Myxoma chest x ray: Difference between revisions
No edit summary |
|||
| Line 37: | Line 37: | ||
*Tumor mobility and distensibility. | *Tumor mobility and distensibility. | ||
| style="padding: 5px 5px; background: #F5F5F5;" align=center| | | style="padding: 5px 5px; background: #F5F5F5;" align=center| | ||
*Limited views of the mediastinum and cannot be used to evaluate extracardiac manifestations of disease.<ref name="pmid1943240">{{cite journal |vauthors=Reeder GS, Khandheria BK, Seward JB, Tajik AJ |title=Transesophageal echocardiography and cardiac masses |journal=Mayo Clin. Proc. |volume=66 |issue=11 |pages=1101–9 |year=1991 |pmid=1943240 |doi= |url=}}</ref> | *Limited views of the [[mediastinum]] and cannot be used to evaluate extracardiac manifestations of disease.<ref name="pmid1943240">{{cite journal |vauthors=Reeder GS, Khandheria BK, Seward JB, Tajik AJ |title=Transesophageal echocardiography and cardiac masses |journal=Mayo Clin. Proc. |volume=66 |issue=11 |pages=1101–9 |year=1991 |pmid=1943240 |doi= |url=}}</ref> | ||
*TEE is an invasive imaging technique. | *[[Transesophageal echocardiography (TEE)|TEE]] is an invasive imaging technique. | ||
* | *[[TTE]] is limited by the imaging window, which can vary with the patient and operator experience. | ||
|- | |- | ||
| style="padding: 5px 5px; background: #DCDCDC;" align=center|'''MRI''' | | style="padding: 5px 5px; background: #DCDCDC;" align=center|'''MRI''' | ||
| Line 52: | Line 52: | ||
* Provides some functional information such as, flow direction and flow velocity in large vessels. | * Provides some functional information such as, flow direction and flow velocity in large vessels. | ||
| style="padding: 5px 5px; background: #F5F5F5;" align=center| | | style="padding: 5px 5px; background: #F5F5F5;" align=center| | ||
*Cannot show calcification. | *Cannot show [[calcification]]. | ||
*High susceptibility to motion artifact. | *High susceptibility to motion [[artifact]]. | ||
*Dependent on regular electrocardiographic rhythms and cardiac gating. | *Dependent on regular electrocardiographic rhythms and cardiac gating. | ||
|- | |- | ||
| Line 62: | Line 62: | ||
*Intracardiac heterogeneously low attenuating mass. | *Intracardiac heterogeneously low attenuating mass. | ||
*The attenuation is usually lower than that of myocardium. | *The attenuation is usually lower than that of myocardium. | ||
*Calcification is common | *[[Calcification]] is common | ||
| style="padding: 5px 5px; background: #F5F5F5;" align=center| | | style="padding: 5px 5px; background: #F5F5F5;" align=center| | ||
*CT provides better soft-tissue contrast. | *CT provides better soft-tissue contrast. | ||
| Line 73: | Line 73: | ||
*Coronary angiography may be helpful to detect vascular supply of the tumor by the coronary arteries. | *Coronary angiography may be helpful to detect vascular supply of the tumor by the coronary arteries. | ||
| style="padding: 5px 5px; background: #F5F5F5;" align=center| | | style="padding: 5px 5px; background: #F5F5F5;" align=center| | ||
*The angiographic findings of cardiac myxoma demonstrate feeding vessels, contrast medium poolings, and clusters of tortuous vessels that correspond to tumor vasculature | *The angiographic findings of cardiac myxoma demonstrate feeding vessels, contrast medium poolings, and clusters of [[tortuous]] vessels that correspond to tumor vasculature | ||
| style="padding: 5px 5px; background: #F5F5F5;" align=center| | | style="padding: 5px 5px; background: #F5F5F5;" align=center| | ||
*Angiography can detect the concomitant coronary disease and the unique vascular appearances of cardiac myxoma. | *Angiography can detect the concomitant coronary disease and the unique vascular appearances of cardiac myxoma. | ||
Revision as of 15:16, 29 October 2019
|
Myxoma Microchapters |
|
Diagnosis |
|---|
|
Treatment |
|
Case Studies |
|
Myxoma chest x ray On the Web |
|
American Roentgen Ray Society Images of Myxoma chest x ray |
Editor-In-Chief: C. Michael Gibson, M.S., M.D. [1]; Associate Editor-In-Chief: Maria Fernanda Villarreal, M.D. [2] Cafer Zorkun, M.D., Ph.D. [3] Ahmad Al Maradni, M.D. [4]
Overview
There are no specific chest x-ray findings associated with cardiac myxoma, the results can be reported as normal.
Key Chest X-Ray Findings in Cardiac Myxoma
There are no specific chest x-ray findings associated with cardiac myxoma, the results can be reported as normal.[1] Related imaging findings include cardiomegaly, left atrial enlargement, vascular redistribution, prominent pulmonary trunk, and intracardiac tumoral calcification (rare).
Gallery
-
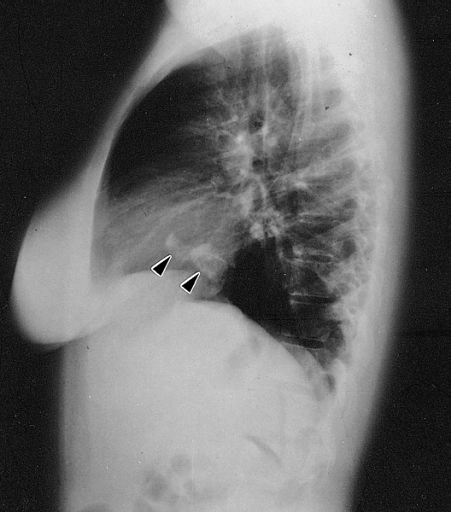
Lateral chest radiograph from a 16-year-old girl with syncope and bacterial endocarditis. The radiograph demonstrates two areas of dense calcification (arrowheads) overlying the posterior aspect of heart. The posterior-anterior (PA) view confirmed location in the heart (not shown). At surgery a calcified myxoma of the right atrium was removed. Image courtesy of Professor Peter Anderson DVM PhD and published with permission © PEIR, University of Alabama at Birmingham, Department of Pathology
| Imaging Technique | Features | Description | Advantages | Limitations |
|---|---|---|---|---|
| Two- or three-dimensional echocardiography |
|
|
|
|
| MRI |
|
|
|
|
| CT |
|
|
|
|
| Angiography |
|
|
|
|
| Chest x-ray |
|
|
|
|
References
- ↑ Cardiac Myxoma. Radiopedia.http://radiopaedia.org/articles/cardiac-myxoma Accessed on November 24, 2015
- ↑ Reeder GS, Khandheria BK, Seward JB, Tajik AJ (1991). "Transesophageal echocardiography and cardiac masses". Mayo Clin. Proc. 66 (11): 1101–9. PMID 1943240.