Jugular venous pressure
Editor-In-Chief: C. Michael Gibson, M.S., M.D. [1] Synonyms and keywords: Jugular venous distention; elevated JVP; JVD; elevated neck veins; distended neck veins
Overview
The jugular venous pressure (JVP, sometimes referred to as jugular venous pulse) is the indirectly observed pressure over the venous system. It can be useful in the differentiation of different forms of heart and lung disease.
Classically three upward deflections and two downward deflections have been described. the upward deflections are the "a" (atrial filling), "c" (ventricular contraction and resulting bulging of tricuspid into the right atrium during isovolumic systole) and "v"= atrial venous filling. and the downward deflections of the wave are the "x"(tricuspid opens and ventricular filling occurs) and the "y" descent reflects filling of ventricle after tricuspid opening.
The interpretation of JVP findings can be challenging and is becoming a lost art, as much of the subtle information previously obtained by careful observation of the JVP can now be gained easily with echocardiography and/or EKG. Certain wave form abnormalities, include "Cannon a-waves", which result when the atrium contracts against a closed tricuspid valve, due to complete heart block (3rd degree heart block), or even in ventricular tachycardia. Another abnormality, "c-v waves", can be a sign of tricuspid regurgitation.
An elevated JVP is the classic sign of venous hypertension (e.g. right-sided heart failure). The paradoxical increase of the JVP with inspiration (instead of the expected decrease) is referred to as the Kussmaul sign, and indicates impaired filling of the right ventricle. The differential diagnosis of Kussmaul's sign includes constrictive pericarditis, restrictive cardiomyopathy, pericardial effusion, and severe right-sided heart failure.
Assessment of Jugular Venous Distention
Assessment for distention of the right Internal jugular vein (IJ) is a difficult skill. Its importance lies in the fact that the IJV is in straight-line communication with the right atrium. The IJV can therefore function as a manometer, with distention indicating elevation of Central venous pressure (CVP). This in turn is an important marker of intravascular volume status and related cardiac function. The focus here is on simply determining whether or not Jugular Venous Distention (JVD) is present. A discussion of the a, c and v waves that make up the jugular venous pulsations can be found elsewhere. These are quite difficult to detect for even the most seasoned physician.
Why is JVD so hard to assess?
The IJV lies deep to skin and soft tissues, which can provide quite a bit of cover. Additionally, this blood vessel is under much lower pressure then the adjacent, pulsating carotid artery. It therefore takes a sharp eye to identify the relatively weak, transmitted venous impulses.
A few things to remember:
- Think anatomically. The right internal jugular vein (IJV) runs between the two heads (sternal and clavicular) of the sternocleidomastoid muscle (SCM) and up in front of the ear. This muscle can be identified by asking the patient to turn their head to the left and into your hand while you provide resistance to the movement. The two heads form the sides of a small triangle, with the clavicle making up the bottom edge. You should be able to feel a shallow defect formed by the borders of these landmarks. Note, you are trying to identify impulses originating from the IJV and transmitted to the overlying skin in this area. You can't actually see the IJV. The external jugular vein (EJV) runs in an oblique direction across the sternocleidomastoid and, in contrast to the IJV, can usually be directly visualized. If the EJV is not readily apparent, have the patient look to the left and valsalva. This usually makes it quite obvious. EJV distention is not always a reliable indicator of elevated CVP as valves, designed to prevent the retrograde flow of blood, can exist within this vessel causing it to appear engorged even when CVP is normal. It also makes several turns prior to connecting with the central venous system and is thus not in a direct line with the right atrium.
- Take your time. Look at the area in question for several minutes while the patient's head is turned to the left. The carotid artery is adjacent to the IJV, lying just medial to it. If you are unsure whether a pulsation is caused by the carotid or the IJ, place your hand on the patient's radial artery and use this as a reference. The carotid impulse coincides with the palpated radial artery pulsation and is characterized by a single upstroke timed with systole. The venous impulse (at least when the patient is in sinus rhythm and there is no tricuspid regurgitation) has three components, each associated with the aforementioned a, c and v waves. When these are transmitted to the skin, they create a series of flickers that are visible diffusely within the overlying skin. In contrast, the carotid causes a single up and down pulsation. Furthermore, the carotid is palpable. The IJ is not and can, in fact, be obliterated by applying pressure in the area where it emerges above the clavicle.
