|
|
| (25 intermediate revisions by 8 users not shown) |
| Line 1: |
Line 1: |
| {{SI}}
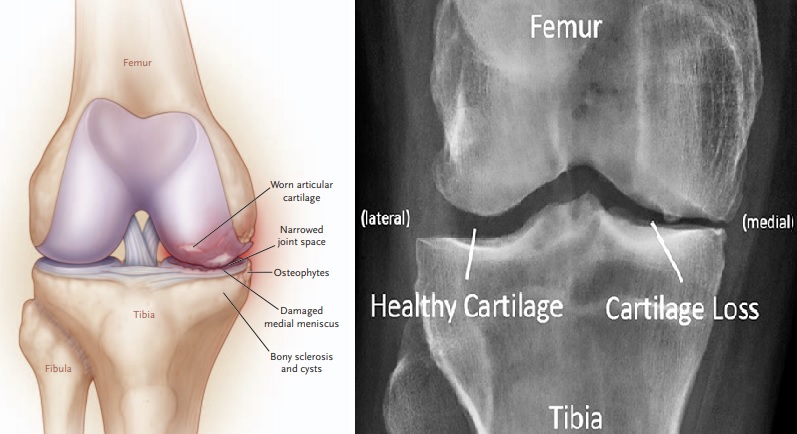
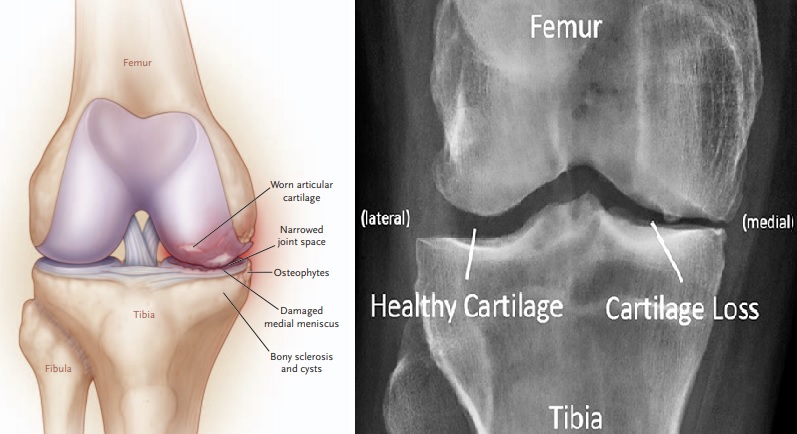
| | [[File:TITLE.jpg|thumb|Osteoarthritis (OA) of the Medial Side of the Knee.]] |
| | __NOTOC__ |
|
| |
|
| '''Editor-In-Chief:''' [[User:Bobby Schwartz|Robert G. Schwartz, M.D.]] [mailto:RGSHEAL@aol.com], [http://www.piedmontpmr.com Piedmont Physical Medicine and Rehabilitation, P.A.] | | '''For patient information click [[{{PAGENAME}} (patient information)|here]]''' |
| | {{Infobox_Disease }} |
| | {{Osteoarthritis}} |
| | [[File:TITLE.jpg|thumb|Osteoarthritis (OA) ]] |
| | {{CMG}}; {{AE}}[[User:DrMars|Mohammadmain Rezazadehsaatlou]] [2]; [[User:Bobby Schwartz|Robert G. Schwartz, M.D.]] [mailto:RGSHEAL@aol.com], [http://www.piedmontpmr.com Piedmont Physical Medicine and Rehabilitation, P.A.], [3] [[User:Irfan Dotani|Irfan Dotani]] |
|
| |
|
| {{EJ}} | | {{SK}} OA; Ostearthritis; Ostarthritis; Osteoarthrosis; Arthritis; Degenerative arthritis; Degenerative joint disease; DJD; Arthrosis; Hypertrophic osteoarthritis; Facets disease, Facets syndrome; Osteoarthrosis deformans; Malum senile, Morbus senilis; Wear-and-tear arthritis. |
| | ==[[Osteoarthritis overview|Overview]]== |
| | ==[[Osteoarthritis historical perspective|Historical Perspective]]== |
| | ==[[Osteoarthritis classification|Classification]]== |
| | ==[[Osteoarthritis pathophysiology|Pathophysiology]]== |
|
| |
|
| | ==[[Osteoarthritis causes|Causes]]== |
|
| |
|
| ==Overview== | | ==[[Osteoarthritis differential diagnosis|Differentiating Osteoarthritis from other Diseases]]== |
| {{Infobox_Disease |
| |
| Name = Osteoarthritis |
| |
| Image = Gonarthrose-Knorpelaufbrauch.jpg |
| |
| Caption = |
| |
| DiseasesDB = 9313 |
| |
| ICD10 = {{ICD10|M|15||m|15}}-{{ICD10|M|19||m|15}}, {{ICD10|M|47||m|45}} |
| |
| ICD9 = {{ICD9|715}} |
| |
| ICDO = |
| |
| OMIM = 165720 |
| |
| MedlinePlus = 000423 |
| |
| eMedicineSubj = med |
| |
| eMedicineTopic = 1682 |
| |
| eMedicine_mult = {{eMedicine2|orthoped|427}} {{eMedicine2|pmr|93}} {{eMedicine2|radio|492}} |
| |
| MeshID = D010003 |
| |
| }}
| |
| {{Search infobox}}
| |
| '''Osteoarthritis / Osteoarthrosis''' ('''OA''', also known as '''degenerative arthritis''', '''degenerative joint disease''', '''arthrosis''' or in more colloquial terms "wear and tear"), is a condition in which low-grade inflammation results in pain in the joints, caused by wearing of the [[cartilage]] that covers and acts as a cushion inside joints. As the bone surfaces become less well protected by cartilage, the patient experiences pain upon weight bearing, including walking and standing. Due to decreased movement because of the pain, regional muscles may [[atrophy]], and [[ligament]]s may become more lax. OA is the most common form of [[arthritis]]. The word is derived from the Greek word "''osteo''", meaning "of the bone", "''arthro''", meaning "joint", and "''itis''", meaning [[inflammation]], although many sufferers have little or no inflammation.
