Pancreatic cancer (patient information)
For the WikiDoc page for this topic, click here
Editor-in-Chief: Jinhui Wu
Please Join in Editing This Page and Apply to be an Editor-In-Chief for this topic: There can be one or more than one Editor-In-Chief. You may also apply to be an Associate Editor-In-Chief of one of the subtopics below. Please mail us [1] to indicate your interest in serving either as an Editor-In-Chief of the entire topic or as an Associate Editor-In-Chief for a subtopic. Please be sure to attach your CV and or biographical sketch.
What is Pancreatic cancer?
-
Pancreatic adenocarcinoma
-
Pancreatic adenocarcinoma
-
Pancreatic adenocarcinoma
The pancreas is a gland behind your stomach and in front of your spine. It produces juices that help break down food and hormones that help control blood sugar levels. Cancer of the pancreas is the fourth-leading cause of cancer death in the U.S.
Pancreatic cancer is hard to catch early. It doesn't cause symptoms right away. When you do get symptoms, they are often vague or you may not notice them. They include yellowing of the skin and eyes, pain in the abdomen and back, weight loss and fatigue. Also, because the pancreas is hidden behind other organs, health care providers cannot see or feel the tumors during routine exams. Because it is often found late and it spreads quickly, pancreatic cancer can be hard to treat. Possible treatments include surgery, radiation and chemotherapy.
What are the symptoms of Pancreatic cancer?
Pancreatic cancer is sometimes called a "silent disease" because early pancreatic cancer often does not cause symptoms. But, as the cancer grows, symptoms may include:
- Pain in the upper abdomen or upper back
- Yellow skin and eyes, and dark urine from jaundice
- Weakness
- Loss of appetite
- Nausea and vomiting
- Weight loss
These symptoms are not sure signs of pancreatic cancer. An infection or other problem could also cause these symptoms. Only a doctor can diagnose the cause of a person's symptoms. Anyone with these symptoms should see a doctor so that the doctor can treat any problem as early as possible.
Who is at risk for Pancreatic cancer?
No one knows the exact causes of pancreatic cancer. Doctors can seldom explain why one person gets pancreatic cancer and another does not. However, it is clear that this disease is not contagious. No one can "catch" cancer from another person.
Research has shown that people with certain risk factors are more likely than others to develop pancreatic cancer. A risk factor is anything that increases a person's chance of developing a disease.
Studies have found the following risk factors:
- Age -- The likelihood of developing pancreatic cancer increases with age. Most pancreatic cancers occur in people over the age of 60.
- Smoking -- Cigarette smokers are two or three times more likely than nonsmokers to develop pancreatic cancer.
- Diabetes -- Pancreatic cancer occurs more often in people who have diabetes than in people who do not.
- Being male -- More men than women are diagnosed with pancreatic cancer.
- Being African American -- African Americans are more likely than Asians, Hispanics, or whites to get pancreatic cancer.
- Family history-- The risk for developing pancreatic cancer triples if a person's mother, father, sister, or brother had the disease. Also, a family history of colon or ovarian cancer increases the risk of pancreatic cancer.
- Chronic pancreatitis -- Chronic pancreatitis is a painful condition of the pancreas. Some evidence suggests that chronic pancreatitis may increase the risk of pancreatic cancer.
Other studies suggest that exposure to certain chemicals in the workplace or a diet high in fat may increase the chance of getting pancreatic cancer.
Most people with known risk factors do not get pancreatic cancer. On the other hand, many who do get the disease have none of these factors. People who think they may be at risk for pancreatic cancer should discuss this concern with their doctor. The doctor may suggest ways to reduce the risk and can plan an appropriate schedule for checkups.
How to know you have Pancreatic cancer (Diagnosis)?
If a patient has symptoms that suggest pancreatic cancer, the doctor asks about the patient's medical history. The doctor may perform a number of procedures, including one or more of the following:
- Physical exam -- The doctor examines the skin and eyes for signs of jaundice. The doctor then feels the abdomen to check for changes in the area near the pancreas, liver, and gallbladder. The doctor also checks for ascites, an abnormal buildup of fluid in the abdomen.
