Pediculosis pubis
|
WikiDoc Resources for Pediculosis pubis |
|
Articles |
|---|
|
Most recent articles on Pediculosis pubis Most cited articles on Pediculosis pubis |
|
Media |
|
Powerpoint slides on Pediculosis pubis |
|
Evidence Based Medicine |
|
Cochrane Collaboration on Pediculosis pubis |
|
Clinical Trials |
|
Ongoing Trials on Pediculosis pubis at Clinical Trials.gov Trial results on Pediculosis pubis Clinical Trials on Pediculosis pubis at Google
|
|
Guidelines / Policies / Govt |
|
US National Guidelines Clearinghouse on Pediculosis pubis NICE Guidance on Pediculosis pubis
|
|
Books |
|
News |
|
Commentary |
|
Definitions |
|
Patient Resources / Community |
|
Patient resources on Pediculosis pubis Discussion groups on Pediculosis pubis Patient Handouts on Pediculosis pubis Directions to Hospitals Treating Pediculosis pubis Risk calculators and risk factors for Pediculosis pubis
|
|
Healthcare Provider Resources |
|
Causes & Risk Factors for Pediculosis pubis |
|
Continuing Medical Education (CME) |
|
International |
|
|
|
Business |
|
Experimental / Informatics |
For patient information click here
Editor-In-Chief: C. Michael Gibson, M.S., M.D. [1]; Associate Editor(s)-in-Chief: Kiran Singh, M.D. [2]; Dima Nimri, M.D. [3]
Synonyms and keywords: Pubic louse infestation; Phthiriasis pubis; Pubic lice; Crabs; Infestation caused by crab lice; Infestation caused by Phthirus pubis; Infestation by crab lice
Overview
Pediculosis pubis (also known as "crabs" and "pubic lice"[1]) is a disease caused by the pubic louse, Pthirus pubis, a parasitic insect notorious for infesting human pubic hair. The species may also live on other areas with hair, including the eyelashes, causing pediculosis ciliaris. Infestation usually leads to intense itching in the pubic area. Treatment with topic agents such as permethrin or pyrethrin with piperonyl butoxide is exceedingly effective. Worldwide it affects about 2% of the population.
Historical Perspective
- Pediculosis pubis was reported in the literature as early as 1946.[2]
- In 1946, Andrew G. Franks describes the use of DDT in the treatment of pediculosis pubis.[2]
Classification
Infestation with pubic lice may be classified according to the site affected into:[3]
- Phthiriasis pubis: infestation of pubic hair with pubic lice
- Phthiriasis palpebrarum: infestation of eyelashes with pubic lice
Pathophysiology
