Sandbox:Hyperlipoproteinemia type5
|
Breast Cancer Microchapters |
|
Diagnosis |
|---|
|
Treatment |
|
Case Studies |
|
Sandbox:Hyperlipoproteinemia type5 On the Web |
|
American Roentgen Ray Society Images of Sandbox:Hyperlipoproteinemia type5 |
|
Risk calculators and risk factors for Sandbox:Hyperlipoproteinemia type5 |
Editor-In-Chief: C. Michael Gibson, M.S., M.D. [1]; Associate Editor(s)-in-Chief: Person 1, Person 2, Your Name
Overview
Historical Perspective
Classification
Pathophysiology
Causes
Differentiating Any Disease from other Diseases
Epidemiology and Demographics
Risk Factors
Screening
Natural History, Complications and Prognosis
A reduced HDL-C level is associate with ASCVD
Diagnosis
Diagnosis of HLP type 5 is usually by clinical presentation.
- History (including age of onset of symptomes in the patient and family members).
- Physical findings such as eruptive xanthomas and tendon xanthomas.
- Laboratory evaluation such as lipid levels and apolipoprotein assays.
History and Symptoms | Physical Examination | Laboratory Findings | Electrocardiogram | Chest X Ray | CT | MRI | Echocardiography or Ultrasound | Other Imaging Findings | Other Diagnostic Studies
Treatment
Medical Therapy | Surgery | Primary Prevention | Secondary Prevention | Cost-Effectiveness of Therapy | Future or Investigational Therapies
The evaluation and treatment decisions of type 5 HLP should be based on patient-centered and individual circumstances. Lifestyle therapies, such as appropriate nutrition and physical activity, are important elements of ASCVD risk reduction, with or without lipid-altering drug therapy. For patients in whom lipid-altering drug therapy is indicated, statin treatment is the primary pharmacologic modality for reducing ASCVD risk.
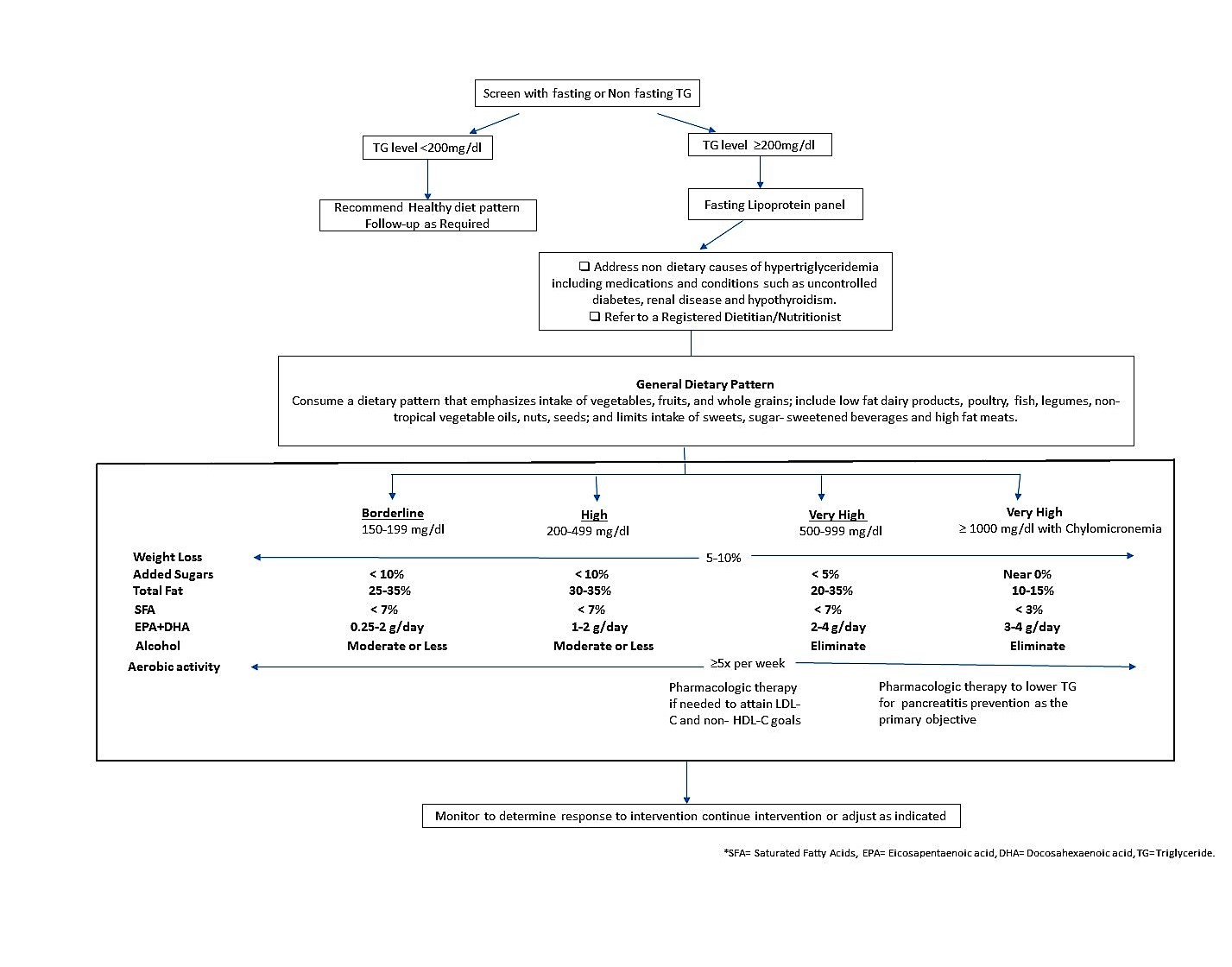
Clinical algorithm for screening and management of elevated TG[1]
Medical Therapy
When the triglyceride concentration is very high (≥500 mg/dL, and especially if ≥1000 mg/dL), the primary goal of therapy is to reduce the triglyceride level to <500 mg/dL for the intent of reducing the risk of pancreatitis.