- Search along the entire projected course of the IJV as the top of the pressure wave (which is the point that you are trying to identify) may be higher than where you are looking. In fact, if the patient's CVP is markedly elevated, you may not be able to identify the top of the wave unless they are positioned with their trunk elevated at 45 degrees or more (else their will be no identifiable "top" of the column as the entire IJV will be engorged). After you've found the top of the wave, see what effect sitting straight up and lying down flat have on the height of the column. Sitting should cause it to appear at a lower point in the neck, while lying has the opposite effect. Realize that these maneuvers do not change the actual value of the central venous pressure. They simply alter the position of the top of the pulsations in relation to other structures in the neck and chest.
- Shine a pen light tangentially across the neck. This sometimes helps to accentuate the pulsations.
- If you are still uncertain, apply gentle pressure to the right upper quadrant of the abdomen for 5 to 10 seconds. This elicits Hepatojugular reflux which, in pathological states, will cause blood that has pooled in the liver to flow in a retrograde fashion and fill out the IJV, making the transmitted pulsations more apparent. Make sure that you are looking in the right area when you push as the best time to detect any change in the height of this column of blood is immediately after you apply hepatic pressure.
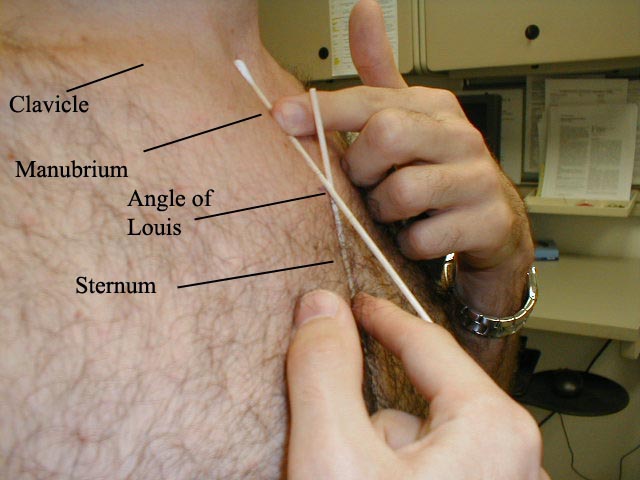
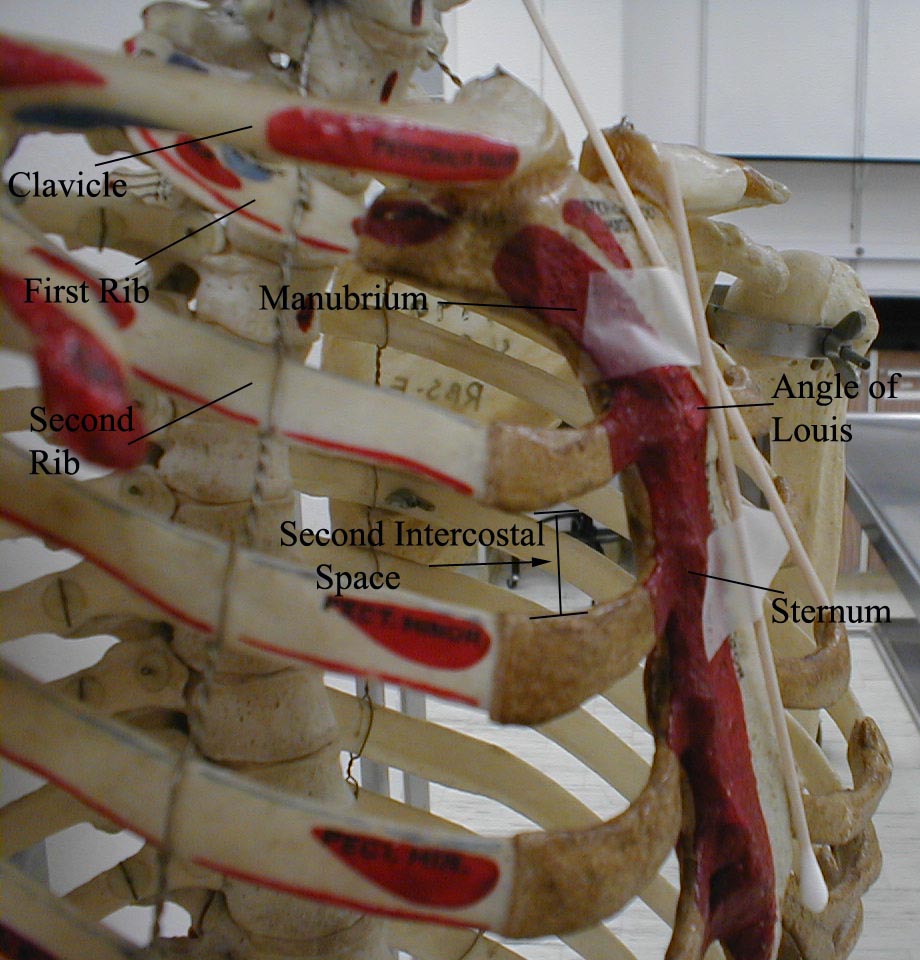
- Once you identify JVD, try to estimate how high in cm the top of the column is above the Angle of Louis. The angle is the site of the joint which connects the manubrium with the rest of the sternum. First identify the suprasternal notch, a concavity at the top of the manubrium. Then walk your fingers downward until you detect a subtle change in the angle of the bone, which is approximately 4 to 5 cm below the notch. This is roughly at the level of the 2nd intercostal space. The vertical distance from the top of the column to this angle is added to 5cm, the rough vertical distance from the angle to the right atrium with the patient lying at a 45 degree angle.
The sum is an estimate of the CVP. However, if you can simply determine with some accuracy whether JVD is present or not, you will be way ahead of he game! Normal is 7-9 cm.
(Images courtesy of Charlie Goldberg, M.D., UCSD School of Medicine and VA Medical Center, San Diego, California)
-
The point at which the Q-tips cross is the Angle of Louis