Transmission
Pubic lice are usually acquired by intimate contact between individuals.[4] Parent-to-child infestations are more likely to occur through routes of shared towels, clothing, beds or closets. Adults are more frequently infested than children. As with most sexually transmitted pathogens, they can only survive a short time away from the warmth and humidity of the human body. Infection in a young child is not necessarily indicative of sexual abuse, although this possibility should be kept in mind.[5][6]
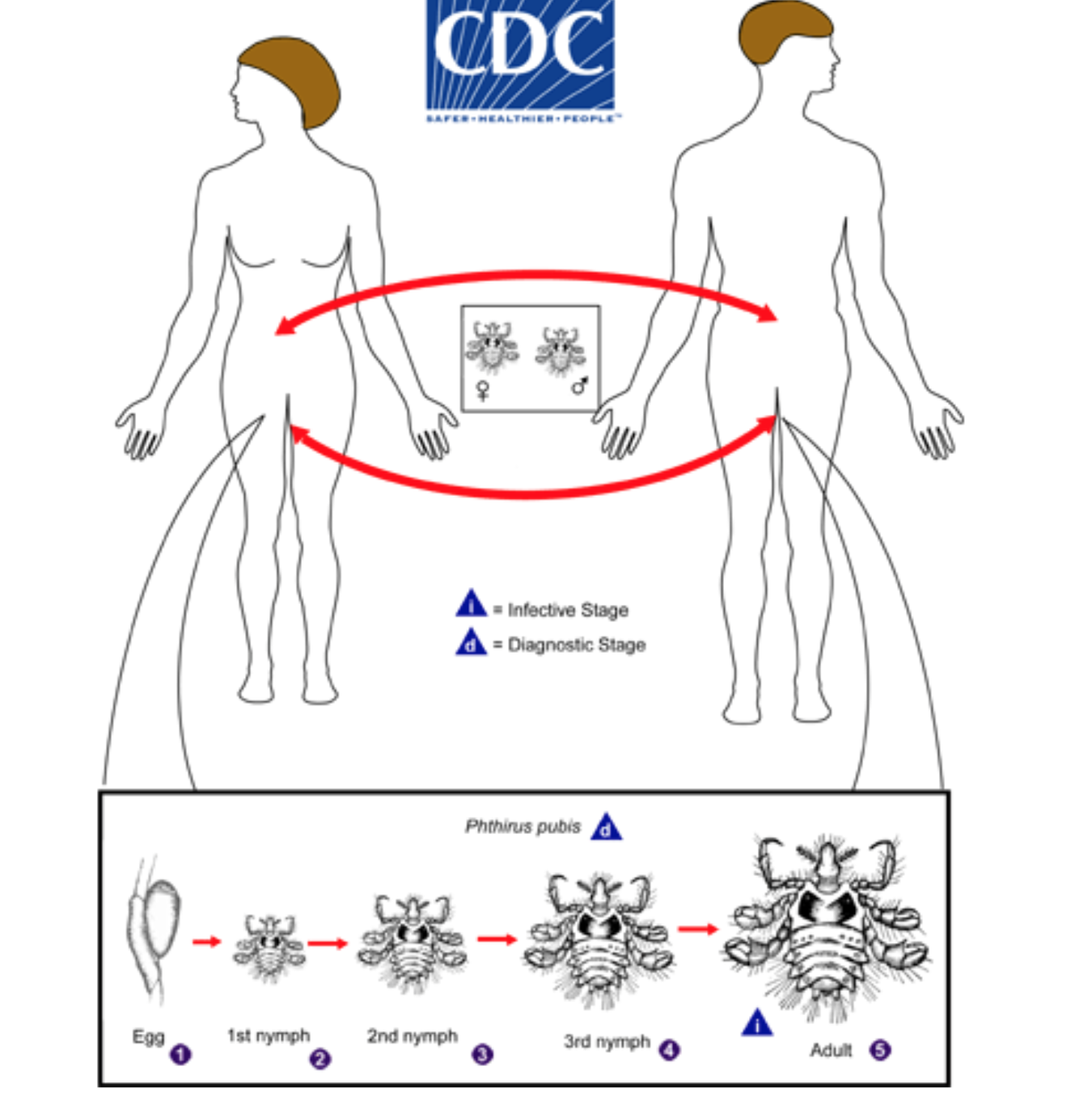
Life Cycle
Pubic lice (Phthirus pubis) have three stages: egg, nymph and adult. Eggs (nits) are laid on a hair shaft. Females will lay approximately 30 eggs during their 3–4 week life span. Eggs hatch after about a week and become nymphs, which look like smaller versions of the adults. The nymphs undergo three molts before becoming adults. Adults are 1.5–2.0 mm long and flattened. They are much broader in comparison to head and body lice. Adult lice are found only on the human host and require human blood to survive. If adults are forced off the host, they will die within 24–48 hours without a blood feeding. Pubic lice are transmitted from person to person most-commonly via sexual contact, although fomites (bedding, clothing) may play a minor role in their transmission.
Macroscopic Characteristics
Pubic lice have three forms: the egg (also called a nit), the nymph, and the adult.
- Nit: Nits are lice eggs. They can be hard to see and are found firmly attached to the hair shaft. They are oval and usually yellow to white.
- Nymph: The nymph is an immature louse that hatches from the nit (egg). A nymph looks like an adult pubic louse but it is smaller. To live, a nymph must feed on blood. It takes 2–3 weeks after hatching to mature into adults capable of reproducing.
- Adult: The adult pubic louse resembles a miniature crab when viewed through a strong magnifying glass. Pubic lice have six legs; their two front legs are very large and look like the pincher claws of a crab. This is how they got the nickname "crabs." Pubic lice are tan to grayish-white in color. Females lay nits and are usually larger than males. To live, lice must feed on blood. If the louse falls off a person, it dies within 1–2 days.[4]
Causes
The cause of pubic lice is pediculus pubis. For more information about the microorganism, click here.
