Influenza epidemiology and demographics: Difference between revisions
(Created page with "{{Influenza}} '''For patient information click here''' {{CMG}} ==Overview== '''Influenza''', commonly known as '''flu''', is an [[infect...") |
m (Bot: Removing from Primary care) |
||
| (52 intermediate revisions by 8 users not shown) | |||
| Line 1: | Line 1: | ||
__NOTOC__ | |||
{{Influenza}} | {{Influenza}} | ||
'''For more information about non-human (variant) influenza viruses that may be transmitted to humans, see [[Zoonotic influenza]]'''<br><br> | |||
{{CMG}}; {{AE}} {{AL}} | |||
==Overview== | |||
The CDC estimates that 5 to 20 percent of Americans are affected by the flu during each flu season, which typically lasts from October to March. Children are 2 to 3 times more likely than adults to get sick with the flu, and children frequently spread the virus to others. For elderly people, newborn babies, pregnant women, and people with certain chronic illnesses, the flu and its complications can be life-threatening. Although most people recover from the illness, between 3,000 and 49,000 US citizens die from the flu and its complications every year.<ref>{{cite web| url=http://www.niaid.nih.gov/topics/Flu/understandingFlu/Pages/overview.aspx| title= National Institute of Allergy and Infectious Diseases - Flu Overview}} </ref> | |||
==Epidemiology and Demographics== | |||
== | ===Prevalence=== | ||
*Influenza affects approximately 5 to 10% of adults and 20 to 30% of children worldwide. | |||
*WHO reports 3 to 5 million cases of severe influenza disease, with approximately 250 000 to 500 000 deaths.<ref> {{cite web|url=http://www.who.int/mediacentre/factsheets/fs211/en/| title=WHO Influenza Fact Sheets}}</ref> | |||
===Gender=== | |||
*There is no gender predominance for influenza infection. However, pregnant women are at increased risk of having severe illness and possible complications. | |||
===Age=== | |||
*Influenza viruses cause disease among persons in all age groups. | |||
*Rates of infection are highest among children, but the risks for complications, hospitalizations, and deaths from influenza are higher among persons aged 65 years and older, young children, and persons of any age who have medical conditions that place them at increased risk for complications from influenza (such as immunosuppression and pregnancy). | |||
*During 1990--1999, estimated average rates of influenza-associated pulmonary and circulatory deaths per 100,000 persons were:<ref name=CDCACIP> {{cite web|url=http://www.cdc.gov/flu/professionals/acip/clinical.htm| title=CDC Hospitalizations and Deaths from Influenza}}</ref> | |||
:* 0.4-0.6 among persons aged 0-49 years | |||
:* 7.5 among persons aged 50-64 years | |||
:* 98.3 among persons aged 65 years and older. | |||
=== | ===Mortality=== | ||
{{ | *Number of deaths: '''1,532''' <ref name="CDC Mortality"> {{cite web| url=http://www.cdc.gov/nchs/fastats/flu.htm| title=CDC FastStats Influenza}} </ref> | ||
*Deaths per 100,000 population: '''0.5''' <ref name="CDC Mortality"> {{cite web| url=http://www.cdc.gov/nchs/fastats/flu.htm| title=CDC FastStats Influenza}} </ref> | |||
[[ | ===Vaccination=== | ||
The following data represents the percentage of individuals who received influenza vaccine in the United States:<ref name="CDC Mortality"> {{cite web| url=http://www.cdc.gov/nchs/fastats/flu.htm| title=CDC FastStats Influenza}}</ref> | |||
* '''45.2%''' of children from 6 months to 17 years old received an influenza vaccination during the past 12 months. | |||
* '''26.3%''' of adults aged 18 to 49 years received an influenza vaccination during the past 12 months. | |||
*'''42.7%''' of adults aged 50 to 64 years received an influenza vaccination during the past 12 months. | |||
*'''66.5%''' of adults aged 65 years and over received an influenza vaccination during the past 12 months. | |||
{| | |||
|[[File:Percentage of adults aged 18 and over who received an influenza vaccination during the past 12 months, by age group and quarter US, 1997–2012.png|thumb|350px|Percentage of adults aged 18 and over who received an influenza vaccination during the past 12 months, by age group and quarter: United States, 1997–2012<br> Image obtained from CDC[http://www.cdc.gov/nchs/data/nhis/earlyrelease/earlyrelease201306_04.pdf]]] | |||
