|
|
| (31 intermediate revisions by 6 users not shown) |
| Line 1: |
Line 1: |
| | __NOTOC__ |
| {{Infobox Disease | | | {{Infobox Disease | |
| Name = {{PAGENAME}} | | | Name = {{PAGENAME}} | |
| Line 9: |
Line 10: |
| OMIM = | | | OMIM = | |
| MedlinePlus = 000272 | | | MedlinePlus = 000272 | |
| eMedicineSubj = med | | | eMedicineSubj = | |
| eMedicineTopic = 2674 | | | eMedicineTopic = | |
| eMedicine_mult = {{eMedicine2|radio|576}} | | | eMedicine_mult = | |
| MeshID = D010192 | | | MeshID = D010192 | |
| }} | | }} |
| '''For patient information click [[{{PAGENAME}} (patient information)|here]]''' | | '''For patient information click [[{{PAGENAME}} (patient information)|here]]''' |
|
| |
|
| {{SI}} | | {{Pancreatic pseudocyst}} |
| {{CMG}} | | {{CMG}} {{AE}} [[User:Vidhipatel|Vidhi Patel]] M.B.B.S. |
|
| |
|
| '''Contributors:''' [[User:zorkun|Cafer Zorkun]] M.D., PhD.
| | {{SK}} Pseudocyst of pancreas |
|
| |
|
| {{Editor Help}}
| | ==[[Pancreatic pseudocyst overview|Overview]]== |
|
| |
|
| ==Overview== | | ==[[Pancreatic pseudocyst historical perspective|Historical Perspective]]== |
|
| |
|
| A '''pancreatic [[pseudocyst]]''' is a circumscribed collection of fluid rich in [[amylase]] and other pancreatic [[enzyme|enzymes]], blood and necrotic tissue typically located in the [[lesser sac]]. It has a non-epithelialised lining made of granulation tissue and hence the name pseudocyst ''(pseudo - false)''. By contrast, true cysts have an [[epithelium|epithelial]] lining. This is typically a complication of acute [[pancreatitis]], but may also occur following [[abdominal trauma]].
| | ==[[Pancreatic pseudocyst classification|Classification]]== |
|
| |
|
| Pancreatic pseudocysts account for approximately 75% of all pancreatic masses. | | ==[[Pancreatic pseudocyst pathophysiology|Pathophysiology]]== |
|
| |
|
| ==Etiopathogenesis== | | ==[[Pancreatic pseudocyst causes|Causes]]== |
|
| |
|
| Acute pancreatitis results amongst other things in the disruption of pancreatic parenchyma and the ductal system. This results in extravasation of pancreatic enzymes which in turn digest the adjoining tissues. This results in a collection of fluid containing pancreatic enzymes, hemolysed blood and necrotic debris around the pancreas. The [[lesser sac]] being a potential space, the fluid collects here preferentially. This is called an acute pancreatic collection. Some of these collections resolve on their own as the patient recovers from the acute episode. However, others become more organised and get walled-off within a thick wall of granulation tissue and fibrosis. This takes several weeks to occur and results in a pancreatic pseudocyst.
| | ==[[Pancreatic pseudocyst differential diagnosis|Differentiating Pancreatic pseudocyst from other Diseases]]== |
|
| |
|
| ==Diagnosis== | | ==[[Pancreatic pseudocyst epidemiology and demographics|Epidemiology and Demographics]]== |
|
| |
|
| The questions that need to be answered are:
| | ==[[Pancreatic pseudocyst risk factors|Risk Factors]]== |
| * where, how big and how many?
| |
| * is there a communication with the pancreatic ductal system? Draining such a pseudocyst carries an increased risk of pancreatic fistula.
| |
|
| |
|
| The most useful imaging tools are;
| | ==[[Pancreatic pseudocyst screening|Screening]]== |
|
| |
|
| * [[Ultrasonography]] - The role of ultrasonography in imaging the pancreas is limited by patient habitus, operator experience and the fact that the pancreas lies behind the stomach (and so a gas-filled stomach will obscure the pancreas).