- Lab tests -- The doctor may take blood, urine, and stool samples to check for bilirubin and other substances. Bilirubin is a substance that passes from the liver to the gallbladder to the intestine. If the common bile duct is blocked by a tumor, the bilirubin cannot pass through normally. Blockage may cause the level of bilirubin in the blood, stool, or urine to become very high. High bilirubin levels can result from cancer or from noncancerous conditions.
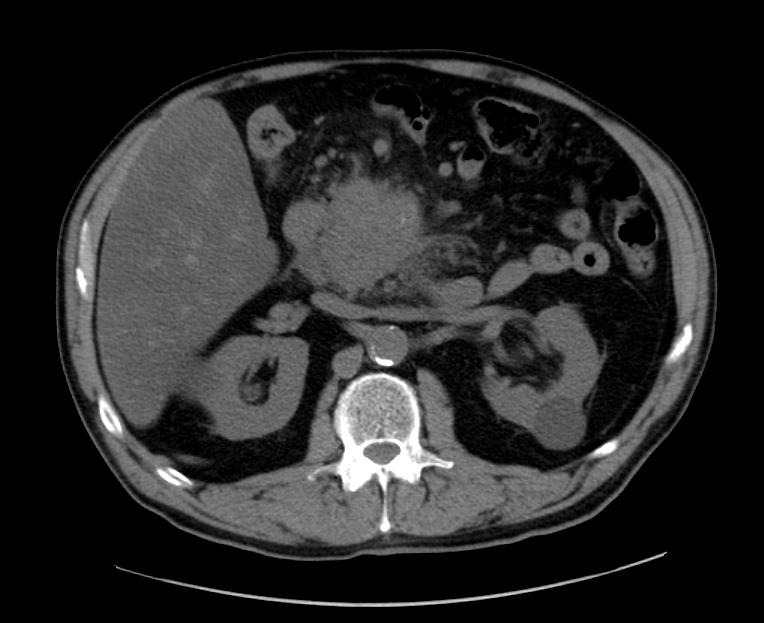
- CT scan (Computed tomography) -- An x-ray machine linked to a computer takes a series of detailed pictures. The x-ray machine is shaped like a donut with a large hole. The patient lies on a bed that passes through the hole. As the bed moves slowly through the hole, the machine takes many x-rays. The computer puts the x-rays together to create pictures of the pancreas and other organs and blood vessels in the abdomen.
- Ultrasonography -- The ultrasound device uses sound waves that cannot be heard by humans. The sound waves produce a pattern of echoes as they bounce off internal organs. The echoes create a picture of the pancreas and other organs inside the abdomen. The echoes from tumors are different from echoes made by healthy tissues.
- The ultrasound procedure may use an external or internal device, or both types:
- Transabdominal ultrasound: To make images of the pancreas, the doctor places the ultrasound device on the abdomen and slowly moves it around.
- EUS (Endoscopic ultrasound): The doctor passes a thin, lighted tube (endoscope) through the patient's mouth and stomach, down into the first part of the small intestine. At the tip of the endoscope is an ultrasound device. The doctor slowly withdraws the endoscope from the intestine toward the stomach to make images of the pancreas and surrounding organs and tissues.
- ERCP (endoscopic retrograde cholangiopancreatography) -- The doctor passes an endoscope through the patient's mouth and stomach, down into the first part of the small intestine. The doctor slips a smaller tube (catheter) through the endoscope into the bile ducts and pancreatic ducts. After injecting dye through the catheter into the ducts, the doctor takes x-ray pictures. The x-rays can show whether the ducts are narrowed or blocked by a tumor or other condition.
- PTC (percutaneous transhepatic cholangiography) -- A dye is injected through a thin needle inserted through the skin into the liver. Unless there is a blockage, the dye should move freely through the bile ducts. The dye makes the bile ducts show up on x-ray pictures. From the pictures, the doctor can tell whether there is a blockage from a tumor or other condition.
