Non-bacterial thrombotic endocarditis echocardiography and ultrasound
|
non-bacterial thrombotic endocarditis |
|
Differentiating non-bacterial thrombotic endocarditis from other Diseases |
|---|
|
Diagnosis |
|
Treatment |
|
Case Studies |
|
Non-bacterial thrombotic endocarditis echocardiography and ultrasound On the Web |
|
American Roentgen Ray Society Images of Non-bacterial thrombotic endocarditis echocardiography and ultrasound |
|
FDA on Non-bacterial thrombotic endocarditis echocardiography and ultrasound |
|
CDC on Non-bacterial thrombotic endocarditis echocardiography and ultrasound |
|
Non-bacterial thrombotic endocarditis echocardiography and ultrasound in the news |
|
Blogs on Non-bacterial thrombotic endocarditis echocardiography and ultrasound |
Editor-In-Chief: C. Michael Gibson, M.S., M.D. [1]; Associate Editor(s)-in-Chief: Aisha Adigun, B.Sc., M.D.[2]
Overview
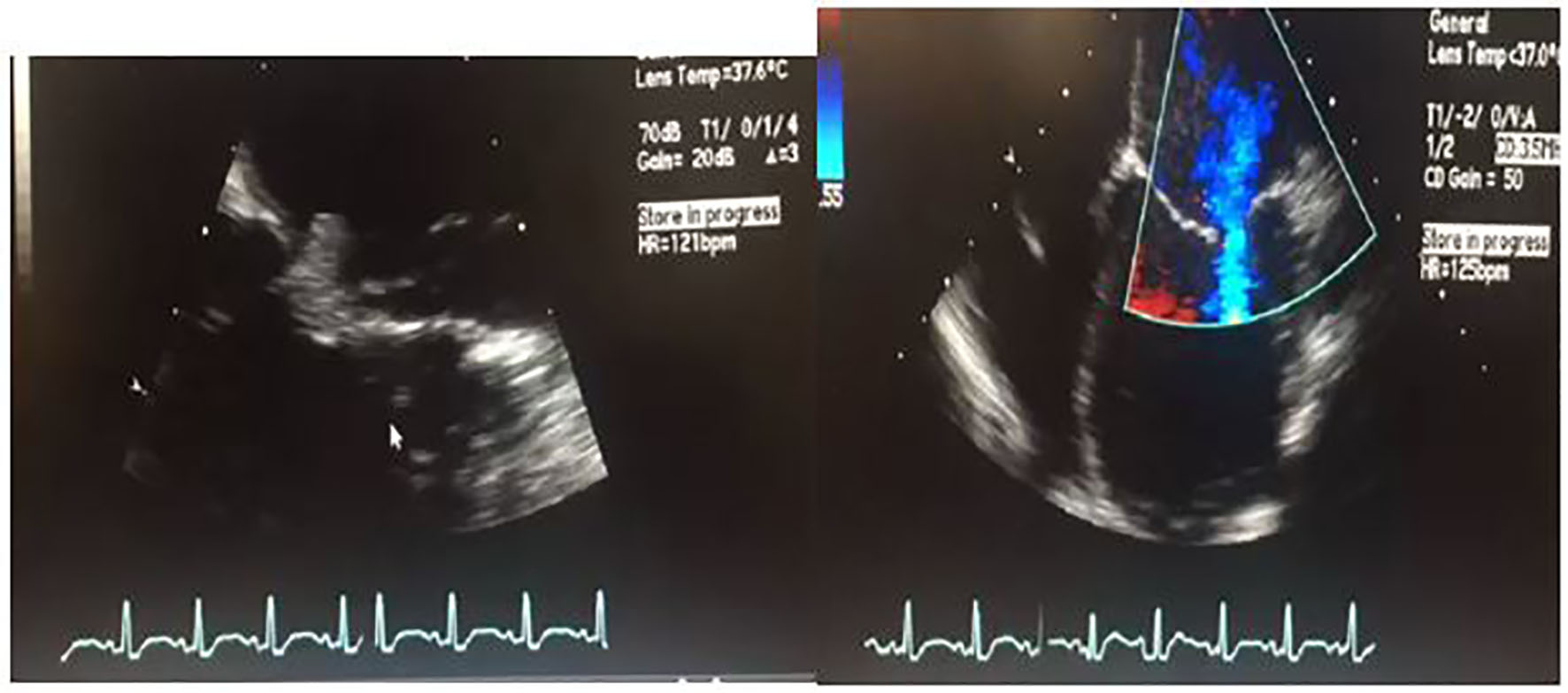
Echocardiography may be helpful in the diagnosis of non-bacterial thrombotic endocarditis. It is especially important in visualizing valvular vegetations suggestive of NBTE. Although echocardiography is important in the diagnosis of vegetations in cardiac valves, it does not differentiate vegetations due to thrombotic infection from vegetations as a result of aggregations of platelets and fibrin.