| | ==[[Pancreatic pseudocyst natural history, complications and prognosis|Natural History, Complications and Prognosis]]== |
| * [[Computerized tomography]] - This is the gold standard for initial assessment and follow-up
| |
|
| |
|
| [http://www.radswiki.net Images courtesy of RadsWiki]
| | ==Diagnosis== |
| | | [[Pancreatic pseudocyst history and symptoms| History and Symptoms]] | [[Pancreatic pseudocyst physical examination | Physical Examination]] | [[Pancreatic pseudocyst laboratory findings|Laboratory Findings]] | [[Pancreatic pseudocyst electrocardiogram|Electrocardiogram]] | [[Pancreatic pseudocyst x ray|X Ray]] | [[Pancreatic pseudocyst CT|CT]] | [[Pancreatic pseudocyst MRI|MRI]] | [[Pancreatic pseudocyst ultrasound|Ultrasound]] | [[Pancreatic pseudocyst other imaging findings|Other Imaging Findings]] | [[Pancreatic pseudocyst other diagnostic studies|Other Diagnostic Studies]] |
| <gallery perRow="3">
| |
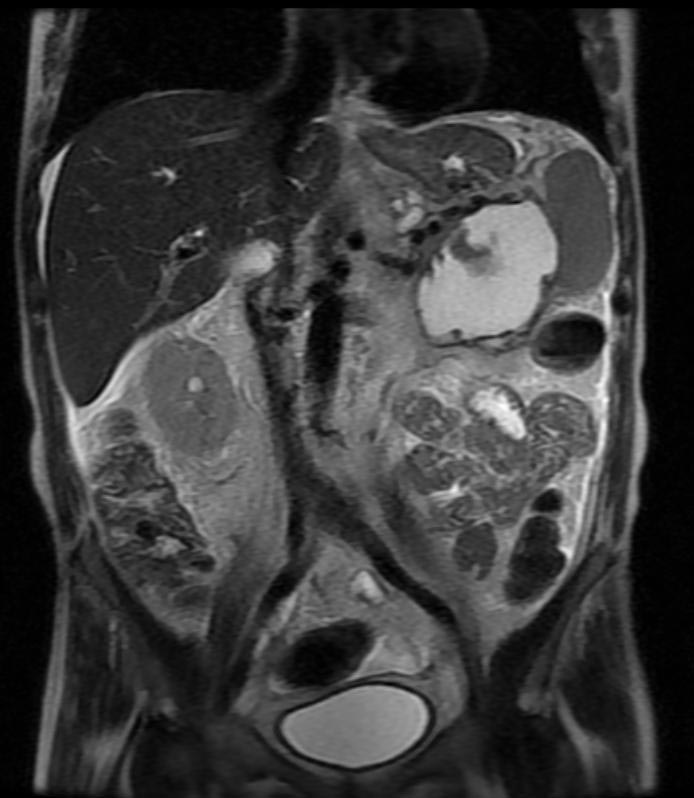
| Image:Pancreatic-pseudocyst-001.jpg|Pancreatic pseudocyst
| |
| Image:Pancreatic-pseudocyst-002.jpg|Pancreatic pseudocyst
| |
| Image:Pancreatic-pseudocyst-003.jpg|Pancreatic pseudocyst
| |
| Image:Pancreatic-pseudocyst-004.jpg|Pancreatic pseudocyst
| |
| Image:Pancreatic-pseudocyst-005.jpg|Pancreatic pseudocyst
| |
| Image:Pancreatic-pseudocyst-006.jpg|Pancreatic pseudocyst
| |
| </gallery>
| |
| | |
| * [[MRCP|Magnetic Resonance Cholangio-pancreatography]] - to establish the relationship of the pseudocyst to the pancreatic ducts
| |
|
| |
|
| ==Treatment== | | ==Treatment== |
| | [[Pancreatic pseudocyst medical therapy|Medical Therapy]] | [[Pancreatic pseudocyst surgery|Surgery]] | [[Pancreatic pseudocyst primary prevention|Primary Prevention]] | [[Pancreatic pseudocyst secondary prevention|Secondary Prevention]] | [[Pancreatic pseudocyst cost-effectiveness of therapy|Cost-Effectiveness of Therapy]] | [[Pancreatic pseudocyst future or investigational therapies|Future or Investigational Therapies]] |
|
| |
|
| A small pseudocyst that is not causing any symptoms may be managed conservatively. However, a large proportion of them will need some form of treatment, The interventions available are:
| | ==Case Studies== |
| * [[Gastroscopy|Endoscopic]] trans-gastric drainage
| |
| * Imaging guided percutaneous drainage
| |
| * Laparoscopic / open cystogastrostomy
| |
|
| |
|
| ==References & Additional Resources==
| | [[Pancreatic pseudocyst case study one|Case #1]] |
| {{refbegin|2}}
| |
| * Adams DB, Anderson MC. Percutaneous catheter drainage compared with internal drainage in the management of pancreatic pseudocyst. Ann Surg. Jun 1992;215(6):571-6; discussion 576-8.
