ST elevation myocardial infarction percutaneous coronary intervention following fibrinolytic administration
| Myocardial infarction | |
 | |
|---|---|
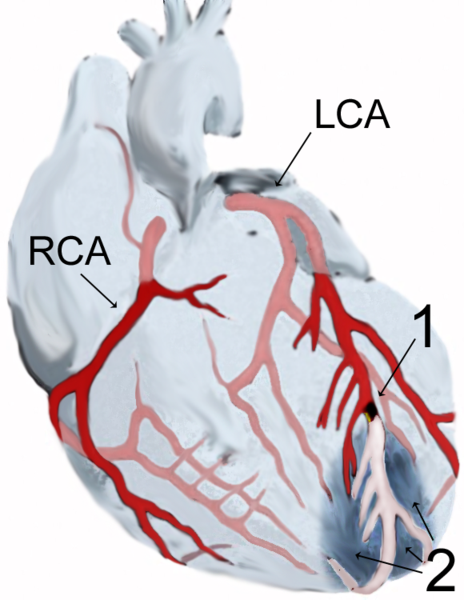
| Diagram of a myocardial infarction (2) of the tip of the anterior wall of the heart (an apical infarct) after occlusion (1) of a branch of the left coronary artery (LCA, right coronary artery = RCA). | |
| ICD-10 | I21-I22 |
| ICD-9 | 410 |
| DiseasesDB | 8664 |
| MedlinePlus | 000195 |
| eMedicine | med/1567 emerg/327 ped/2520 |
|
WikiDoc Resources for ST elevation myocardial infarction percutaneous coronary intervention following fibrinolytic administration |
|
Articles |
|---|
|
Media |
|
Evidence Based Medicine |
|
Clinical Trials |
|
|
|
Guidelines / Policies / Govt |
|
|
|
Books |
|
News |
|
Commentary |
|
Definitions |
|
Patient Resources / Community |
|
|
|
Healthcare Provider Resources |
|
Continuing Medical Education (CME) |
|
International |
|
|
|
Business |
|
Experimental / Informatics |
| Cardiology Network |
 Discuss ST elevation myocardial infarction percutaneous coronary intervention following fibrinolytic administration further in the WikiDoc Cardiology Network |
| Adult Congenital |
|---|
| Biomarkers |
| Cardiac Rehabilitation |
| Congestive Heart Failure |
| CT Angiography |
| Echocardiography |
| Electrophysiology |
| Cardiology General |
| Genetics |
| Health Economics |
| Hypertension |
| Interventional Cardiology |
| MRI |
| Nuclear Cardiology |
| Peripheral Arterial Disease |
| Prevention |
| Public Policy |
| Pulmonary Embolism |
| Stable Angina |
| Valvular Heart Disease |
| Vascular Medicine |
Editor-In-Chief: C. Michael Gibson, M.S., M.D. [1]
Associate Editor-In-Chief: Cafer Zorkun, M.D., Ph.D. [2]
Please Join in Editing This Page and Apply to be an Editor-In-Chief for this topic: There can be one or more than one Editor-In-Chief. You may also apply to be an Associate Editor-In-Chief of one of the subtopics below. Please mail us [3] to indicate your interest in serving either as an Editor-In-Chief of the entire topic or as an Associate Editor-In-Chief for a subtopic. Please be sure to attach your CV and or biographical sketch.
A. Percutaneous Coronary Intervention After Failed Fibrinolysis
Mechanism of Benefit
Pharmacological reperfusion with full dose fibrinolysis is not uniformly successful in restoring antegrade flow in the infarct artery. In such situations, a strategy of prompt coronary angiography with intent to perform PCI is frequently contemplated. In certain patients, such as those with cardiogenic shock (especially those less than 75 years of age), severe congestive heart failure / pulmonary edema, or hemodynamically compromising ventricular arrhythmias (regardless of age), a strategy of coronary angiography with intent to perform PCI is a useful approach regardless of the time since initiation of fibrinolytic therapy,
In patients who do not exhibit the clinical instability noted above, PCI may also be reasonable if there is clinical suspicion of failure of fibrinolysis. This is referred to as rescue PCI. Critical to the success of rescue PCI is the initial clinical identification of patients who are suspected of having failed reperfusion with full dose fibrinolysis.