|[[File:Percentage of persons who received an influenza vaccination during the past 12 months, by age group and sex US, 2012.png|thumb|350px| Percentage of persons who received an influenza vaccination during the past 12 months, by age group and sex: United States, 2012 <br> Image obtained from CDC[http://www.cdc.gov/nchs/data/nhis/earlyrelease/earlyrelease201306_04.pdf]]] | |||
|} | |||
Influenza | ==Influenza in the United States== | ||
===National and Regional Summary of Select Surveillance Components=== | |||
*The proportion of outpatient visits for influenza-like illness (ILI) was 1.4%, which is below the national baseline of 2.0%. One region reported ILI above their region-specific baseline level. | |||
*Puerto Rico experienced high ILI activity; one state experienced low ILI activity; New York City and 49 states experienced minimal ILI activity and the District of Columbia had insufficient data. | |||
*The geographic spread of influenza in Guam was reported as widespread; Puerto Rico and five states reported local activity; the U.S. Virgin Islands and 36 states reported sporadic activity; and the District of Columbia and nine states reported no influenza activity. | |||
{{#widget:BlueTable}} | |||
{| class="BlueTable" style="font-size:95%; width:82%" | |||
|+ '''''Data cumulative since September 28, 2014 (week 40) <ref name="CDC Epi"> {{cite web|url=http://www.cdc.gov/flu/weekly/ | title=CDC Weekly U.S. Influenza Surveillance Report}} </ref>''''' | |||
|- | |||
!style="width: 100px"|HHS Surveillance Regions | |||
!style="width: 70px"|Out-patient ILI<sup>†</sup> | |||
!style="width: 70px"|Percentage positive for flu<sup>‡</sup> | |||
!style="width: 100px"|Number of jurisdictions reporting regional or widespread activity<sup>§</sup> | |||
!style="width: 70px"|2009 H1N1 | |||
!style="width: 70px"|Type A (H3) | |||
!style="width: 70px"|Type A <br><Small>(Subtyping not performed)</small> | |||
!style="width: 70px"|Type B | |||
!style="width: 70px"|Pediatric Deaths | |||
|- | |||
| Nation||Normal||4.8%||1 of 54||7||267||405||392||1 | |||
|- | |||
| Region 1||Normal||1.6%||0 of 6||0||8||8||4||0 | |||
|- | |||
| Region 2||Elevated||1.1%||0 of 4||1||17||17||11||0 | |||
|- | |||
| Region 3||Normal||1.7%||0 of 6||0||16||16||69||0 | |||
|- | |||
| Region 4||Normal||8.0%||0 of 8||0||56||290||246||1 | |||
|- | |||
| Region 5||Normal||2.1%||0 of 6||3||28||15||12||0 | |||
|- | |||
| Region 6||Normal||4.3%||0 of 5||2||32||26||69||0 | |||
|- | |||
| Region 7||Normal||1.9%||0 of 4||0||12||15||9||0 | |||
|- | |||
| Region 8||Normal||1.2%||0 of 6||0||15||5||6||0 | |||
|- | |||
| Region 9||Normal||3.2%||1 of 5||1||27||27||19||0 | |||
|- | |||
| Region 10||Normal||5.5%||0 of 4||0||56||4||7||0 | |||
|- | |||
|colspan=9| | |||
<small>*HHS regions (Region 1 CT, ME, MA, NH, RI, VT; Region 2: NJ, NY, Puerto Rico, US Virgin Islands; Region 3: DE, DC, MD, PA, VA, WV; Region 4: AL, FL, GA, KY, MS, NC, SC, TN; Region 5: IL, IN, MI, MN, OH, WI; Region 6: AR, LA, NM, OK, TX; Region 7: IA, KS, MO, NE; Region 8: CO, MT, ND, SD, UT, WY; Region 9: AZ, CA, Guam, HI, NV; and Region 10: AK, ID, OR, WA). <br> | |||
† Elevated means the % of visits for Influenza-like illness (ILI) is at or above the national or region-specific baseline. <br> | |||
‡ National data are for current week; regional data are for the most recent three weeks. <br> | |||
§ Includes all 50 states, the District of Columbia, Guam, Puerto Rico, and U.S. Virgin Islands </small> | |||
|} | |||
{| | |||
|[[File:Number of Influenza-Associated Pediatric Deaths by Week of Death.png|thumb|480px| Number of Influenza-Associated Pediatric Deaths by Week of Death: 2011-2012 season to present <br> Image obtained from CDC [http://www.cdc.gov/flu/weekly/] ]] | |||
|[[File:Weekly Influenza Activity Estimates Reported by State.png|thumb|480px|Weekly Influenza Activity Estimates Reported by State (Oct 2014)<br> Image obtained from CDC [http://www.cdc.gov/flu/weekly/] ]] | |||
|} | |||
==Worldwide Influenza== | |||
*During May 18–September 20, typical seasonal patterns of influenza activity occurred in temperate climate Southern Hemisphere countries. | |||
=== | ====South and Central America==== | ||
