Oritavancin: Difference between revisions
Gloria Picoy (talk | contribs) No edit summary |
Gloria Picoy (talk | contribs) No edit summary |
||
| Line 56: | Line 56: | ||
=====Development of Drug Resistant Bacteria===== | =====Development of Drug Resistant Bacteria===== | ||
Prescribing ORBACTIV in the absence of a proven or strongly suspected bacterial infection is unlikely to provide benefit to the patient and increases the risk of the development of drug-resistant bacteria. | Prescribing ORBACTIV in the absence of a proven or strongly suspected bacterial infection is unlikely to provide benefit to the patient and increases the risk of the development of drug-resistant bacteria. | ||
|clinicalTrials=Because clinical trials are conducted under widely varying conditions, adverse reaction rates observed in the clinical trials of ORBACTIV cannot be directly compared to rates in the clinical trials of another drug and may not reflect the rates observed in practice. | |||
ORBACTIV has been evaluated in two, double-blind, controlled ABSSSI clinical trials, which included 976 adult patients treated with a single 1200 mg intravenous dose of ORBACTIV and 983 patients treated with intravenous vancomycin for 7 to 10 days. The median age of patients treated with ORBACTIV was 45.6 years, ranging between 18 and 89 years of age with 8.8% ≥65 years of age. Patients treated with ORBACTIV were predominantly male (65.4%), 64.4% were Caucasian, 5.8% were African American, and 28.1% were Asian. Safety was evaluated for up to 60 days after dosing. | |||
In the pooled ABSSSI clinical trials, serious adverse reactions were reported in 57/976 (5.8%) patients treated with ORBACTIV and 58/983 (5.9%) treated with vancomycin. The most commonly reported serious adverse reaction was cellulitis in both treatment groups: 11/976 (1.1%) in ORBACTIV and 12/983 (1.2%) in the vancomycin arms, respectively. | |||
The most commonly reported adverse reactions (≥3%) in patients receiving a single 1200 mg dose of ORBACTIV in the pooled ABSSSI clinical trials were: headache, nausea, vomiting, limb and subcutaneous abscesses, and diarrhea. | |||
In the pooled ABSSSI clinical trials, ORBACTIV was discontinued due to adverse reactions in 36/976 (3.7%) of patients; the most common reported reactions leading to discontinuation were cellulitis (4/976, 0.4%) and osteomyelitis (3/976, 0.3%). | |||
TABLE 1 provides selected adverse reactions occurring in ≥ 1.5% of patients receiving ORBACTIV in the pooled ABSSSI clinical trials. There were 540 (55.3%) patients in the ORBACTIV arm and 559 (56.9%) patients in the vancomycin arm, who reported ≥1 adverse reaction. | |||
[[File:Oritavancin Adverse reactions.png|thumb|none|600px]] | |||
The following selected adverse reactions were reported in ORBACTIV-treated patients at a rate of less than 1.5%: | |||
* Blood and lymphatic system disorders: anemia, eosinophilia | |||
* General Disorders and administration site conditions: infusion site erythema, extravasation, induration, pruritis, rash, edema peripheral | |||
* Immune system disorders: hypersensitivity | |||
* Infections and infestations: osteomyelitis | |||
* Investigations: total bilirubin increased, hyperuricemia | |||
* Metabolism and nutrition disorders: hypoglycemia | |||
* Musculoskeletal and connective tissue disorders: tenosynovitis, myalgia | |||
* Respiratory, thoracic and mediastinal disorders: bronchospasm, wheezing | |||
* Skin and Subcutaneous Tissue Disorders: urticaria, angioedema, erythema multiforme, pruritis, leucocytoclastic vasculitis, rash. | |||
|drugInteractions======Effect of ORBACTIV on CYP Substrates===== | |drugInteractions======Effect of ORBACTIV on CYP Substrates===== | ||
A cocktail drug-drug interaction study was conducted in healthy volunteers (n=16) evaluating the concomitant administration of a single 1200 mg dose of ORBACTIV with probe substrates for several CYP450 enzymes. ORBACTIV was found to be a nonspecific, weak inhibitor (CYP2C9 and CYP2C19) or inducer (CYP3A4 and CYP2D6) of several CYP isoforms. | A cocktail drug-drug interaction study was conducted in healthy volunteers (n=16) evaluating the concomitant administration of a single 1200 mg dose of ORBACTIV with probe substrates for several CYP450 enzymes. ORBACTIV was found to be a nonspecific, weak inhibitor (CYP2C9 and CYP2C19) or inducer (CYP3A4 and CYP2D6) of several CYP isoforms. | ||
| Line 70: | Line 94: | ||
|useInPed=Safety and effectiveness of ORBACTIV in pediatric patients (younger than 18 years of age) has not been studied. | |useInPed=Safety and effectiveness of ORBACTIV in pediatric patients (younger than 18 years of age) has not been studied. | ||
|useInGeri=The pooled Phase 3 ABSSSI clinical trials of ORBACTIV did not include sufficient numbers of subjects aged 65 and older to determine whether they respond differently from younger subjects. Other reported clinical experience has not identified differences in responses between the elderly and younger patients, but greater sensitivity of some older individuals cannot be ruled out. | |useInGeri=The pooled Phase 3 ABSSSI clinical trials of ORBACTIV did not include sufficient numbers of subjects aged 65 and older to determine whether they respond differently from younger subjects. Other reported clinical experience has not identified differences in responses between the elderly and younger patients, but greater sensitivity of some older individuals cannot be ruled out. | ||
|useInGender=Population pharmacokinetic analysis from the Phase 3 ABSSSI trials in patients indicated that gender had no clinically relevant effect on the exposure of ORBACTIV. No dosage adjustment is warranted in these subpopulations. | |||