- Biopsy -- In some cases, the doctor may remove tissue. A pathologist then uses a microscope to look for cancer cells in the tissue. The doctor may obtain tissue in several ways. One way is by inserting a needle into the pancreas to remove cells. This is called fine-needle aspiration. The doctor uses x-ray or ultrasound to guide the needle. Sometimes the doctor obtains a sample of tissue during EUS or ERCP. Another way is to open the abdomen during an operation.
When to seek urgent medical care
See your doctor immediately if you feel as though you have experienced any of the above mentioned symptoms.
Treatment options
People with pancreatic cancer may have several treatment options. Depending on the type and stage, pancreatic cancer may be treated with surgery, radiation therapy, or chemotherapy. Some patients have a combination of therapies.
Surgery
may be used alone or in combination with radiation therapy and chemotherapy.
The surgeon may remove all or part of the pancreas. The extent of surgery depends on the location and size of the tumor, the stage of the disease, and the patient's general health.
- Whipple procedure: If the tumor is in the head (the widest part) of the pancreas, the surgeon removes the head of the pancreas and part of the small intestine, bile duct, and stomach. The surgeon may also remove other nearby tissues.
- Distal pancreatectomy: The surgeon removes the body and tail of the pancreas if the tumor is in either of these parts. The surgeon also removes the spleen.
- Total pancreatectomy: The surgeon removes the entire pancreas, part of the small intestine, a portion of the stomach, the common bile duct, the gallbladder, the spleen, and nearby lymph nodes.
Sometimes the cancer cannot be completely removed. But if the tumor is blocking the common bile duct or duodenum, the surgeon can create a bypass. A bypass allows fluids to flow through the digestive tract. It can help relieve jaundice and pain resulting from a blockage.
The doctor sometimes can relieve blockage without doing bypass surgery. The doctor uses an endoscope to place a stent in the blocked area. A stent is a tiny plastic or metal mesh tube that helps keep the duct or duodenum open.
After surgery, some patients are fed liquids intravenously (by IV) and through feeding tubes placed into the abdomen. Patients slowly return to eating solid foods by mouth. A few weeks after surgery, the feeding tubes are removed.
Radiation therapy
(Also called radiotherapy) uses high-energy rays to kill cancer cells. A large machine directs radiation at the abdomen. Radiation therapy may be given alone, or with surgery, chemotherapy, or both.
Radiation therapy is local therapy. It affects cancer cells only in the treated area. For radiation therapy, patients go to the hospital or clinic, often 5 days a week for several weeks.
Doctors may use radiation to destroy cancer cells that remain in the area after surgery. They also use radiation to relieve pain and other problems caused by the cancer.
Chemotherapy
Is the use of drugs to kill cancer cells. Doctors also give chemotherapy to help reduce pain and other problems caused by pancreatic cancer. It may be given alone, with radiation, or with surgery and radiation.
Chemotherapy is systemic therapy. The doctor usually gives the drugs by injection. Once in the bloodstream, the drugs travel throughout the body.
Usually chemotherapy is an outpatient treatment given at the hospital, clinic, doctor's office, or home. However, depending on which drugs are given and the patient's general health, the patient may need to stay in the hospital.