| |
| * Ahlawat SK, Charabaty-Pishvaian A, Jackson PG, Haddad NG. Single-step EUS-guided pancreatic pseudocyst drainage using a large channel linear array echoendoscope and cystotome: results in 11 patients. JOP. 2006;7(6):616-24.
| |
| * Aranha GV, Prinz RA, Esguerra AC, Greenlee HB. The nature and course of cystic pancreatic lesions diagnosed by ultrasound. Arch Surg. Apr 1983;118(4):486-8.
| |
| * Barragan B, Love L, Wachtel M, Griswold JA, Frezza EE. A comparison of anterior and posterior approaches for the surgical treatment of pancreatic pseudocyst using laparoscopic cystogastrostomy. J Laparoendosc Adv Surg Tech A. Dec 2005;15(6):596-600.
| |
| * Beebe DS, Bubrick MP, Onstad GR, Hitchcock CR. Management of pancreatic pseudocysts. Surg Gynecol Obstet. Dec 1984;159(6):562-4.
| |
| * Bradley EL 3rd. A clinically based classification system for acute pancreatitis. Summary of the International Symposium on Acute Pancreatitis, Atlanta, Ga, September 11 through 13, 1992. Arch Surg. May 1993;128(5):586-90.
| |
| * Bradley EL, Clements JL Jr, Gonzalez AC. The natural history of pancreatic pseudocysts: a unified concept of management. Am J Surg. Jan 1979;137(1):135-41.
| |
| * Bradley EL, Gonzalez AC, Clements JL Jr. Acute pancreatic pseudocysts: incidence and implications. Ann Surg. Dec 1976;184(6):734-7.
| |
| * Brugge WR. The role of endoscopic ultrasound in pancreatic disorders. Int J Pancreatol. Aug 1996;20(1):1-10.
| |
| * Chalmers AG. The role of imaging in acute pancreatitis. Eur J Gastroenterol Hepatol. Feb 1997;9(2):106-16.
| |
| * Clemente CD. The abdomen. In: Anatomy: A Regional Atlas of the Human Body. 2nd ed. Baltimore: Urban & Schwa;1981:246-54.
| |
| * Cohen MJ, Prinz RA. Pancreatic pseudocyst. In: Cameron JL, ed. Current Surgical Therapy. 7th ed. St Louis: Mosby-Year Book;2001:543-7.
| |
| * Cooperman AM. An overview of pancreatic pseudocysts: the emperor''s new clothes revisited. Surg Clin North Am. Apr 2001;81(2):391-7, xii.
| |
| * Criado E, De Stefano AA, Weiner TM, Jacques PF. Long term results of percutaneous catheter drainage of pancreatic pseudocysts. Surg Gynecol Obstet. Oct 1992;175(4):293-8.
| |
| * Dani R, Cundari AM, Nogueira CE, et al. Magnetic resonance cholangiopancreatography in cystic lesions of the pancreas. Pancreas. Apr 2000;20(3):313-8.
| |
| * Gumaste VV, Pitchumoni CS. Pancreatic pseudocyst. Gastroenterologist. Mar 1996;4(1):33-43.
| |
| * Kim YH, Saini S, Sahani D, Hahn PF, Mueller PR, Auh YH. Imaging diagnosis of cystic pancreatic lesions: pseudocyst versus nonpseudocyst. Radiographics. May-Jun 2005;25(3):671-85.
| |
| * Kiviluoto T, Kivisaari L, Kivilaakso E, Lempinen M. Pseudocysts in chronic pancreatitis. Surgical results in 102 consecutive patients. Arch Surg. Feb 1989;124(2):240-3.
| |
| * Laing FC, Gooding GA, Brown T, Leopold GR. Atypical pseudocysts of the pancreas: an ultrasonographic evaluation. J Clin Ultrasound. Feb 1979;7(1):27-33.
| |
| * Lang EK, Paolini RM, Pottmeyer A. The efficacy of palliative and definitive percutaneous versus surgical drainage of pancreatic abscesses and pseudocysts: a prospective study of 85 patients. South Med J. Jan 1991;84(1):55-64.
| |
| * Lee CM, Chang-Chien CS, Lin DY, et al. The real-time ultrasonography of pancreatic pseudocyst: comparison of infected and noninfected pseudocysts. J Clin Ultrasound. Jul-Aug 1988;16(6):393-8.