Clinical Trial Data
MERLIN (Middlesbrough Early Revascularization to Limit INfarction) (n=307), REACT (Rescue Angioplasty versus Conservative Treatment or Repeat Thrombolysis) (n=427), and 3 meta analyses have refocused attention on rescue PCI.[1][2][3][4] This subject has been studied with fewer than 1000 patients enrolled in randomized trials. In the period between trials studying rescue PCI, there was a transition between angiographic and electrocardiographic diagnosis to detect failed reperfusion.
Importantly, in the earlier studies, rescue PCI was performed in infarct arteries with TIMI 0/1 flow, often after a protocol-mandated 90 minute angiogram. In MERLIN and REACT, however, patients were randomized if they had less than 50% ST segment elevation resolution at 60 or 90 minutes, respectively. Many patients had patent infarct arteries on angiography; only 54% of patients in MERLIN and 74% of patients in REACT (which required less than TIMI grade 3 flow for PCI) actually underwent PCI. From a procedural standpoint, stents have replaced balloon angioplasty, antiplatelet therapy has improved with the addition of a thienopyridine agent and often a GP IIb/IIIa receptor antagonist, and procedural success rates are higher.
Despite these historical differences, recent data support the initial observation that rescue PCI decreases adverse clinical events compared with medical therapy. In the Wijeysundera meta-analysis[5], there was a trend toward reduced mortality rates with rescue PCI from 10.4% to 7.3% (RR 0.69 [95% confidence interval (CI) 0.46 to 1.05]; p=0.09), reduced reinfarction rates from 10.7% to 6.1% (RR 0.58 [95% CI 0.35 to 0.97]; p=0.04), and reduced heart failure rates from 17.8% to 12.7% (RR 0.73 [95% CI 0.54 to 1.00]; p=0.05). These event rates suggest that high-risk patients were selected for enrollment, so these data do not inform the clinical community about the role of rescue PCI in lower-risk patients. Also, the benefits of rescue PCI need to be balanced against the risk.
There was an excess occurrence of stroke in 2 trials (10 events vs. 2 events), but the majority of the strokes were thromboembolic rather than hemorrhagic, and the sample size was small, so more data are needed to define this risk. There also was an increase in absolute risk of bleeding of 13%, suggesting that adjustments in antithrombotic medication dosing are needed to improve safety. It should be noted that the majority of patients who underwent rescue PCI received fibrinolytic therapy with streptokinase.
Side Effects
Guidelines (DO NOT EDIT)
Class I
1. A strategy of coronary angiography with intent to perform PCI (or emergency CABG) is recommended for patients who have received fibrinolytic therapy and have any of the following:
a. Cardiogenic shock in patients less than 75 years who are suitable candidates for revascularization (Level of Evidence: B)
b. Severe congestive heart failure and/or pulmonary edema (Killip class III) (Level of Evidence: B)
c. Hemodynamically compromising ventricular arrhythmias (Level of Evidence: C)
Class IIa
1. A strategy of coronary angiography with intent to perform PCI (or emergency CABG) is reasonable in patients 75 years of age or older who have received fibrinolytic therapy, and are in cardiogenic shock, provided that they are suitable candidates for revascularization. (Level of Evidence: B)
2. It is reasonable to perform rescue PCI for patients with 1 or more of the following:
a. Hemodynamic or electrical instability. (Level of Evidence: C)
b. Persistent ischemic symptoms. (Level of Evidence: C)
3. A strategy of coronary angiography with intent to perform rescue PCI is reasonable for patients in whom fibrinolytic therapy has failed (ST segment elevation less than 50% resolved after 90 minutes following initiation of fibrinolytic therapy in the lead showing the worst initial elevation) and a moderate or large area of myocardium at risk (anterior MI, inferior MI with right ventricular involvement or precordial ST segment depression). (Level of Evidence: B)
Class IIb
1. A strategy of coronary angiography with intent to perform PCI in the absence of one or more of the above Class I or IIa indications might be reasonable in moderate and high-risk patients, but its benefits and risks are not well established. The benefits of rescue PCI are greater the earlier it is initiated after the onset of ischemic discomfort. (Level of Evidence: C)