-
Determining the CVP
-
Elevated JVP
Video Instruction
{{#ev:youtube|uelWjO2U1Hk&feature}}
Causes of Elevated Jugular Venous Pressure
Life Threatening Causes
- Cardiac failure
- Cardiomyopathy
- Constrictive pericarditis
- Chronic obstructive pulmonary disease (copd)
- Heart block
- Hodgkin's lymphoma
- Pulmonary embolism
- Pulmonary hypertension
- Pulmonary valve stenosis
- Restrictive cardiomyopathy
- Right atrial myxoma
- Right heart failure
- Right ventricular dilation
- Right ventricular myocardial infarction
- Tension pneumothorax
Common Causes
- Atrial myxoma
- Bradycardia
- Cardiac failure
- Cardiac tamponade
- Cardiomyopathy
- Chronic obstructive pulmonary disease (copd)
- Constrictive pericarditis
- Heart block
- Hodgkin's lymphoma
- Hyperdynamic circulation
- Junctional rhythm
- Mediastinal emphysema
- Mediastinal neoplasm
- Pericardial effusion
- Pulmonary embolism
- Pulmonary hypertension
- Pulmonary valve stenosis
- Restrictive cardiomyopathy
- Right atrial myxoma
- Right heart failure
- Right ventricular dilation
- Right ventricular myocardial infarction
- Superior vena cava syndrome
- Tricuspid regurgitation
- Tricuspid stenosis
- Tricuspid valve incompetence
- Valsalva maneuver
Causes by Organ System
| Cardiovascular | Atrial fibrillation, Atrial myxoma, Bradycardia, Cardiac failure, Cardiac tamponade, Cardiomyopathy, Chronic obstructive pulmonary disease (copd), Constrictive pericarditis, Heart block, Hodgkin's lymphoma, Hyperdynamic circulation, Junctional rhythm, Mediastinal emphysema, Pericardial effusion, Pulmonary embolism, Pulmonary hypertension, Pulmonary valve stenosis, Restrictive cardiomyopathy, Right atrial myxoma, Right heart failure, Right ventricular dilation, Right ventricular myocardial infarction, Superior vena cava syndrome, Tricuspid regurgitation, Tricuspid stenosis, Tricuspid valve incompetence, Valsalva maneuver |
| Chemical/Poisoning | No underlying causes |
| Dental | No underlying causes |
| Dermatologic | No underlying causes |
| Drug Side Effect | No underlying causes |
| Ear Nose Throat | No underlying causes |
| Endocrine | Goiter, Thymoma |
| Environmental | No underlying causes |
| Gastroenterologic | No underlying causes |
| Genetic | No underlying causes |
| Hematologic | Hypervolemia, Superior vena cava syndrome |
| Iatrogenic | No underlying causes |
| Infectious Disease | No underlying causes |
| Musculoskeletal/Orthopedic | No underlying causes |
| Neurologic | No underlying causes |
| Nutritional/Metabolic | No underlying causes |
| Obstetric/Gynecologic | No underlying causes |