Differentiating Pediculosis pubis from other Diseases
Pediculosis pubis must be differentiated from other diseases that cause pruritus and excoriation in the pubic area:[7][8][9]
| Disease | Findings |
|---|---|
| Scabies |
|
| Trichomycosis |
|
| White piedra (a fungal infection) |
|
Epidemiology and Demographics
- The incidence of pubic lice worldwide is estimated at 2,000 per 100,000 cases.[10][11]
- Accurate numbers are difficult to acquire, because pubic lice infestations are not considered a reportable condition by many governments, and many cases are self-treated or treated discreetly by personal physicians.[12]
- It has recently been suggested that an increasing percentage of humans removing their pubic hair has led to reduced crab louse populations in some parts of the world.[13][14]
Risk Factors
Sexual contact with a person infected with pubic lice is a risk factor for its transmission.
Natural History, Complications and Prognosis
Natural History
If left untreated, infestation with pubic lice may persist and lead to secondary bacterial infection due to the associated intense itching.
Complications
Most common complication of pubic lice infestation is excoriations due to intense itching, which may lead to a secondary bacterial infection. When pediculus pubis infests the eyelashes, it may lead to eye infections, such as blepharitis and conjunctivitis.
Prognosis
With proper medical treatment with antimicrobial drugs, pediculosis pubis has an excellent prognosis.
Screening
There are no screening recommendations for pubic lice. [15]
History and Symptoms
- Although any part of the body may be colonized, crab lice favor the hairs of the genital and peri-anal region. Especially in male patients, pubic lice and eggs can also be found in hair on the abdomen and under the armpits as well as on the beard and mustache, while in children they are usually found in eyelashes. Infestation with pubic lice is called Phthiriasis or Pediculosis pubis, while infestation of eyelashes with pubic lice is called Phthriasis palpebrarum [16].
- The main symptom is itching, usually in the pubic hair area. It results from hypersensitivity to louse saliva, and it becomes strong enough 2 or more weeks following initial infestation.[10]
- Erythematous sore lesions may be seen due to scratching.[10]
- In the majority of infestations, a characteristic grey-blue or slate coloration appears (maculae caeruleae) at the feeding site, which may last for days and is also characteristic for the infestation.
Physical Examination
Skin examination in patients with pubic lice may reveal the following findings:[17]
- Visualization of the pubic lice and their nits in the pubic area. Other sites that may be affected include the perianal and inguinal areas, axillary and chest hair, as well as the eyelashes.
- Papular urticaria
- Excoriations, which may become secondarily infected
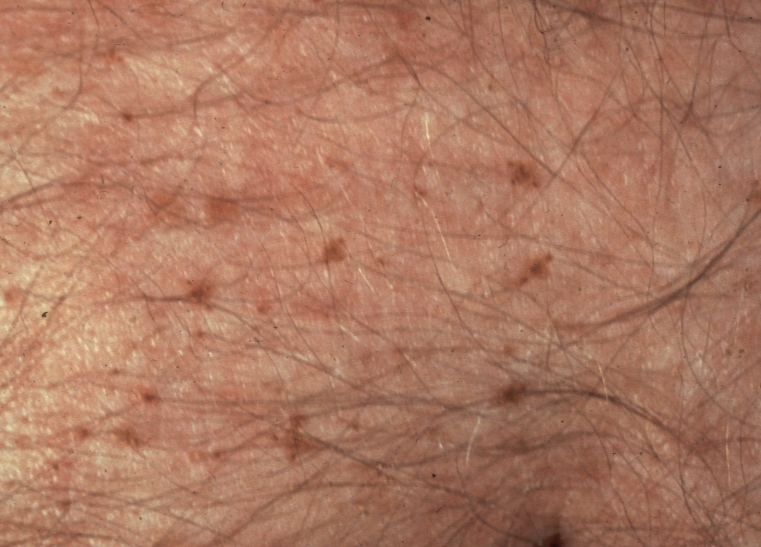
- Maculae cerulea: a pathognomonic finding for pubic lice. These are blue-gray, irregularly shaped macules, which measure 0.5-1 cm in diameter and are usually scattered over the lower abdomen, buttocks and upper thighs.