Echocardiography/Ultrasound
- Echocardiography may be helpful in the diagnosis of non-bacterial thrombotic endocarditis[1]. It is especially important in visualizing valvular vegetations suggestive of NBTE[2].
- Left sided valves are more commonly affected with 75% of cases seen in the mitral valve[3].
- The vegetations in NBTE are typically <1cm, broad-based, and irregularly shaped[4].
- Less commonly, vegetations have been found to involve all the cardiac valves[5][6].
- Transesophageal echocardiography is more sensitive (90%) than transthoracic echocardiography, especially for vegetations <5mm[7].
- Because transesophageal echocardiography is an invasive procedure, evaluation of patients with this modality should be cased-based.
- The two-dimensional transesophageal echocardiography (2D-TEE) has a higher diagnostic value for the detection of vegetations in NBTE, however, the three-dimensional TEE (3D-TEE) has the following benefits over it:
- Improved detection
- Improved characterization
- Improved clinical correlations of NBTE vegetations
- Provides clinically relevant additive information complementing the 2D-TEE for the characterization, detection, and association with the cerebrovascular disease of NBTE endocarditis.
- Although echocardiography is important in the diagnosis of vegetations in cardiac valves, it does not differentiate vegetations due to thrombotic infection from vegetations as a result of aggregations of platelets and fibrin.
References
- ↑ Roldan CA, Shively BK, Crawford MH (November 1996). "An echocardiographic study of valvular heart disease associated with systemic lupus erythematosus". N. Engl. J. Med. 335 (19): 1424–30. doi:10.1056/NEJM199611073351903. PMID 8875919.
- ↑ Roldan CA, Qualls CR, Sopko KS, Sibbitt WL (February 2008). "Transthoracic versus transesophageal echocardiography for detection of Libman-Sacks endocarditis: a randomized controlled study". J. Rheumatol. 35 (2): 224–9. PMID 18085739.
- ↑ "Non-bacterial Thrombotic Endocarditis | IntechOpen".
- ↑ Otto C.M.. Nonbacterial thrombotic endocarditis. Valvular heart disease, 1999 pp. 445–50
- ↑ Biller J, Challa VR, Toole JF, Howard VJ (February 1982). "Nonbacterial thrombotic endocarditis. A neurologic perspective of clinicopathologic correlations of 99 patients". Arch. Neurol. 39 (2): 95–8. doi:10.1001/archneur.1982.00510140029007. PMID 7059307.
- ↑ Reagan TJ, Okazaki H (December 1974). "The thrombotic syndrome associated with carcinoma. A clinical and neuropathologic study". Arch. Neurol. 31 (6): 390–5. doi:10.1001/archneur.1974.00490420056006. PMID 4374176.
- ↑ de Bruijn SF, Agema WR, Lammers GJ, van der Wall EE, Wolterbeek R, Holman ER, Bollen EL, Bax JJ (October 2006). "Transesophageal echocardiography is superior to transthoracic echocardiography in management of patients of any age with transient ischemic attack or stroke". Stroke. 37 (10): 2531–4. doi:10.1161/01.STR.0000241064.46659.69. PMID 16946152.