Renovascular disease
| Renovascular disease | |
 | |
|---|---|
| Renal artery stenosis |
|
Renovascular disease Microchapters |
|
Diagnosis |
|---|
|
Treatment |
|
Case Studies |
|
Renovascular disease On the Web |
|
American Roentgen Ray Society Images of Renovascular disease |
Editor-In-Chief: C. Michael Gibson, M.S., M.D. [1]
Etiology & Pathophysiology
Causes of Ischemic Renal Disease
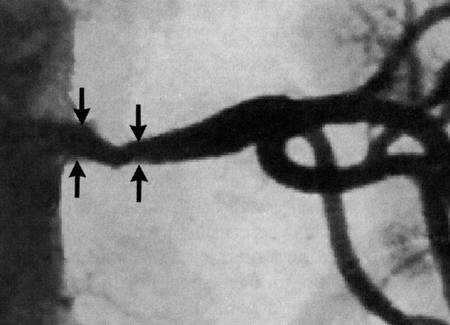
- Atherosclerotic Renal Artery Stenosis (ARAS)
- Atherosclerosis accounts for approximately 90% of the cases of RAS and is the predominant lesion detected in patients >50 years of age
- The presence and number of diseased coronary arteries predicts the likelihood of ARAS
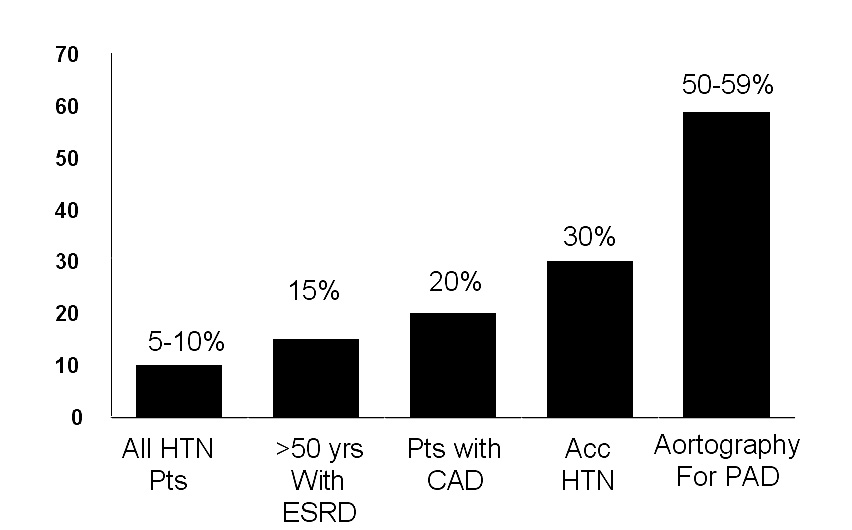
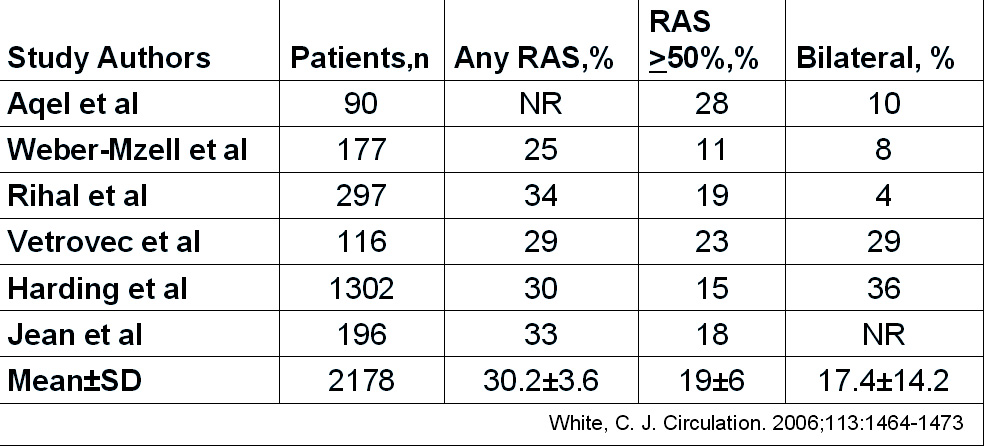
- RAS resulting from atherosclerotic disease is common in (18% to 20%) individuals undergoing coronary angiography (1)
- RAS resulting from atherosclerotic disease is even more common (35% to 50%) in individuals undergoing peripheral vascular angiography for occlusive disease of the aorta and legs (2)
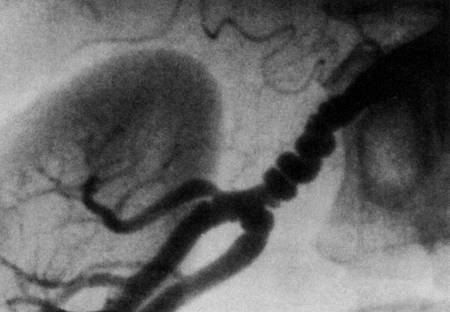
- Fibromuscular dysplasia
- Unknown etiology
- Second most common cause of RAS
- Affects middle-aged women
- More common in first-degree relatives and in the presence of the ACE-I allele.
- Renal artery involvement is seen in 60% of cases - frequently bilateral compromise.