- Inguinal lymphadenopathy
-
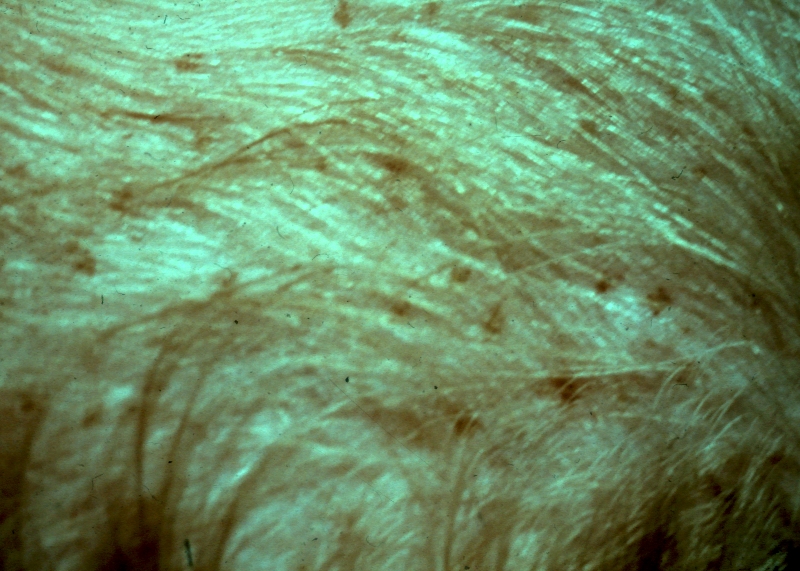
Fig.1 Pubic lice in genital area
-
Fig.2 Pubic lice in abdomen
-
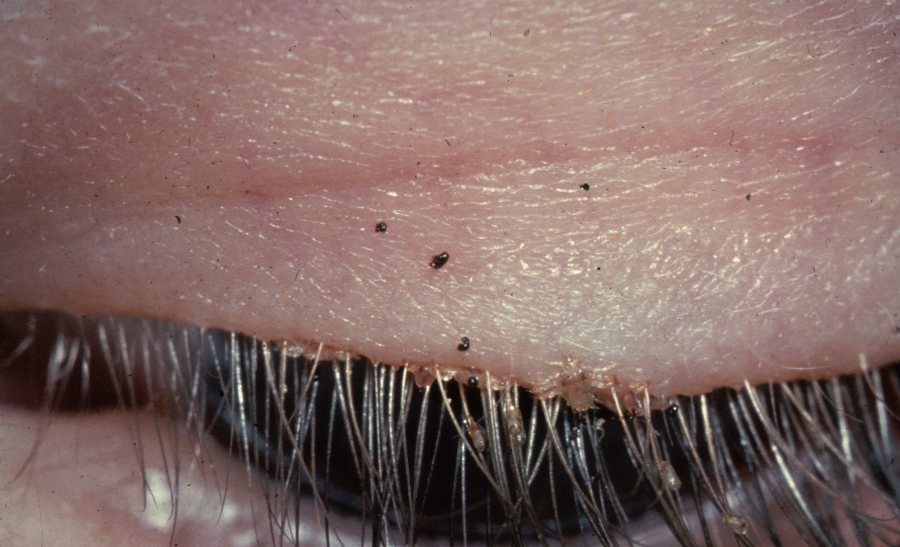
Fig.3 Pubic lice on eye-lashes
Laboratory Findings
The diagnosis of pubic lice is made by visualization of lice on pubic hair and there are no laboratory findings associated with pubic lice.[18]
Other Diagnostic Studies
Diagnosis of pediculosis pubis is made through direct visualization of the lice on pubic hair.[18]
Medical Therapy
- Generally, all patients with Pediculosis pubis require antimicrobial therapy.
- Randomized clinical data that compares the efficacy and safety of antimicrobial therapies is scarce.
- The majority of trials that evaluate therapies for Pediculosis pubis are based on the management of head lice.[19][20][21][22]
- Preferred regimen (1): Permethrin 1% cream rinse applied to affected areas and washed off after 10 minutes
- Alternative regimen (1): Malathion 0.5% lotion applied to affected areas and washed off after 8–12 hours
- Alternative regimen (2): Phenothrin 0.2% lotion applied to affected areas and washed off after 2 hours
- Alternative regimen (3): Ivermectin 250 ug/kg PO, may be repeated in 1-2 weeks
- Note (1): If Malathion or Phenothrin lotion is to be applied to hair, the hair should be dry. In contrast, Permethrin should be applied to wet hair.