|useInRace=Population pharmacokinetic analysis from the Phase 3 ABSSSI trials in patients indicated that race had no clinically relevant effect on the exposure of ORBACTIV. No dosage adjustment is warranted in these subpopulations. | |||
|useInRenalImpair=No dosage adjustment of ORBACTIV is needed in patients with mild or moderate renal impairment. The pharmacokinetics of ORBACTIV in severe renal impairment have not been evaluated. ORBACTIV is not removed from blood by hemodialysis. | |useInRenalImpair=No dosage adjustment of ORBACTIV is needed in patients with mild or moderate renal impairment. The pharmacokinetics of ORBACTIV in severe renal impairment have not been evaluated. ORBACTIV is not removed from blood by hemodialysis. | ||
|useInHepaticImpair=No dosage adjustment of ORBACTIV is needed in patients with mild or moderate hepatic impairment. The pharmacokinetics of ORBACTIV in patients with severe hepatic insufficiency has not been studied. | |useInHepaticImpair=No dosage adjustment of ORBACTIV is needed in patients with mild or moderate hepatic impairment. The pharmacokinetics of ORBACTIV in patients with severe hepatic insufficiency has not been studied. | ||
|useInReproPotential=Oritavancin did not affect the fertility or reproductive performance of male rats (exposed to daily doses up to 30 mg/kg for at least 4 weeks) and female rats (exposed to daily doses up to 30 mg/kg for at least 2 weeks prior to mating). Those daily doses would be equivalent to a human dose of 300 mg, or 25% of clinical dose. Higher doses were not evaluated in nonclinical fertility studies. | |||
|administration=Intravenous | |administration=Intravenous | ||
|overdose=In the ORBACTIV clinical program there was no incidence of accidental overdose of ORBACTIV. | |overdose=In the ORBACTIV clinical program there was no incidence of accidental overdose of ORBACTIV. | ||
Based on an in vitro hemodialysis study, ORBACTIV is unlikely to be removed from blood by hemodialysis. In the event of overdose, supportive measures should be taken. | Based on an in vitro hemodialysis study, ORBACTIV is unlikely to be removed from blood by hemodialysis. In the event of overdose, supportive measures should be taken. | ||
|mechAction=Oritavancin has three mechanisms of action: (i) inhibition of the transglycosylation (polymerization) step of cell wall biosynthesis by binding to the stem peptide of peptidoglycan precursors; (ii) inhibition of the transpeptidation (crosslinking) step of cell wall biosynthesis by binding to the peptide bridging segments of the cell wall; and (iii) disruption of bacterial membrane integrity, leading to depolarization, permeabilization, and cell death. These multiple mechanisms contribute to the concentration-dependent bactericidal activity of oritavancin. | |||
|structure=The chemical structure is represented below: | |||
[[File:Oritavancin Chemical structure.png|thumb|none|500px]] | |||
|PD=The antimicrobial activity of oritavancin appears to correlate with the ratio of area under the concentration-time curve to minimal inhibitory concentration (AUC/MIC) based on animal models of infection. | |PD=The antimicrobial activity of oritavancin appears to correlate with the ratio of area under the concentration-time curve to minimal inhibitory concentration (AUC/MIC) based on animal models of infection. | ||
| Line 82: | Line 113: | ||
======Cardiac Electrophysiology====== | ======Cardiac Electrophysiology====== | ||
In a thorough QTc study of 135 healthy subjects at a dose 1.3 times the 1200 mg recommended dose, ORBACTIV did not prolong the QTc interval to any clinically relevant extent. | In a thorough QTc study of 135 healthy subjects at a dose 1.3 times the 1200 mg recommended dose, ORBACTIV did not prolong the QTc interval to any clinically relevant extent. | ||
|PK=The population PK analysis was derived using data from the two Phase 3 ABSSSI clinical trials in 297 patients. The mean pharmacokinetic parameters of oritavancin in patients following a single 1200 mg dose are presented in TABLE 2. | |||
[[File:Oritavancin Mean PK parameters.png|thumb|none|500px]] | |||
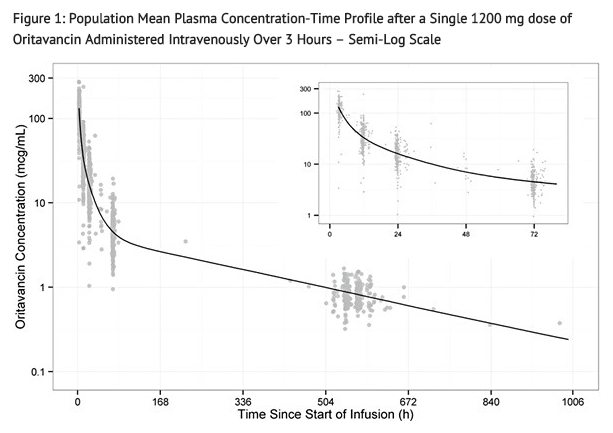
Oritavancin exhibits linear pharmacokinetics at a dose up to 1200 mg. The mean, population-predicted oritavancin concentration-time profile displays a multi-exponential decline with a long terminal plasma half-life as shown in FIGURE 1. | |||
[[File:Oritavancin Population Mean Plasma Concentration.png|thumb|none|500px]] | |||
======Distribution====== | |||
Oritavancin is approximately 85% bound to human plasma proteins. | |||
Based on population PK analysis, the population mean total volume of distribution is estimated to be approximately 87.6 L, indicating oritavancin is extensively distributed into the tissues. | |||
Exposures of oritavancin in skin blister fluid were approximately 20% of those in plasma (AUC0-24) after single 800 mg dose in healthy subjects. | |||
======Metabolism/Excretion====== | |||
Non-clinical studies including in vitro human liver microsome studies indicated that oritavancin is not metabolized. No mass balance study has been conducted in humans. In humans, oritavancin is slowly excreted unchanged in feces and urine with less than 1% and 5% of the dose recovered in feces and urine, respectively, after 2 weeks of collection. | |||
Oritavancin has a terminal half-life of approximately 245 hours and a clearance of 0.445 L/h based on population pharmacokinetic analyses. | |||
|nonClinToxic=======Mechanism of Resistance====== | |||