*In temperate countries of South America, influenza activity began to increase in June, remained elevated through July and mid-August, and decreased in September. Influenza A viruses were reported more frequently than influenza B viruses, and influenza A (H3N2) viruses were predominant in Chile, Argentina, Uruguay, and Paraguay. | |||
*In tropical South America, influenza A viruses were most commonly reported. Influenza A (H3N2) viruses predominated in Brazil and Colombia, whereas influenza B viruses were more frequently reported in Ecuador. In Peru, influenza A (H3N2) and pH1N1 viruses cocirculated, but influenza B viruses also were identified. | |||
*In the Caribbean and Central America, an increase in the number of influenza B viruses was reported in July and August, particularly in Honduras, Jamaica, and Nicaragua, with influenza A viruses cocirculating in Guatemala and Panama. | |||
====Europe and North America==== | |||
*In Europe and North America, influenza activity was low, and small numbers of pH1N1, influenza A (H3N2), and influenza B viruses were identified. | |||
====Asia==== | |||
*In South Asia and Southeast Asia, a decrease in influenza activity was observed during August and September, and influenza A (H3N2) predominated in Cambodia, India, China, and Vietnam, with smaller numbers of influenza B viruses reported. | |||
*In Thailand, influenza B viruses were more frequently reported in July and August, but influenza A (H3N2) and pH1N1 viruses also were identified. | |||
====South Africa==== | |||
*In South Africa, influenza activity began to increase in late May and decreased in early August. Influenza A (H3N2) viruses predominated in that country, but pH1N1 and influenza B viruses also were reported. | |||
====Australia and New Zealand==== | |||
*In Australia and New Zealand, influenza activity began to increase in late July and remained elevated through mid-September. Influenza A viruses predominated in both countries. | |||
==References== | ==References== | ||
{{ | {{Reflist|2}} | ||
{{WH}} | |||
{{WS}} | |||
[[Category:Disease]] | [[Category:Disease]] | ||
[[Category:Pulmonology]] | [[Category:Pulmonology]] | ||
[[Category:Influenza| ]] | [[Category:Influenza| ]] | ||
Latest revision as of 22:24, 29 July 2020
|
Influenza Microchapters |
|
Diagnosis |
|---|
|
Treatment |
|
Case Studies |
|
Influenza epidemiology and demographics On the Web |
|
American Roentgen Ray Society Images of Influenza epidemiology and demographics |
|
Risk calculators and risk factors for Influenza epidemiology and demographics |
For more information about non-human (variant) influenza viruses that may be transmitted to humans, see Zoonotic influenza
Editor-In-Chief: C. Michael Gibson, M.S., M.D. [5]; Associate Editor(s)-in-Chief: Alejandro Lemor, M.D. [6]
Overview
The CDC estimates that 5 to 20 percent of Americans are affected by the flu during each flu season, which typically lasts from October to March. Children are 2 to 3 times more likely than adults to get sick with the flu, and children frequently spread the virus to others. For elderly people, newborn babies, pregnant women, and people with certain chronic illnesses, the flu and its complications can be life-threatening. Although most people recover from the illness, between 3,000 and 49,000 US citizens die from the flu and its complications every year.[1]
Epidemiology and Demographics
Prevalence
- Influenza affects approximately 5 to 10% of adults and 20 to 30% of children worldwide.
- WHO reports 3 to 5 million cases of severe influenza disease, with approximately 250 000 to 500 000 deaths.[2]
Gender
- There is no gender predominance for influenza infection. However, pregnant women are at increased risk of having severe illness and possible complications.
Age
- Influenza viruses cause disease among persons in all age groups.
- Rates of infection are highest among children, but the risks for complications, hospitalizations, and deaths from influenza are higher among persons aged 65 years and older, young children, and persons of any age who have medical conditions that place them at increased risk for complications from influenza (such as immunosuppression and pregnancy).
- During 1990--1999, estimated average rates of influenza-associated pulmonary and circulatory deaths per 100,000 persons were:[3]
- 0.4-0.6 among persons aged 0-49 years
- 7.5 among persons aged 50-64 years
- 98.3 among persons aged 65 years and older.