| |
|
| |
|
| OA affects nearly 21 million people in the [[United States]], accounting for 25% of visits to [[primary care physician]]s, and half of all [[NSAID]] (Non-Steroidal Anti-Inflammatory Drugs) [[Medical prescription|prescriptions]]. It is estimated that 80% of the population will have [[radiograph]]ic evidence of OA by age 65, although only 60% of those will be [[symptomatic]].<ref>Green GA. ''Understanding NSAIDS: from aspirin to COX-2''. Clin Cornerstone 2001; 3:50-59. PMID 11464731.</ref> Treatment is with NSAIDs, local injections of [[glucocorticoid]] or [[hyaluronan]], and in severe cases, with [[joint replacement]] surgery. There has been no cure for OA, as cartilage has not been induced to regenerate. However, if OA is caused by cartilage damage (for example as a result of an injury) Autologous Chondrocyte Implantation may be a possible treatment. <ref>[http://biomed.brown.edu/Courses/BI108/BI108_1999_Groups/Cartilage_Team/christine/HowitWorks.html Autologous Chondrocyte Implantation]</ref> Clinical trials employing [[tissue engineering|tissue-engineering]] methods have demonstrated regeneration of cartilage in damaged knees, including those that had progressed to osteoarthritis.<ref>{{cite journal |author=Hollander AP, Dickinson SC, Sims TJ, ''et al'' |title=Maturation of tissue engineered cartilage implanted in injured and osteoarthritic human knees |journal=Tissue Eng. |volume=12 |issue=7 |pages=1787-98 |year=2006 |pmid=16889509 |doi=10.1089/ten.2006.12.1787}}</ref> Further, in January 2007, Johns Hopkins University was offering to license a technology of this kind, <ref>[http://www.birchbob.com/MarketingPieces/jhu/indexJE.htm Repairing knee joints by growing new cartilage using an injectable hydrogel]</ref> listing several clinical competitors in its market analysis.
| | ==[[Osteoarthritis epidemiology and demographics|Epidemiology and Demographics]]== |
|
| |
|
| ==Signs and symptoms== | | ==[[Osteoarthritis risk factors|Risk Factors]]== |
| The main symptom is [[chronic pain]], causing loss of mobility and often stiffness. "Pain" is generally described as a sharp ache, or a burning sensation in the associated [[muscle]]s and [[tendon]]s. OA can cause a crackling noise (called "[[crepitus]]") when the affected joint is moved or touched, and patients may experience muscle [[spasm]] and contractions in the tendons. Occasionally, the joints may also be filled with fluid. Humid weather increases the pain in many patients.