In serial passage studies, resistance to oritavancin was observed in isolates of S. aureus and E. faecalis. Resistance to oritavancin was not observed in clinical studies. | |||
======Interaction with Other Antimicrobial Agents====== | |||
In in vitro studies, oritavancin exhibits synergistic bactericidal activity in combination with gentamicin, moxifloxacin or rifampicin against isolates of methicillin-susceptible S. aureus (MSSA), with gentamicin or linezolid against isolates of heterogeneous vancomycin-intermediate S. aureus (hVISA), VISA, and vancomycin-resistant S. aureus (VRSA), and with rifampin against isolates of VRSA. In vitro studies demonstrated no antagonism between oritavancin and gentamicin, moxifloxacin, linezolid or rifampin. | |||
======Antibacterial Activity====== | |||
Oritavancin has been shown to be active against most isolates of the following bacteria, both in vitro and in clinical infections as described in the Indications and Usage section. | |||
* Staphylococcus aureus (including methicillin-resistant isolates) | |||
* Streptococcus agalactiae | |||
* Streptococcus anginosus group (includes S. anginosus, S. intermedius, and S. constellatus) | |||
* Streptococcus dysgalactiae | |||
* Streptococcus pyogenes | |||
* Enterococcus faecalis (vancomycin-susceptible isolates only) | |||
The following in vitro data are available but their clinical significance has not been established. At least 90% of isolates of the following microorganisms exhibit an in vitro minimum inhibitory concentration (MIC) less than or equal to 0.12 mcg/mL for oritavancin. However, the safety and effectiveness of oritavancin in treating clinical infections due to these bacteria have not been established in adequate and well-controlled clinical trials. | |||
* Enterococcus faecium (vancomycin-susceptible isolates only) | |||
======Carcinogenesis and Mutagenesis====== | |||
Long term studies in animals have not been conducted to determine the carcinogenic potential of oritavancin. | |||
No mutagenic or clastogenic potential of oritavancin was found in a battery of tests, including an Ames assay, in vitro chromosome aberration assay in Chinese hamster ovary cells, in vitro forward mutation assay in mouse lymphoma cells and an in vivo mouse micronucleus assay. | |||
|clinicalStudies======Acute Bacterial Skin and Skin Structure Infections (ABSSSI)===== | |||
A total of 1987 adults with clinically documented ABSSSI suspected or proven to be due to Gram-positive pathogens were randomized into two identically designed, randomized, double-blind, multi-center, multinational, non-inferiority trials (Trial 1 and Trial 2) comparing a single 1200 mg intravenous dose of ORBACTIV to intravenous vancomycin (1 g or 15 mg/kg every 12 hours) for 7 to 10 days. The primary analysis population (modified intent to treat, mITT) included all randomized patients who received any study drug. Patients could receive concomitant aztreonam or metronidazole for suspected Gram-negative and anaerobic infection, respectively. Patient demographic and baseline characteristics were balanced between treatment groups. Approximately 64% of patients were Caucasian and 65% were males. The mean age was 45 years and the mean body mass index was 27 kg/m2. Across both trials, approximately 60% of patients were enrolled from the United States and 27% of patients from Asia. A history of diabetes was present in 14% of patients. The types of ABSSSI across both trials included cellulitis/erysipelas (40%), wound infection (29%), and major cutaneous abscesses (31%). Median infection area at baseline across both trials was 266.6 cm2. | |||
The primary endpoint in both trials was early clinical response (responder), defined as cessation of spread or reduction in size of baseline lesion, absence of fever, and no rescue antibacterial drug at 48 to 72 hours after initiation of therapy. | |||
TABLE 5 provides the efficacy results for the primary endpoint in Trial 1 and Trial 2 in the primary analysis population. | |||
[[File:Oritavancin Clinical Response Rates in ABSSSI Trials using Responders at 48-72 Hours after Initiation of Therapy.png|thumb|none|500px]] | |||
A key secondary endpoint in these two ABSSSI trials evaluated the percentage of patients achieving a 20% or greater reduction in lesion area from baseline at 48-72 hours after initiation of therapy. TABLE 6 summarizes the findings for this endpoint in the two ABSSSI trials. | |||
[[File:Oritavancin Clinical Response Rates in ABSSSI Trials using Reduction in Lesion Area of 20% or Greater at 48-72 Hours after Initiation of Therapy.png|thumb|none|500px]] | |||
Another secondary efficacy endpoint in the two trials was investigator-assessed clinical success at post therapy evaluation at day 14 to 24 (7 to 14 days from end of blinded therapy). A patient was categorized as a clinical success if the patient experienced a complete or nearly complete resolution of baseline signs and symptoms related to primary ABSSSI site (erythema, induration/edema, purulent drainage, fluctuance, pain, tenderness, local increase in heat/warmth) such that no further treatment with antibacterial drugs was needed. | |||
TABLE 7 summarizes the findings for this endpoint in the mITT and clinically evaluable population in these two ABSSSI trials. Note that there are insufficient historical data to establish the magnitude of drug effect for antibacterial drugs compared with placebo at the post therapy visits. Therefore, comparisons of ORBACTIV to vancomycin based on clinical success rates at these visits cannot be utilized to establish non-inferiority conclusions. | |||
[[File:Oritavancin Clinical Success Rates in ABSSSI Trials at the Follow-Up Visit.png|thumb|none|500px]] | |||