Mortality
Vaccination
The following data represents the percentage of individuals who received influenza vaccine in the United States:[4]
- 45.2% of children from 6 months to 17 years old received an influenza vaccination during the past 12 months.
- 26.3% of adults aged 18 to 49 years received an influenza vaccination during the past 12 months.
- 42.7% of adults aged 50 to 64 years received an influenza vaccination during the past 12 months.
- 66.5% of adults aged 65 years and over received an influenza vaccination during the past 12 months.
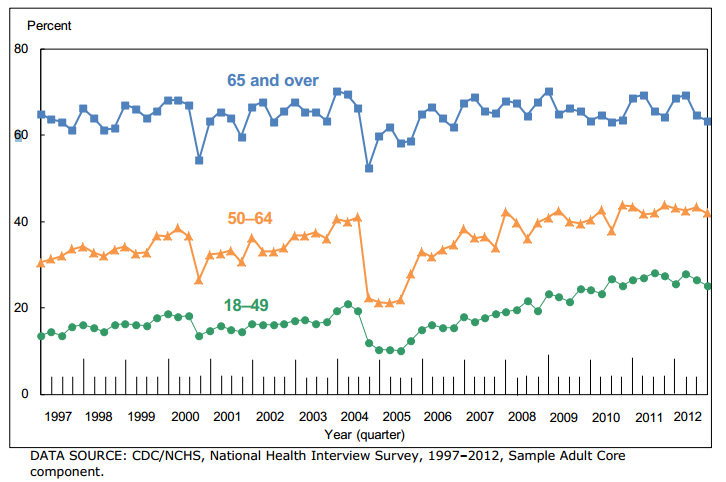 Image obtained from CDC[1] |
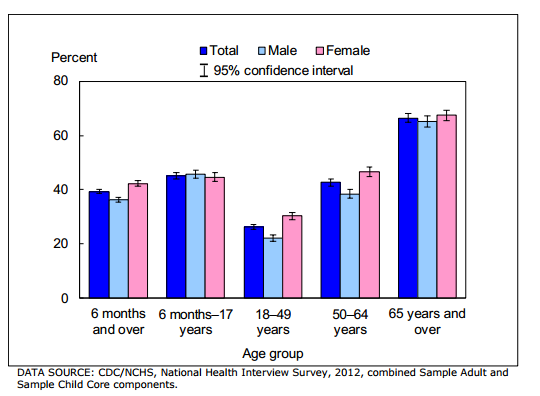 Image obtained from CDC[2] |
Influenza in the United States
National and Regional Summary of Select Surveillance Components
- The proportion of outpatient visits for influenza-like illness (ILI) was 1.4%, which is below the national baseline of 2.0%. One region reported ILI above their region-specific baseline level.
- Puerto Rico experienced high ILI activity; one state experienced low ILI activity; New York City and 49 states experienced minimal ILI activity and the District of Columbia had insufficient data.
- The geographic spread of influenza in Guam was reported as widespread; Puerto Rico and five states reported local activity; the U.S. Virgin Islands and 36 states reported sporadic activity; and the District of Columbia and nine states reported no influenza activity.
| HHS Surveillance Regions | Out-patient ILI† | Percentage positive for flu‡ | Number of jurisdictions reporting regional or widespread activity§ | 2009 H1N1 | Type A (H3) | Type A (Subtyping not performed) |
Type B | Pediatric Deaths |
|---|---|---|---|---|---|---|---|---|