| Oncologic | Atrial myxoma, Hodgkin's lymphoma, Mediastinal neoplasm, Right atrial myxoma, Thymoma |
| Ophthalmologic | No underlying causes |
| Overdose/Toxicity | No underlying causes |
| Psychiatric | No underlying causes |
| Pulmonary | Chronic obstructive pulmonary disease (copd), Mediastinal emphysema, Mediastinal neoplasm, Pulmonary embolism, Pulmonary hypertension, Pulmonary valve stenosis, Sclerosing mediastinitis, Tension pneumothorax |
| Renal/Electrolyte | No underlying causes |
| Rheumatology/Immunology/Allergy | No underlying causes |
| Sexual | No underlying causes |
| Trauma | No underlying causes |
| Urologic | No underlying causes |
| Miscellaneous | No underlying causes |
Causes in Alphabetical Order
The CVP vs the JVP
The central venous pressure (CVP) lies approximately 5 cm above the middle of the right atrium. The CVP is therefore estimated to be the JVP in cm plus 5 cm. Normally the CVP is 5-9 cm of H2O.
Hepatojugular reflux
Hepatojugular reflux, sometimes incorrectly referenced as a "reflex",[1] is an expanded form of the JVP measurement. By pressing on the liver (hepato-) for 15-30 seconds, venous blood is advanced into the circulation. The JVP increases in a normal person, and distention should appear more pronounced. However, a slow decrease of the JVP after checking for hepatojugular reflux can indicate right ventricular failure.
Method

A classical method for quantifying the JVP was described by Borst & Molhuysen in 1952.[2] It has since been modified in various ways.
The patient is positioned under 45°, and the filling level of the jugular vein determined. In healthy people, it is maximum several (3-4) centimetres above the sternal angle. Some doctors employ a venous arc, an instrument to measure the JVP more accurately. A pen-light can aid in discerning the jugular filling level.
Visualization of the JVP
The JVP is easiest to observe if one looks along the surface of the sternocleidomastoid muscle, as it is easier to appreciate the movement relative the neck when looking from the side (as opposed to looking at the surface at a 90 degree angle). Like judging the movement of an automobile from a distance, it is easier to see the movement of an automobile when it is crossing one's path at 90 degrees (i.e. moving left to right or right to left), as opposed to coming toward one. Remember, tangential light is critical.
Differentiation of the JVP from the carotid pulse
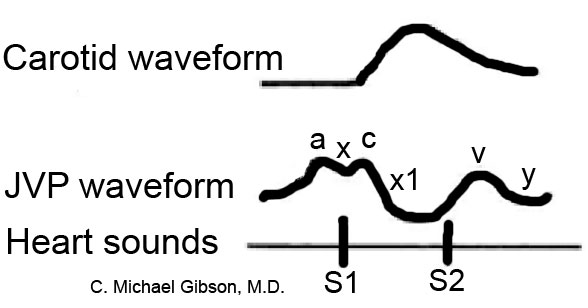
Pulses in the JVP are rather hard to observe, but trained cardiologists do try to discern these as signs of the state of the right atrium.