- Note (2): If necessary, treatment may be repeated after 1 week.
- Note (3): Permethrin may be safe among pregnant women, but randomized data is lacking.[25]
Specific Considerations
Eyelashes
If the eyelashes are infected, the following are indicated:[24]
- Preferred regimen: Permethrin 1% lotion to be applied using a cotton swab to the eyelashes and to be washed out after 10 minutes
- Alternative regimen: Ivermectin 250 ug/kg PO, may be repeated in 1-2 weeks
- Note: Keep eyelids closed during application of Permethrin
- Vaseline eye patch may be reapplied twice per day for 8-10 days
- Use tweezers (or forceps) to remove visible lice
Non-Pharmacologic Management
Treatment of Sexual Partners
- Pubic lice may be spread through sexual intercourse.
- Therefore, all partners with whom the patient has had sexual contact within the previous 30 days should be evaluated and treated, and sexual contact should be avoided until all partners have successfully completed treatment and are thought to be cured.[24]
- Because of the strong association between the presence of pubic lice and other sexually transmitted infections (STIs), patients diagnosed with pubic lice should undergo evaluation for other STIs.[24]
Surgery
There is no role for surgery in the treatment of pubic lice.
Primary Prevention
Abstaining from sexual intercourse with an infected person is one of the means of preventing infestation with pubic lice.
Secondary Prevention
Once a patient is diagnosed with pubic lice, the following preventive measures may be followed:[17]
- Washing with hot water and drying of all clothes and bedding
- Promoting personal hygiene and sanitation measures
- Treatment of sexual contacts with pubic lice
- Examining patients and their sexual partners for other STDs.
References
- ↑ Ronald P. Rapini, Jean L. Bolognia & Joseph L. Jorizzo (2007). Dermatology. St. Louis: Mosby. ISBN 1-4160-2999-0.
- ↑ 2.0 2.1 FRANKS AG, DOBES WL (1946). "DDT in the treatment of scabies, larva migrans and pediculosis pubis". Arch Derm Syphilol. 53: 381. PMID 21026349.
- ↑ N. P. Manjunatha, G. R. Jayamanne, S. P. Desai, T. R. Moss, J. Lalik & A. Woodland (2006). "Pediculosis pubis: presentation to ophthalmologist as pthriasis palpebrarum associated with corneal epithelial keratitis". International Journal of STD & AIDS. 17 (6): 424–426. doi:10.1258/095646206777323445.
- ↑ 4.0 4.1 P. A. Leone (2007). "Scabies and pediculosis pubis: an update of treatment regimens and general review". Clinical Infectious Diseases. 44 (Suppl. 3): S153–S159. doi:10.1086/511428. PMID 17342668.
- ↑ Sidney Klaus, Yigal Shvil & Kosta Y. Mumcuoglu (1994). "Generalized infestation of a 3½-year-old girl with the pubic louse". Pediatric Dermatology. 11 (1): 26–28. doi:10.1111/j.1525-1470.1994.tb00068.x. PMID 8170844.
- ↑ José A. Varela, Luis Otero, Emma Espinosa, Carmen Sánchez, María Luisa Junquera & Fernando Vázquez (April 2003). "Phthirus pubis in a sexually transmitted diseases unit: a study of 14 years". Sexually Transmitted Diseases. 30 (4): 292–6. doi:10.1097/00007435-200304000-00004. PMID 12671547.
- ↑ Sentamilselvi G, Janaki C, Murugusundram S (2009). "Trichomycoses". Int J Trichology. 1 (2): 100–7. doi:10.4103/0974-7753.58552. PMC 2938571. PMID 20927231.
- ↑ Anderson AL, Chaney E (2009). "Pubic lice (Pthirus pubis): history, biology and treatment vs. knowledge and beliefs of US college students". Int J Environ Res Public Health. 6 (2): 592–600. doi:10.3390/ijerph6020592. PMC 2672365. PMID 19440402.
- ↑ Leone PA (2007). "Scabies and pediculosis pubis: an update of treatment regimens and general review". Clin Infect Dis. 44 Suppl 3: S153–9. doi:10.1086/511428. PMID 17342668.
- ↑ 10.0 10.1 10.2 Dholakia S, Buckler J, Jeans JP, Pillai A, Eagles N, Dholakia S (2014). "Pubic lice: an endangered species?". Sex Transm Dis. 41 (6): 388–91. doi:10.1097/OLQ.0000000000000142. PMID 24825336.
