-CT refers to 3-dimensional CT scanning plus additional dimension of changes observed with respect to time as perfusion of contrast occurs. The principle is similar to CT angiography.
- 4D-CT provides extremely detailed images of neck in multiple planes and enables the visualization of difference in hyper-functioning parathyroid gland compared with normal parathyroid glands and other structures in the neck on the basis on perfusion characteristics ( rapid uptake and washout).
- 4D-CT has a sensitive of 88% in preoperative lateralizing hyper-functioning parathyroid glands to one side of neck when compared to sestamibi imaging (68% to 86% sensitive) and ultrasound (61% to 88% sensitive).
- 4D-CT has a sensitive of 79-88% in preoperative localizing the hyper-functioning parathyroid gland to the correct quadrant of the neck (right inferior, right superior, left inferior, or left superior) when compared to sestamibi imaging (33% to 40% sensitive) and ultrasound (29% to 48% sensitive).
- 4D-CT has a specificity of 75-100% in preoperative localizing the hyper-functioning parathyroid gland.
- 4D-CT enables an improved planning preoperativively, particularly in case of reoperation.
- A modified technique of 4D-CT/Ultrasound (Mod 4D-CT/US) has a sensitivity of 94% and specificity of 96% for lateralizing the hyperfunctioning parathyroid glands to one side of the neck. Mod 4D-CT/US has a sensitivity of 82% and specificity of 93% for localizing the hyper-functioning parathyroid gland to the correct quadrant of the neck (right inferior, right superior, left inferior, or left superior). Mod 4D-CT/US has a positive predictive vaue of 92% for single-gland disease and 75% for multi-gland disease.Mod 4D-CT/US has a negative predictive value of 73% for single-gland disease and 92% multi-gland disease.
- The major disadvantage of 4D-CT is significant radiation exposure associated with scanning the patient multiple times.
MRI
MRI may be helpful in the preoperative evaluation of hype-functioning parathyroid glands.
SPECT
Sestamibi scintigraphy
- Technetium-99m-methoxyisobutylisonitrile (99mTc-sestamibi or MIBI) scintigraphy is the most popular investigation for preoperative localization of hyper-functioning parathyroid glands.
- Most of the sestamibi is retained in mitochondria of thyroid and abnormal parathyroid tissue and is a function of mitochondrial activity.
- The basis of this "single-isotope, double-phase technique" is that sestamibi washes out of the thyroid more rapidly than from abnormal parathyroid tissue.
- As all parathyroid lesions does not retain sestamibi nor all thyroid tissue washes out quickly, subtraction imaging may be beneficial.
| Factors influencing Sestamibi-SPECT scan | |||
|---|---|---|---|
| Biological factors | Sensitivity | ||
| Biochemical factors | Serum calcium | Higher calcium | Increased |
| Serum Parathyroid hormone | Higher | Increased | |
| Vitamin D | |||
References
- ↑ Westin G, Björklund P, Akerström G (2009). "Molecular genetics of parathyroid disease". World J Surg. 33 (11): 2224–33. doi:10.1007/s00268-009-0022-6. PMID 19373510.
- ↑ Maida MJ, Praveen E, Crimmins SR, Swift GL (2006). "Coeliac disease and primary hyperparathyroidism: an association?". Postgrad Med J. 82 (974): 833–5. doi:10.1136/pgmj.2006.045500. PMC 2653933. PMID 17148709.
- ↑ Bai HX, Giefer M, Patel M, Orabi AI, Husain SZ (2012). "The association of primary hyperparathyroidism with pancreatitis". J. Clin. Gastroenterol. 46 (8): 656–61. doi:10.1097/MCG.0b013e31825c446c. PMC 4428665. PMID 22874807.
- ↑ 4.0 4.1 Corlew DS, Bryda SL, Bradley EL, DiGirolamo M (1985). "Observations on the course of untreated primary hyperparathyroidism". Surgery. 98 (6): 1064–71. PMID 3878002.
- ↑ Lips P (2001). "Vitamin D deficiency and secondary hyperparathyroidism in the elderly: consequences for bone loss and fractures and therapeutic implications". Endocr Rev. 22 (4): 477–501. doi:10.1210/edrv.22.4.0437. PMID 11493580.
- ↑ Peacock M (2002). "Primary hyperparathyroidism and the kidney: biochemical and clinical spectrum". J. Bone Miner. Res. 17 Suppl 2: N87–94. PMID 12412783.
- ↑ Jevtic V (2003). "Imaging of renal osteodystrophy". Eur J Radiol. 46 (2): 85–95. doi:10.1016/S0720-048X(03)00072-X. PMID 12714225.
- ↑ Cunningham J, Locatelli F, Rodriguez M (2011). "Secondary hyperparathyroidism: pathogenesis, disease progression, and therapeutic options". Clin J Am Soc Nephrol. 6 (4): 913–21. doi:10.2215/CJN.06040710. PMID 21454719.
- ↑ Block GA, Hulbert-Shearon TE, Levin NW, Port FK (1998). "Association of serum phosphorus and calcium x phosphate product with mortality risk in chronic hemodialysis patients: a national study". Am. J. Kidney Dis. 31 (4): 607–17. PMID 9531176.