Influenza epidemiology and demographics
|
Influenza Microchapters |
|
Diagnosis |
|---|
|
Treatment |
|
Case Studies |
|
Influenza epidemiology and demographics On the Web |
|
American Roentgen Ray Society Images of Influenza epidemiology and demographics |
|
Risk calculators and risk factors for Influenza epidemiology and demographics |
For patient information click here
Editor-In-Chief: C. Michael Gibson, M.S., M.D. [1]
Overview
Influenza, commonly known as flu, is an infectious disease of birds and mammals caused by RNA viruses of the biological family Orthomyxoviridae (the influenza viruses). In humans, common symptoms of influenza infection are fever, sore throat, muscle pains, severe headache, coughing, weakness and general discomfort.
Seasonal variations
Influenza reaches peak prevalence in winter, and because the Northern and Southern Hemisphere have winter at different times of the year, there are actually two different flu seasons each year. This is why the World Health Organization (assisted by the National Influenza Centers) makes recommendations for two different vaccine formulations every year; one for the Northern, and one for the Southern Hemisphere.[2]
It remains unclear why outbreaks of the flu occur seasonally rather than uniformly throughout the year. One possible explanation is that, because people are indoors more often during the winter, they are in close contact more often, and this promotes transmission from person to person. Another is that cold temperatures lead to drier air, which may dehydrate mucus, preventing the body from effectively expelling virus particles. The virus may also survive longer on exposed surfaces (doorknobs, countertops, etc.) in colder temperatures. Increased travel and visitation due to the Northern Hemisphere winter holiday season may also play a role.[3] However, seasonal changes in infection rates are also seen in tropical regions and these peaks of infection are seen mainly during the rainy season.[4] Seasonal changes in contact rates from school-terms, which are a major factor in other childhood diseases such as measles and pertussis, may also play a role in flu. A combination of these small seasonal effects may be amplified by "dynamical resonance" with the endogenous disease cycles.[5] H5N1 exhibits seasonality in both humans and birds.[1]
An alternative hypothesis to explain seasonality in influenza infections is an effect of vitamin D levels on immunity to the virus.[6] This idea was first proposed by Robert Edgar Hope-Simpson in 1965.[7] He proposed that the cause of influenza epidemics during winter may be connected to seasonal fluctuations of vitamin D, which is produced in the skin under the influence of solar (or artificial) UV radiation. This could explain why influenza occurs mostly in winter and during the tropical rainy season, when people stay indoors, away from the sun, and their vitamin D levels fall. Furthermore, some studies have suggested that administering cod liver oil, which contains large amounts of vitamin D, can reduce the incidence of respiratory tract infections.[8]
Epidemic and pandemic spread
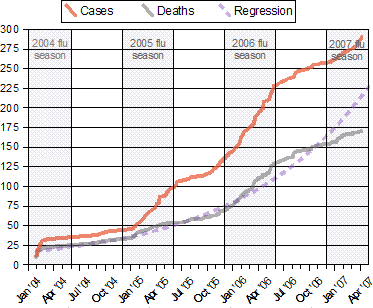
As influenza is caused by a variety of species and strains of viruses, in any given year some strains can die out while others create epidemics while yet another strain can cause a pandemic. Typically, in a year's normal two flu seasons (one per hemisphere) there are between three and five million cases of severe illness and up to 500,000 deaths worldwide, which by some definitions is a yearly influenza epidemic.[9] Although the incidence of influenza can vary widely between years, approximately 36,000 deaths and more than 200,000 hospitalizations are directly associated with influenza every year in America.[10][11][12] Every ten to twenty years a pandemic occurs, which infects a large proportion of the world's population, and can kill tens of millions of people (see history section).