Outcomes by Baseline Pathogen: TABLE 8 shows outcomes in patients with an identified baseline pathogen in the microbiological Intent-to-Treat (microITT) population in a pooled analysis of Trial 1 and Trial 2. The outcomes shown in the table are clinical response rates at 48 to 72 hours and clinical success rates at follow-up study day14 to 24. | |||
[[File:Oritavancin Outcomes by Baseline Pathogen.png|thumb|none|600px]] | |||
|howSupplied=* Single use 50 mL capacity glass vials containing sterile lyophilized powder equivalent to 400 mg of oritavancin (NDC 65293-015-01). | |||
|storage=Stored at 20°C to 25°C (68°F to 77°F) | |||
|packLabel=[[File:Oritavancin FDA package label.png|thumb|none|600px]] | |||
|fdaPatientInfo=Patients should be advised that allergic reactions, including serious allergic reactions, could occur and that serious reactions require immediate treatment. They should inform their healthcare provider about any previous hypersensitivity reactions to ORBACTIV, other glycopeptides (vancomycin, telavancin, or dalbavancin) or other allergens. | |||
Patients should be advised that diarrhea is a common problem caused by antibacterial drugs including ORBACTIV, which usually resolves when the drug is discontinued. Sometimes, frequent watery or bloody diarrhea may occur and may be a sign of a more serious intestinal infection. If severe watery or bloody diarrhea develops, patients should contact their healthcare provider. | |||
|alcohol=Alcohol-Oritavancin interaction has not been established. Talk to your doctor about the effects of taking alcohol with this medication. | |alcohol=Alcohol-Oritavancin interaction has not been established. Talk to your doctor about the effects of taking alcohol with this medication. | ||
|brandNames=* Orbactiv | |brandNames=* Orbactiv | ||
}} | }} | ||
} | |||
{{drugbox | | {{drugbox | | ||
| IUPAC_name = | | IUPAC_name = | ||
Revision as of 17:32, 10 February 2015
Editor-In-Chief: C. Michael Gibson, M.S., M.D. [1]; Associate Editor(s)-in-Chief: Gloria Picoy [2]
Disclaimer
WikiDoc MAKES NO GUARANTEE OF VALIDITY. WikiDoc is not a professional health care provider, nor is it a suitable replacement for a licensed healthcare provider. WikiDoc is intended to be an educational tool, not a tool for any form of healthcare delivery. The educational content on WikiDoc drug pages is based upon the FDA package insert, National Library of Medicine content and practice guidelines / consensus statements. WikiDoc does not promote the administration of any medication or device that is not consistent with its labeling. Please read our full disclaimer here.
Overview
Oritavancin is an antibiotic that is FDA approved for the treatment of acute bacterial skin and skin structure infections caused by Gram-positive microorganisms. Common adverse reactions include nausea, vomiting and headache
limb and subcutaneous abscesses, and diarrhea.
Adult Indications and Dosage
FDA-Labeled Indications and Dosage (Adult)
Acute Bacterial Skin and Skin Structure Infections
- Oritavancin is indicated for the treatment of adult patients with acute bacterial skin and skin structure infections (ABSSSI) caused by susceptible isolates of the following Gram-positive microorganisms:
- Staphylococcus aureus (including methicillin-susceptible and methicillin–resistant isolates), Streptococcus pyogenes, Streptococcus agalactiae, Streptococcus dysgalactiae, Streptococcus anginosus group (includes S. anginosus, S. intermedius, and S. constellatus), and Enterococcus faecalis (vancomycin-susceptible isolates only).
- Dosage: a single 1200 mg dose administered by intravenous infusion over 3 hours
Off-Label Use and Dosage (Adult)
Guideline-Supported Use
There is limited information regarding Off-Label Guideline-Supported Use of Oritavancin in adult patients.
Non–Guideline-Supported Use
There is limited information regarding Off-Label Non–Guideline-Supported Use of Oritavancin in adult patients.
Pediatric Indications and Dosage
FDA-Labeled Indications and Dosage (Pediatric)
Safety and efficacy are not established in pediatric patients
Off-Label Use and Dosage (Pediatric)
Guideline-Supported Use
There is limited information regarding Off-Label Guideline-Supported Use of Oritavancin in pediatric patients.
Non–Guideline-Supported Use
There is limited information regarding Off-Label Non–Guideline-Supported Use of Oritavancin in pediatric patients.
Contraindications
Intravenous Unfractionated Heparin Sodium
Use of intravenous unfractionated heparin sodium is contraindicated for 48 hours after ORBACTIV administration because the activated partial thromboplastin time (aPTT) test results are expected to remain falsely elevated for approximately 48 hours after ORBACTIV administration.
Hypersensitivity
ORBACTIV is contraindicated in patients with known hypersensitivity to ORBACTIV.
Warnings
Potential Risk of Bleeding with Concomitant Use of Warfarin
Co-administration of ORBACTIV and warfarin may result in higher exposure of warfarin, which may increase the risk of bleeding. Use ORBACTIV in patients on chronic warfarin therapy only when the benefits can be expected to outweigh the risk of bleeding. Frequently monitor for signs of bleeding.
ORBACTIV has been shown to artificially prolong PT and INR for up to 24 hours, making the monitoring of the anticoagulation effect of warfarin unreliable up to 24 hours after an ORBACTIV dose.
Coagulation Test Interference
ORBACTIV has been shown to artificially prolong aPTT for 48 hours and the PT and INR for 24 hours by binding to and preventing action of the phospholipid reagents which activate coagulation in commonly used laboratory coagulation tests.