The JVP and carotid pulse can be differentiated several ways:
- multiphasic - the JVP "beats" twice (in quick succession) in the cardiac cycle. In other words, there are two waves in the JVP for each contraction-relaxation cycle by the heart. The first beat represents that atrial contraction (termed a) and second beat the VENOUS FILLING against a closed tricuspid valve (termed v) and not the commonly mistaken 'ventricular contraction'. The carotid artery only has one beat in the cardiac cycle.
- non-palpable - the JVP cannot be palpated. If one feels a pulse in the neck, it is generally the common carotid artery.
- occludable - the JVP can be stopped by occluding the internal jugular vein by lightly pressing against the neck.
- varies with head-up-tilt (HUT) - the JVP varies with the angle of neck. If a person is standing their JVP appears to be lower on the neck (or may not be seen at all because it below the sternal angle). The carotid pulse's location does not vary with HUT.
- varies with respiration - the JVP usually descreases with deep inspiration. Physiologically, this is a consequence of the Frank-Starling mechanism as inspiration decreases the thoracic pressure and increases blood movement into the heart (venous return), which a healthy heart moves into the pulmonary circulation.
- abdominal jugular reflux (AJR) (also hepatojugular reflux) - the JVP changes with abdominal pressure. If the JVP is elevated 4 cm, it usually returns to its baseline level within 10 seconds. If the JVP remains elevated for a longer period of time it suggests heart failure.
JVP waveform
The jugular venous pulsation has a double waveform. The ‘a’ wave corresponds to atrial contraction and ends synchronously with the carotid artery pulse. The ‘c’ wave occurs when the ventricles begin to contract and is caused by bulging of the atrioventricular (AV) valves backwards towards the atria. The ‘v’ wave is seen when the tricuspid valve is closed, just before ventricular contraction – with and just after the carotid pulse. The ‘v’ wave represents the gradual build-up of blood in the atria while the AV valves are closed during ventricular contraction. The absence of ‘a’ waves is a feature of atrial fibrillation.
Components of the JVP Waveform
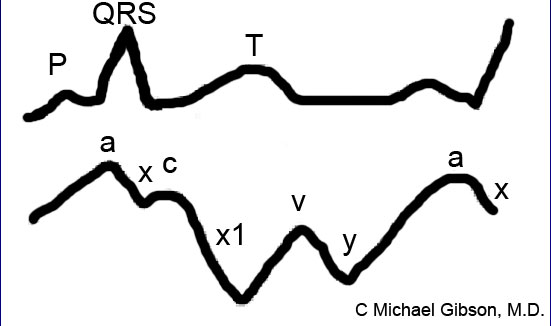
Abnormalities in the JVP Waveforms
| Absence of a wave | Atrial fibrillation |
| Flutter of a wave | Atrial flutter |
| Prominent a waves | First-degree atrioventricular block |
| Large a waves | Tricuspid stenosis, Right atrial myxoma, Pulmonary hypertension, Pulmonic stenosis |
| Absent x descent | Tricuspid regurgitation |
| Prominent x descent | Conditions associated with large a waves |
| Slow y descent | Tricuspid stenosis, Right atrial myxoma |
| Rapid y descent | Constrictive pericarditis, severe Right heart failure, Tricuspid regurgitation, Atrial septal defect |
| Absent y descent | Cardiac tamponade |
References
- ↑ Aronson J (1999). "Hepatojugular reflux". BMJ. 318 (7192): 1172. PMID 10221938. Free Full Text.
- ↑ Borst J, Molhuysen J (1952). "Exact determination of the central venous pressure by a simple clinical method". Lancet. 2 (7): 304–9. PMID 14955978.