- Progressive renal stenosis is seen in 37% of cases and loss of renal mass in 63%
- Nephroangiosclerosis (HTN injury)
- Diabetic Nephropathy (small vessels)
- Renal thromboembolic disease
- Atheroembolic renal disease
- Aortorenal dissection
- Post renal transplant RAS
- Renal artery vasculitis
- Trauma
- Neurofibromatosis
- Thromboangiitis obliterans
- Scleroderma
Incidence
- Prevalence of Renal Artery Stenosis
- Most Common Cause of HTN
- Incidence of Renal Artery Stenosis at Cardiac Catheterization
Diagnosis
- Manifestations of Renovascular Disease (3)
- Asymptomatic "Incidental RAS"
- Renovascular Hypertension
- Ischemic Nephropathy
- Accelerated CV Disease
- Congestive Heart Failure
- Stroke
- Secondary Aldosteronism
Clinical Clues to the Diagnosis of Renal Artery Stenosis-ACC/AHA Guidelines
- CLASS I
- Onset of hypertension before the age of 30 years or severe hypertension after age 55; level of evidence B
- Accelerated, resistant, or malignant hypertension; level of evidence C
- Development of new azotemia or worsening renal function after administration of an ACE inhibitor or ARB agent; level of evidence B
- Uneaplained atrophic kidney or sizse discrepancy between kidnyes of >1.5cm; level of evidence B
- Sudden, unexplained pulmonary edema; level of evidence B
- CLASS IIa
- Unexplained renal dysfunction, including individuals starting renal replacement therapy; level of evidence B
- CLASS IIb
- Multivessel coronary artery disease; level of evidence B
- Unexplained congestive heart failure; level of evidence C
- Refractory angina; level of evidence C
Diagnostic Methods to Detect Renal Artery Stenosis - ACC/AHA Guidelines
- CLASS I
- Duplex ultrasound sonography is recommended as a screening test to establish the diagnosis of renal artery stenosis; Level of eveidence: B
- Computed tomographic angiography(in individuals with normal renal function) is recommended as a screnning test to establish the diagnosis of renal artery stenosis; Level of eveidence: B
- Magnetic resonance angiography is recommended as a screening test to establish the diagnosis of renal artery stenosis; Level of eveidence: B
- When the clinical index of suspicion is high and the results of noninvasive tests are inconclusive, cathether angiography is recommended as a diagnostic test to establish teh diagnosis of renal aretry stenosis; Level of eveidence: B
- CLASS III
- Captopril renal scintigraphy is not recommended as a screening test to establish the diagnosis of renal artery stenosis; Level of eveidence: C
- Selective renal vein measurements are not recommended as a useful screening test to establish the diagnosis of RAS; Level of eveidence: B
- The plasma renin activity is not recommended as a useful screening test to establish the diagnosis of RAS; Level of eveidence: B
- The captopril test (measurements of plasma renin activity following captopril administration) is not recommended as a useful screening test to establish the diagnosis of renal artery stenosis; Level of eveidence: B
Indications for Revascularization
- Reasons to Revascularize Atherosclerotic Renovascular Disease
- Indications for revascularization of RAS
- hypertension
- Failure of medical therapy despite full doses of 3 drugs, including diuretic
- Compelling need for ACE inhibition/angiotensin blockade with angiotensin-dependent GFR
- Progressive renal insufficiency with salvagable kidneys
- Recent rise in serum creatinine
- Loss of GFR during antihypertensive therapy (e.g., ACEI)
- Evidence of preserved diastolic blood flow (low resistive index)
- Circulatory congestion, recurrent “flash” pulmonary edema
- Refractory congestive heart failure with bilateral renal artery stenosis
- hypertension
Treatment Options
Medical Therapy
PTA
Surgical
Technical Considerations
Renal Arteriography
- Abdominal Aortogram: identification of ostia of the renal arteries and accessory renal arteries (25% of population)
- Arteriography should include both the arterial phase and the nephrographic phase
- Disease involving renal bifurcations require cranial or caudal angulation to open out the lesion
- Evidence of aortic atheroma: technique of no-touch angiography is recommended
Brachial Approach
- For renal arteries that are oriented cephalad.
- When the aorta is occluded distally or the renal artery takeoff is severely angulated
- Proximal renal artery segment initially courses inferiorly and posteriorly braquial approach allows more coaxial alignment.
- Greater incidence of vascular site complications
Femoral approach
- Renal artery angioplasty and stenting are usually performed via retrograde femoral approach.
- When the real artery origin is oriented horizontally or caudally with respect to the aorta, femoral approach is preferred.
Complications
Complications of Percutaneous Renal Revascularization
- Atheroembolism into the renal or peripheral vascular bed = cholesterol embolization
- Dissection of renal artery or the wall of the aorta
- Acute or delayed thrombosis
- Infection
- Rupture of renal artery
- Renal perforation
Prognosis
Favorable Predictors
Successful Outcome For Control Of Hypertension
- Rapid acceleration of hypertension over the prior weeks or months
- Presence of “malignant” hypertension
- Hypertension in association with flash pulmonary edema
- Contemporaneous rise in serum creatinine
- Development of azotemia in response to ACE inhibitors administered for control of hypertension.
Successful Salvage Or Preservation Of Renal Function
- Recent rapid rise in creatinine, unexplained by other factors
- Azotemia resulting from ACE inhibitors
- Absence of diabetes or other cause of intrinsic kidney disease
- Presence of global renal ischemia, wherein the entire functioning renal mass is subtended by bilateral critically narrowed renal arteries or a vessel supplying a solitary kidney.
Unfavorable Predictors
- Renal atrophy demonstrated by kidney length <7.5 cm on ultrasound
- High renal resistance index detected by duplex ultrasound
- Proteinuria > 1gm/day
- Hyperuricemia
- Creatinine clearance <40 mL/minute
References
- PMID 11936924
- PMID 12472042
- PMID 16129817