For patients who require aPTT monitoring within 48 hours of ORBACTIV dosing, a non-phospholipid dependent coagulation test such as a Factor Xa (chromogenic) assay or an alternative anticoagulant not requiring aPTT monitoring may be considered.
Effects by ORBACTIV on activated clotting time (ACT) are expected since the phospholipid reagents are also utilized in this coagulation test. ORBACTIV has no effect on the coagulation system.
Hypersensitivity
Serious hypersensitivity reactions have been reported with the use of ORBACTIV. If an acute hypersensitivity reaction occurs during ORBACTIV infusion, discontinue ORBACTIV immediately and institute appropriate supportive care. Before using ORBACTIV, inquire carefully about previous hypersensitivity reactions to glycopeptides. Due to the possibility of cross-sensitivity, carefully monitor for signs of hypersensitivity during ORBACTIV infusion in patients with a history of glycopeptide allergy. In the Phase 3 ABSSSI clinical trials, the median onset of hypersensitivity reactions in ORBACTIV-treated patients was 1.2 days and the median duration of these reactions was 2.4 days.
Infusion Related Reactions
Infusion related reactions have been reported with ORBACTIV including pruritus, urticaria or flushing. If reactions do occur, consider slowing or interrupting ORBACTIV infusion.
Clostridium difficile-associated Diarrhea
Clostridium difficile-associated diarrhea (CDAD) has been reported for nearly all systemic antibacterial drugs, including ORBACTIV, and may range in severity from mild diarrhea to fatal colitis. Treatment with antibacterial agents alters the normal flora of the colon and may permit overgrowth of C. difficile.
C. difficile produces toxins A and B which contribute to the development of CDAD. Hypertoxin-producing strains of C. difficile cause increased morbidity and mortality, as these infections can be refractory to antibacterial therapy and may require colectomy. CDAD must be considered in all patients who present with diarrhea following antibacterial use. Careful medical history is necessary because CDAD has been reported to occur more than 2 months after the administration of antibacterial agents.
If CDAD is suspected or confirmed, antibacterial use not directed against C. difficile may need to be discontinued. Appropriate fluid and electrolyte management, protein supplementation, antibacterial treatment of C. difficile, and surgical evaluation should be instituted as clinically indicated.
Osteomyelitis
In Phase 3 ABSSSI clinical trials, more cases of osteomyelitis were reported in the ORBACTIV treated arm than in the vancomycin-treated arm. Monitor patients for signs and symptoms of osteomyelitis. If osteomyelitis is suspected or diagnosed, institute appropriate alternate antibacterial therapy}.
Development of Drug Resistant Bacteria
Prescribing ORBACTIV in the absence of a proven or strongly suspected bacterial infection is unlikely to provide benefit to the patient and increases the risk of the development of drug-resistant bacteria.
Adverse Reactions
Clinical Trials Experience
Because clinical trials are conducted under widely varying conditions, adverse reaction rates observed in the clinical trials of ORBACTIV cannot be directly compared to rates in the clinical trials of another drug and may not reflect the rates observed in practice.
ORBACTIV has been evaluated in two, double-blind, controlled ABSSSI clinical trials, which included 976 adult patients treated with a single 1200 mg intravenous dose of ORBACTIV and 983 patients treated with intravenous vancomycin for 7 to 10 days. The median age of patients treated with ORBACTIV was 45.6 years, ranging between 18 and 89 years of age with 8.8% ≥65 years of age. Patients treated with ORBACTIV were predominantly male (65.4%), 64.4% were Caucasian, 5.8% were African American, and 28.1% were Asian. Safety was evaluated for up to 60 days after dosing.
In the pooled ABSSSI clinical trials, serious adverse reactions were reported in 57/976 (5.8%) patients treated with ORBACTIV and 58/983 (5.9%) treated with vancomycin. The most commonly reported serious adverse reaction was cellulitis in both treatment groups: 11/976 (1.1%) in ORBACTIV and 12/983 (1.2%) in the vancomycin arms, respectively.
The most commonly reported adverse reactions (≥3%) in patients receiving a single 1200 mg dose of ORBACTIV in the pooled ABSSSI clinical trials were: headache, nausea, vomiting, limb and subcutaneous abscesses, and diarrhea.
In the pooled ABSSSI clinical trials, ORBACTIV was discontinued due to adverse reactions in 36/976 (3.7%) of patients; the most common reported reactions leading to discontinuation were cellulitis (4/976, 0.4%) and osteomyelitis (3/976, 0.3%).
TABLE 1 provides selected adverse reactions occurring in ≥ 1.5% of patients receiving ORBACTIV in the pooled ABSSSI clinical trials. There were 540 (55.3%) patients in the ORBACTIV arm and 559 (56.9%) patients in the vancomycin arm, who reported ≥1 adverse reaction.

The following selected adverse reactions were reported in ORBACTIV-treated patients at a rate of less than 1.5%:
- Blood and lymphatic system disorders: anemia, eosinophilia
- General Disorders and administration site conditions: infusion site erythema, extravasation, induration, pruritis, rash, edema peripheral
- Immune system disorders: hypersensitivity
- Infections and infestations: osteomyelitis
- Investigations: total bilirubin increased, hyperuricemia
- Metabolism and nutrition disorders: hypoglycemia
- Musculoskeletal and connective tissue disorders: tenosynovitis, myalgia
- Respiratory, thoracic and mediastinal disorders: bronchospasm, wheezing
- Skin and Subcutaneous Tissue Disorders: urticaria, angioedema, erythema multiforme, pruritis, leucocytoclastic vasculitis, rash.
Postmarketing Experience
There is limited information regarding Oritavancin Postmarketing Experience in the drug label.