| |
|
| |
|
| OA commonly affects the [[hands]], feet, [[vertebral column|spine]], and the large weight-bearing joints, such as the [[hip joint|hips]] and [[knee]]s, although in theory, any joint in the body can be affected. As OA progresses, the affected joints appear larger, are stiff and painful, and usually feel ''worse'', the more they are used throughout the day, thus distinguishing it from [[rheumatoid arthritis]].
| | ==[[Osteoarthritis screening|Screening]]== |
|
| |
|
| In smaller joints, such as at the fingers, hard bony enlargements, called [[Heberden's node]]s (on the distal interphalangeal joints) and/or [[Bouchard's nodes]] (on the proximal interphalangeal joints), may form, and though they are not necessarily painful, they do limit the movement of the fingers significantly. OA at the toes leads to the formation of [[bunion]]s, rendering them red or swollen.
| | ==[[Osteoarthritis natural history, complications and prognosis|Natural History, Complications and Prognosis]]== |
| | |
| OA is the most common cause of "water on the knee", an accumulation of excess fluid in or around your knee joint. <ref>[http://www.mayoclinic.com/health/water-on-the-knee/DS00662 Water on the knee], MayoClinic.com</ref>
| |
| | |
| == Causes ==
| |
| Osteoarthritis often affects multiple members of the same family, suggesting that there is [[hereditary]] susceptibility to this condition. A number of studies have shown that there is a greater prevalence of the disease between siblings and especially [[Twin#Identical twins|identical twins]], indicating a hereditary basis. Up to 60% of OA cases are thought to result from genetic factors. Researchers are also investigating the possibility of [[Allergy|allergies]], [[infection]]s, or [[Mycosis|fungi]] as a cause. There is some evidence that allergies, whether fungal, infectious or systemically induced, may be a significant contributing factor to the appearance of osteoarthritis in a synovial sac. | |
| | |
| == Two types ==
| |
| === Primary ===
| |
| This type of OA is a chronic degenerative disorder related to but not caused by [[aging]], as there are people well into their nineties who have no clinical or functional signs of the disease. As a person ages, the water content of the [[cartilage]] decreases due to a reduced [[proteoglycan]] content, thus causing the cartilage to be less resilient. Without the protective effects of the [[proteoglycan]]s, the [[collagen]] fibers of the cartilage can become susceptible to degradation and thus exacerbate the degeneration. [[Inflammation]] of the surrounding [[joint capsule]] can also occur, though often mild (compared to that which occurs in [[rheumatoid arthritis]]). This can happen as breakdown products from the cartilage are released into the synovial space, and the cells lining the joint attempt to remove them. New [[bone]] outgrowths, called "spurs" or osteophytes, can form on the margins of the joints, possibly in an attempt to improve the congruence of the articular cartilage surfaces. These bone changes, together with the inflammation, can be both painful and debilitating.
| |
| | |
| === Secondary ===
| |
| This type of OA is caused by other factors or diseases but the resulting pathology is the same as for primary OA:
| |
| * [[Congenital]] [[disease|disorder]]s, such as:
| |
| ** Congenital hip luxation
| |
| ** People with abnormally-formed joints (e.g. [[hip dysplasia]]) are more vulnerable to OA, as added stress is specifically placed on the joints whenever they move. [However, recent studies have shown that double-jointedness may actually protect the fingers and hand from osteoarthritis.]
| |
| * Cracking joints—the evidence is weak at best that this has any connection to arthritis [http://elfstrom.com/arthritis/knuckle-cracking.html].
| |
| * [[Diabetes]].
| |
| * [[Inflammation|Inflammatory]] diseases (such as Perthes' disease), ([[Lyme disease]]), and all chronic forms of arthritis (e.g. [[costochondritis]], [[gout]], and [[rheumatoid arthritis]]). In gout, [[uric acid]] crystals cause the cartilage to degenerate at a faster pace.
| |
| * [[Injury]] to joints, as a result of an accident.
| |
| * A joint [[infection]], e.g. from an injury.
| |
| * [[Hormone|Hormonal]] disorders.
| |
| * Ligamentous deterioration or instability may be a factor.
| |
| * [[Obesity]]. Obesity puts added weight on the joints, especially the knees.
| |
| * [[Osteopetrosis]] (High bone density).