Class III
1. A strategy of coronary angiography with intent to perform PCI (or emergency CABG) is not recommended in patients who have received fibrinolytic therapy if further invasive management is contraindicated or the patient or designee does not wish further invasive care. (Level of Evidence: C)
B. PCI after Successful Fibrinolysis or for Patients not undergoing Primary Reperfusion
Guidelines (Do Not Edit)
Class IIb
PCI of a hemodynamically significant stenosis in a patent infarct artery greater than 24 hours after STEMI may be considered as part of an invasive strategy. (Level of Evidence: B)
Class III
PCI of a totally occluded infarct artery greater than 24 hours after STEMI is not recommended in asymptomatic patients with one or two-vessel disease if they are hemodynamically and electrically stable and do not have evidence of severe ischemia. (Level of Evidence: B)
Sources
- The 2004 ACC/AHA Guidelines for the Management of Patients With ST-Elevation Myocardial Infarction [6]
- The 2007 Focused Update of the ACC/AHA 2004 Guidelines for the Management of Patients with ST-Elevation Myocardial Infarction [7]
References
- ↑ Sutton AG, Campbell PG, Graham R; et al. (2004). "A randomized trial of rescue angioplasty versus a conservative approach for failed fibrinolysis in ST-segment elevation myocardial infarction: the Middlesbrough Early Revascularization to Limit INfarction (MERLIN) trial". J. Am. Coll. Cardiol. 44 (2): 287–96. doi:10.1016/j.jacc.2003.12.059. PMID 15261920. Unknown parameter
|month=ignored (help) - ↑ Gershlick AH, Stephens-Lloyd A, Hughes S; et al. (2005). "Rescue angioplasty after failed thrombolytic therapy for acute myocardial infarction". N. Engl. J. Med. 353 (26): 2758–68. doi:10.1056/NEJMoa050849. PMID 16382062. Unknown parameter
|month=ignored (help) - ↑ Patel TN, Bavry AA, Kumbhani DJ, Ellis SG (2006). "A meta-analysis of randomized trials of rescue percutaneous coronary intervention after failed fibrinolysis". Am. J. Cardiol. 97 (12): 1685–90. doi:10.1016/j.amjcard.2006.01.028. PMID 16765114. Unknown parameter
|month=ignored (help) - ↑ Collet JP, Montalescot G, Le May M, Borentain M, Gershlick A (2006). "Percutaneous coronary intervention after fibrinolysis: a multiple meta-analyses approach according to the type of strategy". J. Am. Coll. Cardiol. 48 (7): 1326–35. doi:10.1016/j.jacc.2006.03.064. PMID 17010790. Unknown parameter
|month=ignored (help) - ↑ Wijeysundera HC, Vijayaraghavan R, Nallamothu BK; et al. (2007). "Rescue angioplasty or repeat fibrinolysis after failed fibrinolytic therapy for ST-segment myocardial infarction: a meta-analysis of randomized trials". J. Am. Coll. Cardiol. 49 (4): 422–30. doi:10.1016/j.jacc.2006.09.033. PMID 17258087. Unknown parameter
|month=ignored (help) - ↑ Antman EM, Anbe DT, Armstrong PW, Bates ER, Green LA, Hand M, Hochman JS, Krumholz HM, Kushner FG, Lamas GA, Mullany CJ, Ornato JP, Pearle DL, Sloan MA, Smith SC, Alpert JS, Anderson JL, Faxon DP, Fuster V, Gibbons RJ, Gregoratos G, Halperin JL, Hiratzka LF, Hunt SA, Jacobs AK (2004). "ACC/AHA guidelines for the management of patients with ST-elevation myocardial infarction: a report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines (Committee to Revise the 1999 Guidelines for the Management of Patients with Acute Myocardial Infarction)". Circulation. 110 (9): e82–292. PMID 15339869. Unknown parameter
|month=ignored (help) - ↑ Antman EM, Hand M, Armstrong PW; et al. (2008). "2007 Focused Update of the ACC/AHA 2004 Guidelines for the Management of Patients With ST-Elevation Myocardial Infarction: a report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines: developed in collaboration With the Canadian Cardiovascular Society endorsed by the American Academy of Family Physicians: 2007 Writing Group to Review New Evidence and Update the ACC/AHA 2004 Guidelines for the Management of Patients With ST-Elevation Myocardial Infarction, Writing on Behalf of the 2004 Writing Committee". Circulation. 117 (2): 296–329. doi:10.1161/CIRCULATIONAHA.107.188209. PMID 18071078. Unknown parameter
|month=ignored (help)