Diseases with similar symptoms
- Choledocholithiasis
- Pancreatic pseudocyst
- Cystic neoplasm
- Carcinoma of the biliary tract[1]
Where to find medical care for Pancreatic cancer
Directions to Hospitals Treating Pancreatic cancer
Prevention of pancreatic cancer
According to the American Cancer Society, there are no established guidelines for preventing pancreatic cancer, although cigarette smoking has been reported as responsible for 20-30% of pancreatic cancers.[2]
The ACS recommends keeping a healthy weight, and increasing consumption of fruits, vegetables, and whole grains while decreasing red meat intake, although there is no consistent evidence that this will prevent or reduce pancreatic cancer specifically.[3][4] In 2006 a large prospective cohort study of over 80,000 subjects failed to prove a definite association.[5] The evidence in support of this lies mostly in small case-control studies.[6]
In September 2006, a long-term study concluded that taking Vitamin D can substantially cut the risk of pancreatic cancer (as well as other cancers) by up to 50%.[7][8][9]
Several studies, including one published on 1 June 2007, indicate that B vitamins such as B12, B6, and folate, can reduce the risk of pancreatic cancer when consumed in food, but not when ingested in vitamin tablet form.[10][11]
What to expect (Outook/Prognosis)
Patients diagnosed with pancreatic cancer typically have a poor prognosis partly because the cancer usually causes no symptoms early on, leading to locally advanced or metastatic disease at time of diagnosis. Median survival from diagnosis is around 3 to 6 months; 5-year survival is less than 5%.[12] With 37,170 cases diagnosed in the United States in 2007, and 33,700 deaths, pancreatic cancer has one of the highest fatality rates of all cancers and is the fourth highest cancer killer in the United States among both men and women. Although it accounts for only 2.5% of new cases, pancreatic cancer is responsible for 6% of cancer deaths each year.[13]
Sources
- ↑ http://www.wrongdiagnosis.com/p/pancreatic_cancer/misdiag.htm
- ↑ ^ "ACS :: Can Cancer of the Pancreas be Prevented?". http://www.cancer.org/docroot/CRI/content/CRI_2_4_2X_Can_pancreatic_cancer_be_prevented_34.asp?rnav=cri. Retrieved on 2007-12-13.
- ↑ ^ Coughlin, SS; Calle EE, Patel AV, Thun MJ. (December 2000). "Predictors of pancreatic cancer mortality among a large cohort of United States adults". Cancer Causes Control. 11 (10): 915–23.. doi:10.1023/A:1026580131793. PMID 11142526.
- ↑ ^ Zheng, W; et al. (September 1993). "A cohort study of smoking, alcohol consumption, and dietary factors for pancreatic cancer (United States)". Cancer Causes Control. 4 (5): 477–82.. doi:10.1007/BF00050867. PMID 8218880.
- ↑ ^ Larsson, Susanna; Niclas Håkansson, Ingmar Näslund, Leif Bergkvist and Alicja Wolk (February 2006). "Fruit and vegetable consumption in relation to pancreatic cancer risk: a prospective study". Cancer Epidemiology Biomarkers & Prevention 15: 301–305. doi:10.1158/1055-9965.EPI-05-0696. PMID 16492919.
- ↑ ^ "Vegetable and fruit intake and pancreatic cancer in a population-based case-control study in the San Francisco bay area.". Cancer epidemiology, biomarkers & prevention. pubMed.gov. 2005-08. http://www.ncbi.nlm.nih.gov/pubmed/16172215. Retrieved on 2009-01-14.
- ↑ ^ BBC NEWS | Health | Vitamin D 'slashes cancer risk'
- ↑ ^ Vitamin D May Cut Pancreatic Cancer
- ↑ ^ http://www.forbes.com/forbeslife/health/feeds/hscout/2006/09/14/hscout534925.html
- ↑ ^ Schernhammer E, Wolpin B, Rifai N, et al. (June 2007). "Plasma folate, vitamin B6, vitamin B12, and homocysteine and pancreatic cancer risk in four large cohorts". Cancer Res. 67 (11): 5553–60. doi:10.1158/0008-5472.CAN-06-4463. PMID 17545639. http://cancerres.aacrjournals.org/cgi/content/abstract/67/11/5553.
- ↑ ^ "United Press International - Consumer Health Daily - Briefing". http://www.upi.com/Consumer_Health_Daily/Briefing/2007/06/01/pancreatic_cancer_risk_cut_by_b6_b12/3712/. Retrieved on 2007-06-04.
- ↑ # ^ WHO | Cancer
- ↑ ^ Jemal A, Siegel R, Ward E, Murray T, Xu J, Thun MJ (2007). "Cancer statistics, 2007". CA Cancer J Clin 57 (1): 43–66. doi:10.3322/canjclin.57.1.43. PMID 17237035. http://caonline.amcancersoc.org/cgi/content/full/57/1/43.