| |
| * Sports injuries, or similar injuries from exercise or work. Certain sports, such as running or football, put undue pressure on the knee joints. Injuries resulting in broken ligaments can lead to instability of the joint and over time to wear on the cartilage and eventually osteoarthritis.
| |
| * [[Pregnancy]]
| |
| * [[Alkaptonuria]]
| |
| * [[Hemochromatosis]] and [[Wilson's disease]]
| |
|
| |
|
| ==Diagnosis== | | ==Diagnosis== |
| [[Diagnosis]] is normally done through [[x-ray]]s. This is possible because loss of cartilage, subchondral ("below cartilage") [[sclerosis]], subchondral [[cyst]]s, narrowing of the joint space between the articulating bones, and [[bone spur]] formation (osteophytes) show up clearly on x-rays. Plain films, however, often do not correlate well with the findings of physical examination of the affected joints. | | [[Osteoarthritis diagnostic criteria|Diagnostic Criteria]] | [[Osteoarthritis history and symptoms|History and Symptoms]] | [[Osteoarthritis physical examination|Physical Examination]] | [[Osteoarthritis laboratory findings|Laboratory Findings]] | [[Osteoarthritis x ray|X Ray]] | [[Osteoarthritis CT|CT]] | [[Osteoarthritis MRI|MRI]] | [[Osteoarthritis other imaging findings|Other Imaging Findings]] | [[Osteoarthritis other diagnostic studies|Other Diagnostic Studies]] |
| | |
| With or without other techniques, such as [[Magnetic resonance imaging|MRI]] (magnetic resonance imaging), [[arthrocentesis]] and [[arthroscopy]], diagnosis can be made by a careful study of the duration, location, the character of the joint symptoms, and the appearance of the joints themselves. As yet, there are no methods available to detect OA in its early and potentially treatable stages.
| |
| | |
| In 1990, the [http://www.rheumatology.org/about/index.asp?aud=mem|American College of Rheumatology], using data from a multi-center study, developed a set of criteria for the [http://patients.uptodate.com/topic.asp?file=arth_rhe/2266|diagnosis of hand osteoarthritis] based on hard tissue enlargement and swelling of certain joints. These criteria were found to be 92% [[sensitivity (tests)|sensitive]] and 98% [[specificity (tests)|specific]] for hand osteoarthritis versus other entities such as [[rheumatoid arthritis]] and [[spondyloarthropathy|spondyloarthropities]] <ref>{{cite journal |author=Altman R, Alarcón G, Appelrouth D, ''et al'' |title=The American College of Rheumatology criteria for the classification and reporting of osteoarthritis of the hand |journal=Arthritis Rheum. |volume=33 |issue=11 |pages=1601-10 |year=1990 |pmid=2242058 |doi=}}</ref>.
| |
|
| |
|
| ==Treatment== | | ==Treatment== |
| | [[Osteoarthritis medical therapy|Medical Therapy]] | [[Osteoarthritis surgery|Surgery]] | [[Osteoarthritis primary prevention|Primary Prevention]] | [[Osteoarthritis secondary prevention|Secondary Prevention]] | [[Osteoarthritis cost-effectiveness of therapy|Cost-Effectiveness of Therapy]] | [[Osteoarthritis future or investigational therapies|Future or Investigational Therapies]] | [[Stem cell|Stem cell]] |
|
| |
|
| Generally speaking, the process of clinically detectable osteoarthritis is irreversible, and typical treatment consists of medication or other interventions that can reduce the pain of OA and thereby improve the function of the joint.
| | ==Case Studies== |
| | | :[[Osteoarthritis case study one|Case #1]] |
| Application of heat — often moist heat — eases inflammation and swelling in the joints, and can help improve [[blood circulation|circulation]], which has a healing effect on the local area.
| |
| | |
| ===Coping skills and lifestyle changes===
| |
| | |
| No matter what the severity, or where the OA lies, conservative measures, such as weight control, appropriate rest and [[exercise]], and the use of mechanical support devices are usually beneficial to sufferers. In the case of OA of the knees, knee braces, a cane, or a walker can be a helpful aid for walking and support. Regular exercise, if possible, in the form of [[walking]] or [[swimming]], is encouraged. Applying local heat before, and cold packs after exercise, can help relieve pain and inflammation, as can [[relaxation technique]]s. Weight loss can relieve joint stress and may delay progression. Proper advice and guidance by a health care provider is important in OA management, enabling people with this condition to improve their quality of life.