| |
| * Luque-de Leon E, Sarr MG. Management of pseudocysts in chronic pancreatitis. In: Problems in General Surgery. Vol 15. Philadelpha: Lippincott Williams & Wilkins;1998:123-44.
| |
| * Megibow AJ, Lavelle MT, Rofsky NM. MR imaging of the pancreas. Surg Clin North Am. Apr 2001;81(2):307-20, ix-x.
| |
| * Morel P, Rohner A. Surgery for chronic pancreatitis. Surgery. Feb 1987;101(2):130-5.
| |
| * Morgan DE, Baron TH, Smith JK, et al. Pancreatic fluid collections prior to intervention: evaluation with MR imaging compared with CT and US. Radiology. Jun 1997;203(3):773-8.
| |
| * Pansky B. Pancreas. In: Review of Gross Anatomy. 4th ed. New York: Macmillan Publishing Co;1979:332-3.
| |
| * Pitchumoni CS, Agarwal N. Pancreatic pseudocysts. When and how should drainage be performed?. Gastroenterol Clin North Am. Sep 1999;28(3):615-39.
| |
| * Rao R, Fedorak I, Prinz RA. Effect of failed computed tomography-guided and endoscopic drainage on pancreatic pseudocyst management. Surgery. Oct 1993;114(4):843-7; discussion 847-9.
| |
| * Rattner DW, Warshaw AL. Surgical intervention in acute pancreatitis. Crit Care Med. Jan 1988;16(1):89-95.
| |
| * Scott-Conner C, Dawson DL. Internal drainage of pancreatic pseudocysts. In: Operative Anatomy. Philadelphia: Lippincott;1993:427-30.
| |
| * Siegelman SS, Copeland BE, Saba GP, et al. CT of fluid collections associated with pancreatitis. AJR Am J Roentgenol. Jun 1980;134(6):1121-32.
| |
| * Stanley JC, Frey CF, Miller TA, et al. Major arterial hemorrhage: a complication of pancreatic pseudocysts and chronic pancreatitis. Arch Surg. Apr 1976;111(4):435-40.
| |
| * Teh SH, Pham TH, Lee A, Stavlo PL, Hanna AM, Moir C. Pancreatic pseudocyst in children: the impact of management strategies on outcome. J Pediatr Surg. Nov 2006;41(11):1889-93.
| |
| * vanSonnenberg E, Wittich GR, Casola G, et al. Percutaneous drainage of infected and noninfected pancreatic pseudocysts: experience in 101 cases. Radiology. Mar 1989;170(3 Pt 1):757-61.
| |
| * Vick CW, Simeone JF, Ferrucci JT Jr, et al. Pancreatitis-associated fluid collections involving the spleen: sonographic and computed tomographic appearance. Gastrointest Radiol. 1981;6(3):247-50.
| |
| * Vitas GJ, Sarr MG. Selected management of pancreatic pseudocysts: operative versus expectant management. Surgery. Feb 1992;111(2):123-30.
| |
| * Waltman AC, Luers PR, Athanasoulis CA, Warshaw AL. Massive arterial hemorrhage in patients with pancreatitis. Complementary roles of surgery and transcatheter occlusive techniques. Arch Surg. Apr 1986;121(4):439-43.
| |
| * Yeo CJ, Bastidas JA, Lynch-Nyhan A, et al. The natural history of pancreatic pseudocysts documented by computed tomography. Surg Gynecol Obstet. May 1990;170(5):411-7.
| |
| {{refend}}
| |
|
| |
|
| ==See Also== | | ==Related Chapters== |
|
| |
|
| *[[Acute pancreatitis]] | | *[[Acute pancreatitis]] |
| *[[Chronic pancreatitis]] | | *[[Chronic pancreatitis]] |
| | *[[Walled off pancreatic necrosis]] |
|
| |
|
| ==External Links==
| |
| *[http://goldminer.arrs.org/search.php?query=Pancreatic%20pseudocyst Goldminer: Pancreatic pseudocyst]
| |
|
| |
| {{SIB}}
| |
| {{Gastroenterology}} | | {{Gastroenterology}} |
|
| |
| [[Category:Diseases]]
| |
| [[Category:Gastroenterology]]
| |
|
| |
| [[fi:Haiman pseudokysta]] | | [[fi:Haiman pseudokysta]] |
|
| |
|
| {{WikiDoc Help Menu}} | | {{WikiDoc Help Menu}} |
| {{WikiDoc Sources}} | | {{WikiDoc Sources}} |
| | |
| | [[Category:Disease]] |
| | [[Category:Gastroenterology]] |