Drug Interactions
Effect of ORBACTIV on CYP Substrates
A cocktail drug-drug interaction study was conducted in healthy volunteers (n=16) evaluating the concomitant administration of a single 1200 mg dose of ORBACTIV with probe substrates for several CYP450 enzymes. ORBACTIV was found to be a nonspecific, weak inhibitor (CYP2C9 and CYP2C19) or inducer (CYP3A4 and CYP2D6) of several CYP isoforms.
Caution should be used when administering ORBACTIV concomitantly with drugs with a narrow therapeutic window that are predominantly metabolized by one of the affected CYP450 enzymes (e.g., warfarin), as co-administration may increase (e.g. for CYP2C9 substrates) or decrease (e.g. for CYP2D6 substrates) concentrations of the narrow therapeutic range drug. Patients should be closely monitored for signs of toxicity or lack of efficacy if they have been given ORBACTIV while on a potentially affected compound (e.g. patients should be monitored for bleeding if concomitantly receiving ORBACTIV and warfarin).
Drug-Laboratory Test Interactions
ORBACTIV has been shown to artificially prolong aPTT for 48 hours and PT and INR for up to 24 hours by binding to and preventing action of the phospholipid reagents which activate coagulation in commonly used laboratory coagulation tests. Effects by ORBACTIV on ACT are expected since the phospholipid reagents are also utilized in this coagulation test. ORBACTIV has no effect on the coagulation system.
Use in Specific Populations
Pregnancy
Pregnancy Category (FDA): C Reproduction studies performed in rats and rabbits have revealed no evidence of harm to the fetus due to oritavancin at the highest concentrations administered, 30 mg/kg/day and 15 mg/kg/day, respectively. Those daily doses would be equivalent to a human dose of 300 mg, or 25% of the single clinical dose of 1200 mg. Higher doses were not evaluated in nonclinical developmental and reproductive toxicology studies.
There are no adequate and well-controlled trials in pregnant women. ORBACTIV should be used during pregnancy only if the potential benefit justifies the potential risk to the fetus.
Pregnancy Category (AUS):
There is no Australian Drug Evaluation Committee (ADEC) guidance on usage of Oritavancin in women who are pregnant.
Labor and Delivery
There is no FDA guidance on use of Oritavancin during labor and delivery.
Nursing Mothers
It is unknown whether oritavancin is excreted in human milk. Following a single intravenous infusion in lactating rats, radio-labeled [14C]-oritavancin was excreted in milk and absorbed by nursing pups. Caution should be exercised when ORBACTIV is administered to a nursing woman.
Pediatric Use
Safety and effectiveness of ORBACTIV in pediatric patients (younger than 18 years of age) has not been studied.
Geriatic Use
The pooled Phase 3 ABSSSI clinical trials of ORBACTIV did not include sufficient numbers of subjects aged 65 and older to determine whether they respond differently from younger subjects. Other reported clinical experience has not identified differences in responses between the elderly and younger patients, but greater sensitivity of some older individuals cannot be ruled out.
Gender
Population pharmacokinetic analysis from the Phase 3 ABSSSI trials in patients indicated that gender had no clinically relevant effect on the exposure of ORBACTIV. No dosage adjustment is warranted in these subpopulations.
Race
Population pharmacokinetic analysis from the Phase 3 ABSSSI trials in patients indicated that race had no clinically relevant effect on the exposure of ORBACTIV. No dosage adjustment is warranted in these subpopulations.
Renal Impairment
No dosage adjustment of ORBACTIV is needed in patients with mild or moderate renal impairment. The pharmacokinetics of ORBACTIV in severe renal impairment have not been evaluated. ORBACTIV is not removed from blood by hemodialysis.
Hepatic Impairment
No dosage adjustment of ORBACTIV is needed in patients with mild or moderate hepatic impairment. The pharmacokinetics of ORBACTIV in patients with severe hepatic insufficiency has not been studied.
Females of Reproductive Potential and Males
Oritavancin did not affect the fertility or reproductive performance of male rats (exposed to daily doses up to 30 mg/kg for at least 4 weeks) and female rats (exposed to daily doses up to 30 mg/kg for at least 2 weeks prior to mating). Those daily doses would be equivalent to a human dose of 300 mg, or 25% of clinical dose. Higher doses were not evaluated in nonclinical fertility studies.
Immunocompromised Patients
There is no FDA guidance one the use of Oritavancin in patients who are immunocompromised.
Administration and Monitoring
Administration
Intravenous
Monitoring
There is limited information regarding Oritavancin Monitoring in the drug label.
IV Compatibility
There is limited information regarding the compatibility of Oritavancin and IV administrations.
Overdosage
In the ORBACTIV clinical program there was no incidence of accidental overdose of ORBACTIV.
Based on an in vitro hemodialysis study, ORBACTIV is unlikely to be removed from blood by hemodialysis. In the event of overdose, supportive measures should be taken.
Pharmacology
There is limited information regarding Oritavancin Pharmacology in the drug label.
Mechanism of Action
Oritavancin has three mechanisms of action: (i) inhibition of the transglycosylation (polymerization) step of cell wall biosynthesis by binding to the stem peptide of peptidoglycan precursors; (ii) inhibition of the transpeptidation (crosslinking) step of cell wall biosynthesis by binding to the peptide bridging segments of the cell wall; and (iii) disruption of bacterial membrane integrity, leading to depolarization, permeabilization, and cell death. These multiple mechanisms contribute to the concentration-dependent bactericidal activity of oritavancin.
Structure
The chemical structure is represented below:

Pharmacodynamics
The antimicrobial activity of oritavancin appears to correlate with the ratio of area under the concentration-time curve to minimal inhibitory concentration (AUC/MIC) based on animal models of infection.