| |
| | |
| In 2002, a randomized, blinded assessor trial was published showing a positive effect on hand function with patients who practiced home joint protection exercises (JPE). Grip strength, the primary outcome parameter, increased by 25% in the exercise group versus no improvement in the control group. Global hand function improved by 65% for those undertaking JPE. <ref>{{cite journal |author=Stamm TA, Machold KP, Smolen JS, ''et al'' |title=Joint protection and home hand exercises improve hand function in patients with hand osteoarthritis: a randomized controlled trial |journal=Arthritis Rheum. |volume=47 |issue=1 |pages=44-9 |year=2002 |pmid=11932877 |doi=}}</ref>
| |
| | |
| Dealing with chronic pain can be difficult and result in [[clinical depression|depression]]. Communicating with other patients and caregivers can be helpful, as can maintaining a positive attitude. People who take control of their treatment, communicate with their health care provider, and actively manage their arthritis experience can reduce pain and improve function.
| |
| | |
| ===Dietary===
| |
| | |
| Supplements which may be useful for treating OA include:
| |
| | |
| ====Glucosamine====
| |
| A molecule derived from glucosamine is used by the body to make some of the components of cartilage and synovial fluid. Supplemental glucosamine may improve symptoms of OA and delay its progression.<ref name="pmid15855241">{{cite journal |author=Poolsup N, Suthisisang C, Channark P, Kittikulsuth W |title=Glucosamine long-term treatment and the progression of knee osteoarthritis: systematic review of randomized controlled trials |journal=The Annals of pharmacotherapy |volume=39 |issue=6 |pages=1080-7 |year=2005 |pmid=15855241 |doi=10.1345/aph.1E576}}</ref> However, a large study suggests that glucosamine is not effective in treating OA of the knee.<ref>McAlindon T, Formica M, LaValley M, Lehmer M, Kabbara K. ''Effectiveness of glucosamine for symptoms of knee osteoarthritis: Results from an internet-based randomized double-blind controlled trial.'' Am J Med 2004; 117:643-9. PMID 15501201.</ref> A subsequent [[meta-analysis]] that includes this trial concluded that glucosamine hydrochloride is not effective and that the effect of glucosamine sulfate is uncertain.<ref name="pmid17599746">{{cite journal |author=Vlad SC, Lavalley MP, McAlindon TE, Felson DT |title=Glucosamine for pain in osteoarthritis: Why do trial results differ? |journal= |volume=56 |issue=7 |pages=2267-2277 |year=2007 |pmid=17599746 |doi=10.1002/art.22728}}</ref>
| |
| | |
| ====Chondroitin====
| |
| A [[meta-analysis]] of [[randomized controlled trials]] found no benefit from chondroitin.<ref name="pmid17438317">{{cite journal |author=Reichenbach S, Sterchi R, Scherer M, ''et al'' |title=Meta-analysis: chondroitin for osteoarthritis of the knee or hip |journal=Ann. Intern. Med. |volume=146 |issue=8 |pages=580-90 |year=2007 |pmid=17438317 |doi=}}</ref>
| |
| | |
| ====Other supplements====
| |
| *'''Boswellia''', an herbal supplement known in Aryuvedic medicine. It is widely available in health food stores and online.
| |
| *'''[[Antioxidant]]s''', including [[Vitamin C|vitamins C]] and [[Vitamin E|E]] in both foods and supplements, provide pain relief from OA. <ref>McAlindon TE, Jacques P, Zhang Y, et al. Do antioxidant micronutrients protect against the development and progression of knee osteoarthritis? Arthritis Rheum 1996; 39:648-656</ref>
| |
| | |
| * '''[[Hydrolyzed collagen (hydrolysate)]]''' (a gelatin product) may also prove beneficial in the relief of OA symptoms, as substantiated in a German study by Beuker F. et al. and Seeligmuller et al. In their 6-month placebo-controlled study of 100 elderly patients, the verum group showed significant improvement in joint mobility.