- ↑ Varela JA, Otero L, Espinosa E, Sánchez C, Junquera ML, Vázquez F (2003). "Phthirus pubis in a sexually transmitted diseases unit: a study of 14 years". Sex Transm Dis. 30 (4): 292–6. PMID 12671547.
- ↑ Alice L. Anderson & Elizabeth Chaney (2009). "Pubic lice (Pthirus pubis): history, biology and treatment vs. knowledge and beliefs of US College students". International Journal of Environmental Research and Public Health. 6 (2): 592–600. doi:10.3390/ijerph6020592. PMC 2672365. PMID 19440402.
- ↑ N. R. Armstrong & J. D. Wilson (2006). "Did the "Brazilian" kill the pubic louse?". Sexually Transmitted Infections. 82: 265–266. doi:10.1136/sti.2005.018671. PMC 2564756. PMID 16731684.
- ↑ Bloomberg: Brazilian bikini waxes make crab lice endangered species, published 13 January 2013, retrieved 14 January 2013
- ↑ U.S. Preventive Services Task Force https://www.uspreventiveservicestaskforce.org/BrowseRec/Search?s=pubic+lice
- ↑ Manjunatha NP, Jayamanne GR, Desai SP, Moss TR, Lalik J, Woodland A. Pediculosis pubis: presentation to ophthalmologist as pthriasis palpebrarum associated with corneal epithelial keratitis. Int. J. STD AIDS 2006; 17: 424-426
- ↑ 17.0 17.1 Bennett, John E.; Dolin, Raphael; Blaser, Martin J. (2015). Mandell, Douglas, and Bennett's Principles and Practice of Infectious Diseases. Elsevier Inc. ISBN 978-1-4557-4801-3.
- ↑ 18.0 18.1 Gunning K, Pippitt K, Kiraly B, Sayler M (2012). "Pediculosis and scabies: treatment update". Am Fam Physician. 86 (6): 535–41. PMID 23062045.
- ↑ Meinking TL, Taplin D, Kalter DC, Eberle MW (1986). "Comparative efficacy of treatments for pediculosis capitis infestations". Arch Dermatol. 122 (3): 267–71. PMID 2420284.
- ↑ Chosidow O, Chastang C, Brue C, Bouvet E, Izri M, Monteny N; et al. (1994). "Controlled study of malathion and d-phenothrin lotions for Pediculus humanus var capitis-infested schoolchildren". Lancet. 344 (8939–8940): 1724–7. PMID 7997000.
- ↑ Parker J (1997). "Treatment of head lice". N Engl J Med. 336 (10): 734–5, author reply 735. PMID 9045056.
- ↑ Chosidow O, Giraudeau B, Cottrell J, Izri A, Hofmann R, Mann SG; et al. (2010). "Oral ivermectin versus malathion lotion for difficult-to-treat head lice". N Engl J Med. 362 (10): 896–905. doi:10.1056/NEJMoa0905471. PMID 20220184.
- ↑ Workowski, Kimberly A.; Bolan, Gail A. (2015-06-05). "Sexually transmitted diseases treatment guidelines, 2015". MMWR. Recommendations and reports: Morbidity and mortality weekly report. Recommendations and reports / Centers for Disease Control. 64 (RR-03): 1–137. ISSN 1545-8601. PMID 26042815.
- ↑ 24.0 24.1 24.2 24.3 24.4 Scott GR, Chosidow O, IUSTI/WHO (2011). "European guideline for the management of pediculosis pubis, 2010". Int J STD AIDS. 22 (6): 304–5. doi:10.1258/ijsa.2011.011114. PMID 21680662.
- ↑ Mytton OT, McGready R, Lee SJ, Roberts CH, Ashley EA, Carrara VI; et al. (2007). "Safety of benzyl benzoate lotion and permethrin in pregnancy: a retrospective matched cohort study". BJOG. 114 (5): 582–7. doi:10.1111/j.1471-0528.2007.01290.x. PMID 17439567.
- ↑ Kalter DC, Sperber J, Rosen T, Matarasso S (1987). "Treatment of pediculosis pubis. Clinical comparison of efficacy and tolerance of 1% lindane shampoo vs 1% permethrin creme rinse". Arch Dermatol. 123 (10): 1315–9. PMID 2444166.