Exposure-response analyses from both preclinical and clinical studies support the treatment of clinically relevant Gram-positive microorganisms (e.g. S. aureus and S. pyogenes) causative of ABSSSI with a single 1200 mg dose of ORBACTIV.
Cardiac Electrophysiology
In a thorough QTc study of 135 healthy subjects at a dose 1.3 times the 1200 mg recommended dose, ORBACTIV did not prolong the QTc interval to any clinically relevant extent.
Pharmacokinetics
The population PK analysis was derived using data from the two Phase 3 ABSSSI clinical trials in 297 patients. The mean pharmacokinetic parameters of oritavancin in patients following a single 1200 mg dose are presented in TABLE 2.

Oritavancin exhibits linear pharmacokinetics at a dose up to 1200 mg. The mean, population-predicted oritavancin concentration-time profile displays a multi-exponential decline with a long terminal plasma half-life as shown in FIGURE 1.
Distribution
Oritavancin is approximately 85% bound to human plasma proteins.
Based on population PK analysis, the population mean total volume of distribution is estimated to be approximately 87.6 L, indicating oritavancin is extensively distributed into the tissues.
Exposures of oritavancin in skin blister fluid were approximately 20% of those in plasma (AUC0-24) after single 800 mg dose in healthy subjects.
Metabolism/Excretion
Non-clinical studies including in vitro human liver microsome studies indicated that oritavancin is not metabolized. No mass balance study has been conducted in humans. In humans, oritavancin is slowly excreted unchanged in feces and urine with less than 1% and 5% of the dose recovered in feces and urine, respectively, after 2 weeks of collection.
Oritavancin has a terminal half-life of approximately 245 hours and a clearance of 0.445 L/h based on population pharmacokinetic analyses.
Nonclinical Toxicology
Mechanism of Resistance
In serial passage studies, resistance to oritavancin was observed in isolates of S. aureus and E. faecalis. Resistance to oritavancin was not observed in clinical studies.
Interaction with Other Antimicrobial Agents
In in vitro studies, oritavancin exhibits synergistic bactericidal activity in combination with gentamicin, moxifloxacin or rifampicin against isolates of methicillin-susceptible S. aureus (MSSA), with gentamicin or linezolid against isolates of heterogeneous vancomycin-intermediate S. aureus (hVISA), VISA, and vancomycin-resistant S. aureus (VRSA), and with rifampin against isolates of VRSA. In vitro studies demonstrated no antagonism between oritavancin and gentamicin, moxifloxacin, linezolid or rifampin.
Antibacterial Activity
Oritavancin has been shown to be active against most isolates of the following bacteria, both in vitro and in clinical infections as described in the Indications and Usage section.
- Staphylococcus aureus (including methicillin-resistant isolates)
- Streptococcus agalactiae
- Streptococcus anginosus group (includes S. anginosus, S. intermedius, and S. constellatus)
- Streptococcus dysgalactiae
- Streptococcus pyogenes
- Enterococcus faecalis (vancomycin-susceptible isolates only)
The following in vitro data are available but their clinical significance has not been established. At least 90% of isolates of the following microorganisms exhibit an in vitro minimum inhibitory concentration (MIC) less than or equal to 0.12 mcg/mL for oritavancin. However, the safety and effectiveness of oritavancin in treating clinical infections due to these bacteria have not been established in adequate and well-controlled clinical trials.
- Enterococcus faecium (vancomycin-susceptible isolates only)
Carcinogenesis and Mutagenesis
Long term studies in animals have not been conducted to determine the carcinogenic potential of oritavancin.
No mutagenic or clastogenic potential of oritavancin was found in a battery of tests, including an Ames assay, in vitro chromosome aberration assay in Chinese hamster ovary cells, in vitro forward mutation assay in mouse lymphoma cells and an in vivo mouse micronucleus assay.
Clinical Studies
Acute Bacterial Skin and Skin Structure Infections (ABSSSI)
A total of 1987 adults with clinically documented ABSSSI suspected or proven to be due to Gram-positive pathogens were randomized into two identically designed, randomized, double-blind, multi-center, multinational, non-inferiority trials (Trial 1 and Trial 2) comparing a single 1200 mg intravenous dose of ORBACTIV to intravenous vancomycin (1 g or 15 mg/kg every 12 hours) for 7 to 10 days. The primary analysis population (modified intent to treat, mITT) included all randomized patients who received any study drug. Patients could receive concomitant aztreonam or metronidazole for suspected Gram-negative and anaerobic infection, respectively. Patient demographic and baseline characteristics were balanced between treatment groups. Approximately 64% of patients were Caucasian and 65% were males. The mean age was 45 years and the mean body mass index was 27 kg/m2. Across both trials, approximately 60% of patients were enrolled from the United States and 27% of patients from Asia. A history of diabetes was present in 14% of patients. The types of ABSSSI across both trials included cellulitis/erysipelas (40%), wound infection (29%), and major cutaneous abscesses (31%). Median infection area at baseline across both trials was 266.6 cm2.
The primary endpoint in both trials was early clinical response (responder), defined as cessation of spread or reduction in size of baseline lesion, absence of fever, and no rescue antibacterial drug at 48 to 72 hours after initiation of therapy.
TABLE 5 provides the efficacy results for the primary endpoint in Trial 1 and Trial 2 in the primary analysis population.

A key secondary endpoint in these two ABSSSI trials evaluated the percentage of patients achieving a 20% or greater reduction in lesion area from baseline at 48-72 hours after initiation of therapy. TABLE 6 summarizes the findings for this endpoint in the two ABSSSI trials.