| |
| | |
| * '''[[Ginger]] (rhizome) extract''' - has improved knee symptoms moderately.<ref>Altman RD, Marcussen KC. Arthritis Rheum. 2001 Nov; 44(11):2531-8</ref>
| |
| | |
| * '''[[Methylsulfonylmethane|Methylsulfonylmethane (MSM)]]''': A small study by Kim et al. suggested that MSM significantly reduced pain and improved physical functioning in OA patients without major adverse events (Kim et al). The authors cautioned that although this short pilot study did not address the long-term safety and usefulness of MSM, they suggest that physicians should consider its use for certain osteoarthritis patients.
| |
| | |
| * '''[[S-adenosyl methionine]]''': small scale studies have shown it to be as effective as [[NSAID]]s in reducing pain, although it takes about four weeks for the effect to take place.
| |
| | |
| * '''[[Selenium]]''' deficiency has been correlated with a higher risk and severity of OA, therefore selenium supplementation may reduce this risk.<ref>{{cite web |url=http://www.unc.edu/news/archives/nov05/jordan111005.htm |title=UNC News release -- Study links low selenium levels with higher risk of osteoarthritis |accessdate=2007-06-22 |format= |work=}}</ref>
| |
| | |
| * '''Vitamins B9 ([[folate]]) and [[Vitamin B12|B12]]''' ([[cobalamin]]) taken in large doses significantly reduced OA hand pain, presumbably by reducing systemic inflammation.<ref>Flynn MA, Irvin W, Krause G. J Am Coll Nutr. 1994 Aug; 13(4):351-6.</ref>
| |
| | |
| * '''[[Vitamin D]] deficiency''' has been reported in patients with OA, and supplementation with [[Vitamin D3]] is recommended for pain relief.<ref>Arabelovic S, McAlindon TE. Curr Rheumatol Rep. 2005 Mar; 7(1):29-35.</ref>
| |
| | |
| * Bone Morphogenetic Protein 6 (BMP-6) has recently been shown to have a functional role in the maintenance of joint integrity and is now being produced in an orally ingested form. <ref> K. Bobacz, R. Gurber, A Soleiman, L. Erlacher, J.S. Smolen, and W.B. Grainger, Arthritis & Rheumatism 2003 Sep; 48(9) 2501 </ref>
| |
| | |
| Other nutritional changes shown to aid in the treatment of OA include decreasing [[saturated fat]] intake<ref>Wilhelmi G. Z Rheumatol. 1993 May-Jun; 52(3):174-9. Vasishta VG et al, Rotational Field Magnetic Resonance (RFQMR) in treatment of osteoarthritis of the knee joint, Indian Journal of Aerospace Medicine, 48 (2), 2004; 1-7.</ref> and using a low energy diet to decrease body fat.<ref>Christensen R. Osteoarthritis Cartilage. 2005 Jan; 13(1):20-7.</ref> Lifestyle change may be needed for effective symptomatic relief, especially for knee OA.<ref>De Filippis L et al. Reumatismo. 2004 Jul-Sep; 56(3):169-84.</ref> Reducing sugar, processed foods, fatty foods and [[Solanaceae|nightshade vegetables]] have helped many. According to Dr. John McDougall,<ref>{{cite web |url=http://www.drmcdougall.com/med_hot_arthritis.html |title=Hot Topics: Arthritis |accessdate=2007-06-22 |format= |work=}}</ref> a low fat vegetarian diet can reduce arthritis symptoms. A macrobiotic diet has been known to reduce symptoms as well.
| |
| | |
| ===Medications===
| |
| ====Acetaminophen====
| |
| A mild pain reliever may be sufficiently efficacious. [[Acetaminophen]] (tylenol/paracetamol), is commonly used to treat the pain from OA, although unlike NSAIDs, acetaminophen does not treat the inflammation. A [[randomized controlled trial]] comparing [[acetaminophen]] to [[ibuprofen]] in x-ray proven mild to moderate osteoarthritis of the hip or knee found that equal benefit.<ref name="pmid2052056">{{cite journal |author=Bradley JD, Brandt KD, Katz BP, Kalasinski LA, Ryan SI |title=Comparison of an antiinflammatory dose of ibuprofen, an analgesic dose of ibuprofen, and acetaminophen in the treatment of patients with osteoarthritis of the knee |journal=N. Engl. J. Med. |volume=325 |issue=2 |pages=87-91 |year=1991 |pmid=2052056 |doi=}}</ref> However, [[acetaminophen]] at a dose of 4 grams per day can increase [[liver function test]]s.<ref name="pmid16820551">{{cite journal |author=Watkins PB, Kaplowitz N, Slattery JT, ''et al'' |title=Aminotransferase elevations in healthy adults receiving 4 grams of acetaminophen daily: a randomized controlled trial |journal=JAMA |volume=296 |issue=1 |pages=87-93 |year=2006 |pmid=16820551 |doi=10.1001/jama.296.1.87}}</ref>
| |
| | |
| ====Non-steroidal anti-inflammatory drugs====
| |
| In more severe cases, [[non-steroidal anti-inflammatory drug]]s (NSAID) may reduce both the pain and inflammation. These include medications such as [[diclofenac]], [[ibuprofen]] and [[naproxen]]. High doses are often required. All NSAIDs act by inhibiting the formation of [[prostaglandin]]s, which play a central role in inflammation and pain. However, these drugs are rather taxing on the [[gastrointestinal tract]], and may cause [[stomach]] upset, [[cramp]]ing, [[diarrhoea]], and [[peptic ulcer]].