| Triglyceride concentration | First line of therapy |
|---|---|
| ≥1000mg/dl | Triglyceride lowering agents such as ❑ Fibric acids ❑ High-dose [2 to 4 g/d] long-chain omega-3 fatty acids ❑ Nicotinic acid |
| 500-999mg/dl | ❑ Triglyceride lowering agents, ❑ Statins |
| 200-499mg/dl | Statin will generally be first-line drug therapy.If maximum tolerated statin therapy does not lower non-HDL-C below goal levels in patients with triglycerides 200 to 499 mg/dL, adding an agent that primarily lowers triglycerides may help to achieve atherogenic cholesterol goals. |
When triglycerides are between 200 and 499mg/dL, the primary targets of lipid therapy are non–HDL-C and LDL-C for the purpose of reducing ASCVD risk.
| Lipid treatment goals to reduce ASCVD risk[1] | ||
|---|---|---|
| Risk of ASCVD | Indication for drug therapy | Goal of drug therapy |
| Low ASCVD risk | Non HDL- C* level ≥190mg/dl LDL-C level ≥160mg/dl |
Non HDL- C level <130mg/dl LDL-C level <100mg/dl |
| Moderate ASCVD risk | Non HDL- C* level ≥160mg/dl LDL-C level ≥130mg/dl |
Non HDL- C level <130mg/dl LDL-C level <100mg/dl |
| High ASCVD risk | Non HDL- C level ≥130mg/dl LDL-C level ≥100mg/dl |
Non HDL- C level <130mg/dl LDL-C level <100mg/dl |
| Very high ASCVD risk | Non HDL- C level ≥100mg/dl LDL-C level ≥70mg/dl |
Non HDL- C level <100mg/dl LDL-C level <70mg/dl |
Non–HDL-C comprises the cholesterol carried by all atherogenic particles, including LDL, intermediatedensity lipoproteins, very low-density lipoproteins (VLDL) and VLDL remnants, chylomicron remnants, and lipoprotein.[2]
Secondary Prevention
- Lifestyle interventions are a key to efforts to reduce triglycerides that includes[1]
- weight loss if overweight or obese
- physical activity (≥ 150 minutes per week of moderate or higher intensity activity)
- Restriction of alcohol
- Restriction of sugar/refined carbohydrate intakes
- For patients with very high TG level (≥500 mg/dL),chylomicronemia will generally be present. For such patients, a low-fat diet (,15% of energy) may be helpful to reduce entry of new chylomicron particles into the circulation.[1]
- For patients with triglycerides <500 mg/dL, partial replacement of dietary carbohydrate (especially sugars and other refined carbohydrates) with a combination of unsaturated fats and proteins may help to reduce the triglyceride and non-HDL-C concentrations.
Case Studies
References
- ↑ 1.0 1.1 1.2 1.3 Jacobson TA, Ito MK, Maki KC, Orringer CE, Bays HE, Jones PH et al. (2015) National lipid association recommendations for patient-centered management of dyslipidemia: part 1--full report. J Clin Lipidol 9 (2):129-69. DOI:10.1016/j.jacl.2015.02.003 PMID: 25911072
- ↑ Bays HE, Jones PH, Orringer CE, Brown WV, Jacobson TA (2016) National Lipid Association Annual Summary of Clinical Lipidology 2016. J Clin Lipidol 10 (1 Suppl):S1-43. DOI:10.1016/j.jacl.2015.08.002 PMID: 26891998