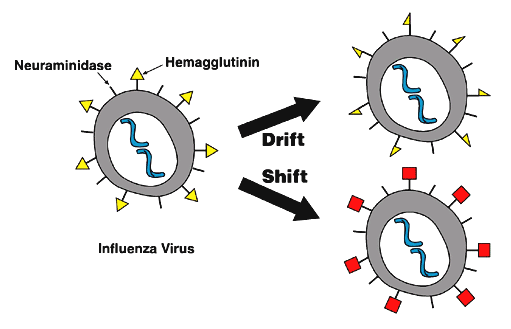
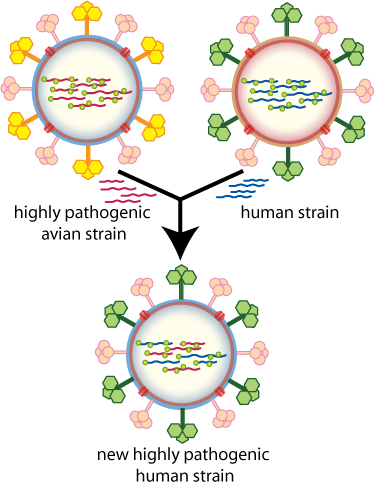
New influenza viruses are constantly being produced by mutation or by reassortment.[13] Mutations can cause small changes in the hemagglutinin and neuraminidase antigens on the surface of the virus. This is called antigenic drift, which creates an increasing variety of strains over time until one of the variants eventually achieves higher fitness, becomes dominant, and rapidly sweeps through the human population – often causing an epidemic.[14] In contrast, when influenza viruses re-assort, they may acquire new antigens — for example by reassortment between avian strains and human strains; this is called antigenic shift. If a human influenza virus is produced with entirely novel antigens, everybody will be susceptible and the novel influenza will spread uncontrollably, causing a pandemic.[15] In contrast to this model of pandemics based on antigenic drift and shift, an alternative approach has been proposed where the periodic pandemics are produced by interactions of a fixed set of viral strains with a human population with a constantly-changing set of immunities to different viral strains.[16]
References
- ↑ 1.0 1.1 WHO Confirmed Human Cases of H5N1 Data published by WHO Epidemic and Pandemic Alert and Response (EPR). Accessed 24 Oct. 2006
- ↑ Recommended composition of influenza virus vaccines for use in the 2006–2007 influenza season WHO report 2006-02-14. Accessed 19 October 2006.
- ↑ Weather and the Flu Season NPR Day to Day, December 17 2003. Accessed, 19 October 2006
- ↑ Shek LP, Lee BW. "Epidemiology and seasonality of respiratory tract virus infections in the tropics." Paediatr Respir Rev. 2003 Jun;4(2):105–11. PMID 12758047
- ↑ Dushoff J, Plotkin JB, Levin SA, Earn DJ. "Dynamical resonance can account for seasonality of influenza epidemics." Proc Natl Acad Sci U S A. 30 November2004;101(48):16915–6. PMID 15557003
- ↑ Cannell, J (2006). "Epidemic influenza and vitamin D". Epidemiol Infect. 134 (6): 1129–40. PMID 16959053. Unknown parameter
|coauthors=ignored (help) - ↑ HOPE-SIMPSON, R. "The nature of herpes zoster: a long-term study and a new hypothesis". Proc R Soc Med. 58: 9–20. PMID 14267505.
- ↑ Linday, L (2004). "Effect of daily cod liver oil and a multivitamin-mineral supplement with selenium on upper respiratory tract pediatric visits by young, inner-city, Latino children: randomized pediatric sites". Ann Otol Rhinol Laryngol. 113 (11): 891–901. PMID 15562899. Unknown parameter
|coauthors=ignored (help) - ↑ Influenza WHO Fact sheet N°211 revised March 2003. Accessed 22 October 2006
- ↑ Thompson, W (2003). "Mortality associated with influenza and respiratory syncytial virus in the United States". JAMA. 289 (2): 179–86. PMID 12517228. Unknown parameter
|coauthors=ignored (help) - ↑ Thompson, W (2004). "Influenza-associated hospitalizations in the United States". JAMA. 292 (11): 1333–40. PMID 15367555. Unknown parameter
|coauthors=ignored (help) - ↑ Flu factsheet National Institute of Allergy and Infectious Diseases Accessed 22 Dec 2006
- ↑
- ↑ "Long intervals of stasis punctuated by bursts of positive selection in the seasonal evolution of influenza A virus". Biol Direct. 1 (1): 34. 2006. PMID 17067369.
- ↑ Parrish, C. "The origins of new pandemic viruses: the acquisition of new host ranges by canine parvovirus and influenza A viruses". Annual Rev Microbiol. 59: 553–86. PMID 16153179. Unknown parameter
|coauthors=ignored (help) - ↑ Recker M, Pybus OG, Nee S, Gupta S (2007). "The generation of influenza outbreaks by a network of host immune responses against a limited set of antigenic types". Proc Natl Acad Sci U S A. 104 (18): 7711–7716. PMID 17460037.