| |
| | |
| ====COX-2 selective inhibitors====
| |
| Another type of NSAID, [[COX-2 selective inhibitor]]s (such as [[celecoxib]], and the withdrawn [[rofecoxib]] and [[valdecoxib]]) reduce this risk substantially. These latter NSAIDs carry an elevated risk for [[cardiovascular disease]], and some have now been withdrawn from the market.
| |
| | |
| ====Corticosteroids====
| |
| Most doctors nowadays loath the use of [[steroid]]s in the treatment of OA as their effect is modest and the adverse effects may outweigh the benefits.
| |
| | |
| ====Narcotics====
| |
| For severe pain, [[narcotic]] pain relievers such as [[tramadol]], and eventually [[opioid]]s ([[hydrocodone]], [[oxycodone]] or [[morphine]]) may be necessary; these should be reserved for very severe cases, and are rarely medically necessary for [[chronic pain]].
| |
| | |
| ===Topical===
| |
| "Topical treatments" are treatments designed for local application and action. Some [[NSAID]]s are available for topical use (e.g. [[ibuprofen]] and [[diclofenac]]) and may improve symptoms without having systemic side-effects.
| |
| | |
| [[emollient|Cream]]s and [[lotion]]s, containing [[capsaicin]], are effective in treating pain associated with OA if they are applied with sufficient frequency.
| |
| | |
| Severe pain in specific joints can be treated with local [[lidocaine]] [[Injection (medicine)|injection]]s or similar local [[anaesthetic]]s, and glucocorticoids (such as [[hydrocortisone]]). Corticosteroids (cortisone and similar agents) may temporarily reduce the pain.
| |
|
| |
|
| ===Surgery=== | | ==Related Chapters== |
| If the above management is ineffective, [[joint replacement]] [[surgery]] may be required. Individuals with very painful OA joints may require surgery such as fragment removal, repositioning bones, or fusing bone to increase stability and reduce pain.
| |
| | |
| ===Other approaches===
| |
| | |
| There are various other modalities in use for osteoarthritis:
| |
| | |
| ====Acupuncture====
| |
| A [[meta-analysis]] of [[randomized controlled trials]] of [[acupuncture]] for knee osteoarthritis concluded "clinically relevant benefits, some of which may be due to [[placebo]] or expectation effects".<ref name="pmid17577006">{{cite journal |author=Manheimer E, Linde K, Lao L, Bouter LM, Berman BM |title=Meta-analysis: acupuncture for osteoarthritis of the knee |journal=Ann. Intern. Med. |volume=146 |issue=12 |pages=868-77 |year=2007 |pmid=17577006 |doi=}}</ref>
| |
| | |
| ====Low level laser therapy====
| |
| Low level laser therapy ; this is a light wave based treatment that may reduce pain. The treatment is painless, inexpensive and without risks or side effects. Unfortunately, it may not actually have any real benefits.[http://www.jr2.ox.ac.uk/bandolier/booth/alternat/lasarth.html].
| |
| | |
| ====Rotational Field Quantum Magnetic Resonance (“RFQMR”)====
| |
| Rotational Field Quantum Magnetic Resonance (“RFQMR”) has been claimed to be effective for regeneration of cartilage in the knee joints. A three-year trial of this method involving 500 patients has been conducted at the Indian Airforce's Institute of Aerospace Medicine, Bangalore (India). RFQMR Technology is claimed to utilize sub-radio and near-radio frequency electromagnetic radiation focused onto tissues to alter proton spin inside and outside cells, generating streaming voltage potentials resulting in stimulation of cartilage growth. The treatment is said to be painless and is claimed to be safe. Pre and post 3 months MRI showed significant increase in cartilage growth.