Another secondary efficacy endpoint in the two trials was investigator-assessed clinical success at post therapy evaluation at day 14 to 24 (7 to 14 days from end of blinded therapy). A patient was categorized as a clinical success if the patient experienced a complete or nearly complete resolution of baseline signs and symptoms related to primary ABSSSI site (erythema, induration/edema, purulent drainage, fluctuance, pain, tenderness, local increase in heat/warmth) such that no further treatment with antibacterial drugs was needed.
TABLE 7 summarizes the findings for this endpoint in the mITT and clinically evaluable population in these two ABSSSI trials. Note that there are insufficient historical data to establish the magnitude of drug effect for antibacterial drugs compared with placebo at the post therapy visits. Therefore, comparisons of ORBACTIV to vancomycin based on clinical success rates at these visits cannot be utilized to establish non-inferiority conclusions.

Outcomes by Baseline Pathogen: TABLE 8 shows outcomes in patients with an identified baseline pathogen in the microbiological Intent-to-Treat (microITT) population in a pooled analysis of Trial 1 and Trial 2. The outcomes shown in the table are clinical response rates at 48 to 72 hours and clinical success rates at follow-up study day14 to 24.

How Supplied
- Single use 50 mL capacity glass vials containing sterile lyophilized powder equivalent to 400 mg of oritavancin (NDC 65293-015-01).
Storage
Stored at 20°C to 25°C (68°F to 77°F)
Images
Drug Images
{{#ask: Page Name::Oritavancin |?Pill Name |?Drug Name |?Pill Ingred |?Pill Imprint |?Pill Dosage |?Pill Color |?Pill Shape |?Pill Size (mm) |?Pill Scoring |?NDC |?Drug Author |format=template |template=DrugPageImages |mainlabel=- |sort=Pill Name }}
Package and Label Display Panel

{{#ask: Label Page::Oritavancin |?Label Name |format=template |template=DrugLabelImages |mainlabel=- |sort=Label Page }}
Patient Counseling Information
Patients should be advised that allergic reactions, including serious allergic reactions, could occur and that serious reactions require immediate treatment. They should inform their healthcare provider about any previous hypersensitivity reactions to ORBACTIV, other glycopeptides (vancomycin, telavancin, or dalbavancin) or other allergens.
Patients should be advised that diarrhea is a common problem caused by antibacterial drugs including ORBACTIV, which usually resolves when the drug is discontinued. Sometimes, frequent watery or bloody diarrhea may occur and may be a sign of a more serious intestinal infection. If severe watery or bloody diarrhea develops, patients should contact their healthcare provider.
Precautions with Alcohol
Alcohol-Oritavancin interaction has not been established. Talk to your doctor about the effects of taking alcohol with this medication.
Brand Names
- Orbactiv
Look-Alike Drug Names
There is limited information regarding Oritavancin Look-Alike Drug Names in the drug label.
Drug Shortage Status
Price
References
The contents of this FDA label are provided by the National Library of Medicine.
}
| File:Oritavancin.svg | |
| Identifiers | |
|---|---|
| CAS Number | |
| E number | {{#property:P628}} |
| ECHA InfoCard | {{#property:P2566}}Lua error in Module:EditAtWikidata at line 36: attempt to index field 'wikibase' (a nil value). |
| Chemical and physical data | |
| Formula | C86H97Cl3N10O26 |
| Molar mass | 1793.1 g/mol |
|
WikiDoc Resources for Oritavancin |
|
Articles |
|---|
|
Most recent articles on Oritavancin Most cited articles on Oritavancin |
|
Media |
|
Powerpoint slides on Oritavancin |
|
Evidence Based Medicine |
|
Clinical Trials |
|
Ongoing Trials on Oritavancin at Clinical Trials.gov Clinical Trials on Oritavancin at Google
|
|
Guidelines / Policies / Govt |
|
US National Guidelines Clearinghouse on Oritavancin
|
|
Books |
|
News |
|
Commentary |
|
Definitions |
|
Patient Resources / Community |
|
Patient resources on Oritavancin Discussion groups on Oritavancin Patient Handouts on Oritavancin Directions to Hospitals Treating Oritavancin Risk calculators and risk factors for Oritavancin
|
|
Healthcare Provider Resources |
|
Causes & Risk Factors for Oritavancin |
|
Continuing Medical Education (CME) |
|
International |
|
|
|
Business |
|
Experimental / Informatics |
Oritavancin (INN, also known as LY333328) is an investigational glycopeptide antibiotic with bactericidal activity effective in treating infections caused by Gram-positive organisms. It treats complicated skin and skin structure infections. This new drug will be tested for treatment of bacteraemia and nosocomial pneumonia.
It demonstrates similar activity to vancomycin, but it has stronger activity against Staphylococcus and Enterococcus. The pharmacokinetics and pharmacodynamics of oritavancin appear to be favourable and once-daily dosing is likely. The incidence of multi-drug resistant bacteria is increasing and explorations into additional treatment options are essential. The clinical efficacy of oritavancin has not yet been determined.
References
- Ward K, Mersfelder T, LaPlante K (2006). "Oritavancin--an investigational glycopeptide antibiotic". Expert Opin Investig Drugs. 15 (4): 417&ndash, 29. PMID 16548791.
- Pages with script errors
- Pages with broken file links
- E number from Wikidata
- ECHA InfoCard ID from Wikidata
- Chemical articles with unknown parameter in Infobox drug
- Articles without EBI source
- Chemical pages without ChemSpiderID
- Chemical pages without DrugBank identifier
- Articles without KEGG source
- Articles without InChI source
- Articles without UNII source
- Drugs missing an ATC code
- Drugs with no legal status
- Articles containing unverified chemical infoboxes
- CS1 maint: Multiple names: authors list
- Glycopeptide antibiotics