Platelet rich plasma
Editor-in-Chief: Robert G. Schwartz, M.D. [1], Piedmont Physical Medicine and Rehabilitation, P.A.; Mayo Friedlis, M.D. [2], Physical Medicine and Pain Management Speicialist, Capitol Spine and Pain Centers, Fairfax, VA
Please Join in Editing This Page and Apply to be an Editor-In-Chief for this topic: There can be one or more than one Editor-In-Chief. You may also apply to be an Associate Editor-In-Chief of one of the subtopics below. Please mail us [3] to indicate your interest in serving either as an Editor-In-Chief of the entire topic or as an Associate Editor-In-Chief for a subtopic. Please be sure to attach your CV and or biographical sketch.
Overview
PRP is an autologous blood therapy that stimulates your body’s natural healing process through the injection of its own growth factors into injured areas. Research and clinical data show that PRP injections are extremely safe, with minimal risk for any adverse reaction or complication. Because PRP is produced from your own blood, there is no concern for rejection or disease transmission. There is a small risk of infection from any injection into the body, but this is rare. Some research suggests that PRP may have an anti-bacterial property which protects against possible infection.
Your body naturally recruits platelets and white blood cells from the blood to initiate a healing response. Under normal conditions, platelets store numerous growth factors which are released in response to signals from the injured tissue. Special PRP devices concentrate platelets from whole blood. When the PRP is injected into the damaged tissue growth factor release is enhanced so that natural healing is accelerated. Desired results include by enhancing the body's natural healing capacity, and a more rapid, more efficient, more thorough restoration of tissue to a healthy state [4].
History
PRP was initially developed in the 1970s. It enjoyed increasing use in hospital and outpatient surgical settings in the 1980's and began to be utilized in physician offices for musculoskeletal procedures in the 1990's. Technological advances have enabled the administration of PRP to become more popular among musculoskeletal physicians (physiatrists and orthopedists) since 2000. Much of the original PRP use centered around orhtopedic surgical procedures, such as spinal fusions and joint replacements,however PRP has also enjoyed extensive use among maxillofacial and plastic surgeons and dermatologists.
Pathophysiology
After an injury, the repair response of musculoskeletal tissues starts with the formation of a blood clot and degranulation of platelets, which releases growth factors and cytokines at the site. This microenvironment results activation of inflammatory cells and proliferation of local progenitor cells. In most cases, fibroblastic scar tissue is formed. In some settings, however, such as in a fracture callus, these conditions can also facilitate the formation of new bone tissue.
Transforming growth factor beta (TGF-b), platelet-derived growth factor (PDGF), insulin-like growth factor (IGF), vascular endothelial growth factors (VEGF), epidermal growth factor (EGF) and fibroblast growth factor-2 (FGF-2) are growth factors that can be found at injury sites during wound healing. In addition to soft tissue repair (muscle, tendon, ligament and supporting joint structures), PRP has been shown to enhance one or more phases of osteogenesis, early angiogenesis and revascularization.
Studies also recognize the possibility that the effect of the clot microenvironment or concentrates of PDFGs on fracture repair might be either positive or negative. The nature of this effect, like that of many graft materials, depends on the clinical setting, particularly the graft site’s local environment of cells in which PRP or associated factors are placed.
In summary, available data suggest that PRP is valuable in enhancing soft-tissue repair and in wound healing. The clinical role of PRP in bone repair remains controversial however. PRP is not uniformly successful as an adjuvant to bone grafting procedures. PRP may promote or inhibit bone formation, depending on the setting in which it is used and the quality of the PRP.
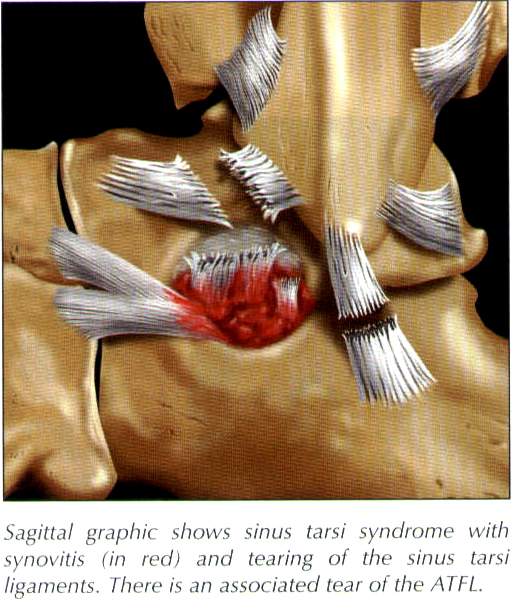
Example musculoskeletal conditions and symptoms treated with PRP
- Sports injuries
- Joint pain associated with arthritis
- Ligamentous strain
- Tendionosis, Tendinopathy
- Reflex muscle spasm
- Recurrent swelling or fullness involving a joint or muscular region
- Popping, clicking, grinding, or catching sensations with movement
- Spinal pain (musculoskeletal; non neurogenic in origin)
- Distinct tender points and “jump signs” along the bone at tendon or ligament attachments
- Sclerotomal numbness, tingling, aching, or burning, referred into an upper or lower extremity
- Recurrent, referred headache, face pain, jaw pain, ear pain
Treatment

In most instances PRP is not the first treatment employed. Other traditional interventions such as restorative therapies, medication, anesthetic injection and [Prolotherapy] are frequently employed first. Most musculoskeletal physicians will use Prolotherapy prior to PRP when considering regenerative treatment for muscle, tendon, ligament or supporting joint structures, however individual considerations exist. Examples where PRP might be utilized first include professional athletes that need rapid wound healing time, more severe cases and instances where multiple problems exist.
PRP is an effective alternative to invasive arthroscopic surgery, including those cases that have failed or that simply are not remedial to arthroscopy. When contraindications exist for joint replacement (obesity, age, medical co morbidity) PRP can also be a beneficial alternative however in these cases PRP is more commonly used as an activator in conjunction with autologous stem cell grafting.
The PRP process involves drawing blood, spinning it down to separate out growth factor rich platelets, then injecting the platelet rich plasma into the injured area. To make the injection more comfortable, local anesthetic (numbing medicine) or nerve blocks are performed first. To help ensure accuracy of placement, Ultrasound guidance is employed (see [Diagnostic musculoskeletal ultrasound]).
Most patients don’t require anything more then acetaminophen for pain from the procedure. Often, following a PRP injection, an "achy" soreness is felt. This "soreness" is a positive sign that healing has been set in motion. The soreness can last for several days but gradually decreases as healing and tissue repair occurs. It is important that anti-inflammatory medications such as Ibuprofen, Aleve and Aspirin be avoided following PRP treatments.
These medicines may block the effects of the PRP injection. While many patients find it best to rest the area for several days after PRP, as long as you are responsible you can resume normal activities following I treatment. You should avoid anything other then light activity however for at least several days after injection.
Depending on your response to treatment, one to three PRP injections may be required. Following the initial treatment a follow up visit will usually be scheduled within 2-3 weeks. At that time a decision may be made regarding the need for additional treatment. In general, chronic or severe injuries require more treatment then mild injuries. Restorative therapy including exercise or physical therapy may be prescribed as well.