| |
| | |
| ====Prolotherapy====
| |
| Prolotherapy (proliferative therapy); this is the injection of an irritant substance (such as dextrose) to create an acute inflammatory reaction. It is claimed to strengthen and heal damaged tissues including ligaments, tendons and cartilage as part of this reaction. The injection is painful (like corticosteroids or hyaluronic acid) and may cause an increase in pain for a few days afterwards. The only other significant risk is the rare possibility of infection.
| |
| | |
| ====Radiosynoviorthesis====
| |
| Radiosynoviorthesis: A radioactive isotope (a beta-ray emitter with a brief half-life) is injected into the joint to soften the tissue. Due to the involvement of radioactive material, this is an elaborate and costly procedure, but it has a success rate of around 80%.
| |
| | |
| ==Prognosis==
| |
| The most common course of OA is an intermittent, progressive worsening of symptoms over time, although in some patients the disease stabilizes. Prognosis also varies depending on which joint is involved.
| |
| | |
| Factors associated with progression of OA:
| |
| *Knees: High [[body mass index]], [[genu varum|varus]] or [[genu valgum|valgus knee]] [[deformity]].
| |
| *Hips: Night pain, presence of [[femur|femoral]] osteophytes, and subchondral sclerosis in females.
| |
| *Hands: Older age.
| |
| | |
| ==References==
| |
| {{Reflist|2}}
| |
| | |
| ==See also==
| |
| *[[Back pain]] | | *[[Back pain]] |
| *[[Chronic pain]] | | *[[Chronic pain]] |
| Line 177: |
Line 41: |
|
| |
|
| == External links == | | == External links == |
| * [http://www.arthritis.org/disease-center.php?disease_id=32 Osteoarthritis The Arthritis Foundation]
| |
| * [http://www.arthritiscare.org.uk Arthritis Care]
| |
| * [http://osteoarthritisoa.com/factorfictionOA.php Osteoarthritis fact and fiction]
| |
| * [http://my.webmd.com/content/article/78/95594.htm WebMDHealth: Osteoarthritis Basics at WebMD]
| |
| * [http://www.medicinenet.com/osteoarthritis/article.htm MedicineNet.com: Osteoarthritis]
| |
| * [http://www.nlm.nih.gov/medlineplus/osteoarthritis.html MedlinePlus:Osteoarthritis at National Institutes of Health] | | * [http://www.nlm.nih.gov/medlineplus/osteoarthritis.html MedlinePlus:Osteoarthritis at National Institutes of Health] |
| * [http://www.oatrial.com Osteoarthritis Clinical Trials Resource]
| |
| * [http://www.umm.edu/patiented/articles/what_osteoarthritis_000035_1.htm Overview at University of Maryland]
| |
| * [http://www.spine-health.com/topics/cd/osteound/osteound01.html Understanding Osteoarthritis of the Spine]
| |
| * [http://www.arthritismd.com/osteoarthritis.html Physician submitted articles]
| |
| * [http://www.osteo.co.il/osteoarthritis_and_osteopathy.html Understanding osteoarthritis]
| |
| * [http://www.paremanifesto.org Focuses on living with arthritis with links to support groups in 16 different countries]
| |
| * [http://www.sbfhealthcare.com Rotational Field Quantum Magnetic Resonance (RFQMR) in treatment of osteoarthritis]
| |
| * [http://news.bbc.co.uk/1/hi/health/1556883.stm BBC Coverage of Autologous Chondrocyte graft in UK]
| |
| * [http://www.action.org.uk/touching_lives/pdfs/touching_lives.2003.autumn.pdf UK Health Charity covers Autologous Chondrocyte grafts]
| |
|
| |
|
| | {{Diseases of the musculoskeletal system and connective tissue}} |
|
| |
|
| {{SIB}}
| |
| {{Diseases of the musculoskeletal system and connective
| |
|
| |
| [[Category:Arthritis]]
| |
| [[Category:General practice]]
| |
| [[Category:Rheumatology]] | | [[Category:Rheumatology]] |
|
| |
|
| |
|
| [[bg:Артроза]] | | [[bg:Артроза]] |