| Nation | Normal | 4.8% | 1 of 54 | 7 | 267 | 405 | 392 | 1 |
| Region 1 | Normal | 1.6% | 0 of 6 | 0 | 8 | 8 | 4 | 0 |
| Region 2 | Elevated | 1.1% | 0 of 4 | 1 | 17 | 17 | 11 | 0 |
| Region 3 | Normal | 1.7% | 0 of 6 | 0 | 16 | 16 | 69 | 0 |
| Region 4 | Normal | 8.0% | 0 of 8 | 0 | 56 | 290 | 246 | 1 |
| Region 5 | Normal | 2.1% | 0 of 6 | 3 | 28 | 15 | 12 | 0 |
| Region 6 | Normal | 4.3% | 0 of 5 | 2 | 32 | 26 | 69 | 0 |
| Region 7 | Normal | 1.9% | 0 of 4 | 0 | 12 | 15 | 9 | 0 |
| Region 8 | Normal | 1.2% | 0 of 6 | 0 | 15 | 5 | 6 | 0 |
| Region 9 | Normal | 3.2% | 1 of 5 | 1 | 27 | 27 | 19 | 0 |
| Region 10 | Normal | 5.5% | 0 of 4 | 0 | 56 | 4 | 7 | 0 |
|
*HHS regions (Region 1 CT, ME, MA, NH, RI, VT; Region 2: NJ, NY, Puerto Rico, US Virgin Islands; Region 3: DE, DC, MD, PA, VA, WV; Region 4: AL, FL, GA, KY, MS, NC, SC, TN; Region 5: IL, IN, MI, MN, OH, WI; Region 6: AR, LA, NM, OK, TX; Region 7: IA, KS, MO, NE; Region 8: CO, MT, ND, SD, UT, WY; Region 9: AZ, CA, Guam, HI, NV; and Region 10: AK, ID, OR, WA). | ||||||||
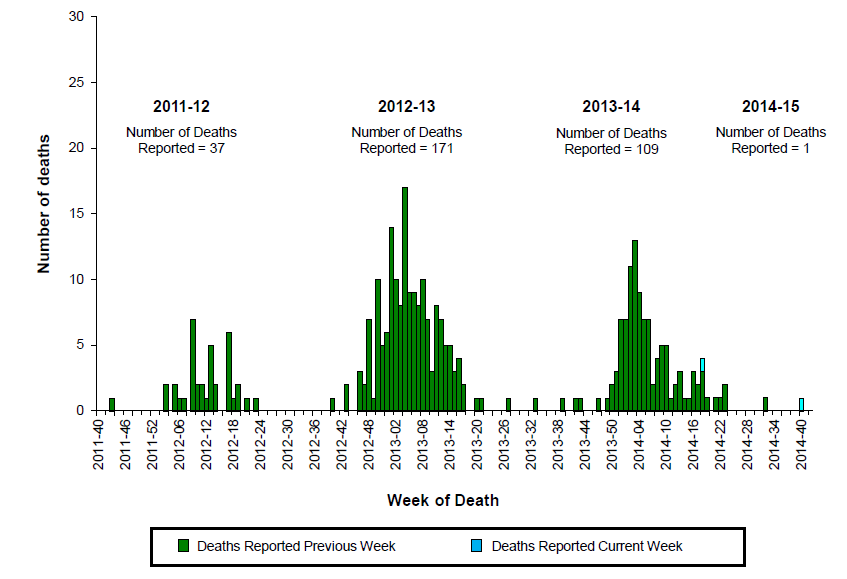 Image obtained from CDC [3] |
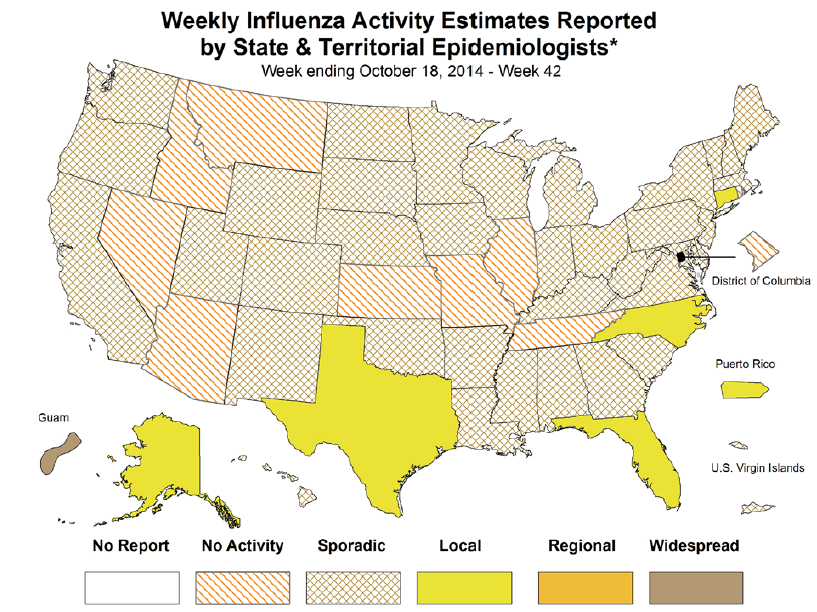 Image obtained from CDC [4] |
Worldwide Influenza
- During May 18–September 20, typical seasonal patterns of influenza activity occurred in temperate climate Southern Hemisphere countries.
South and Central America
- In temperate countries of South America, influenza activity began to increase in June, remained elevated through July and mid-August, and decreased in September. Influenza A viruses were reported more frequently than influenza B viruses, and influenza A (H3N2) viruses were predominant in Chile, Argentina, Uruguay, and Paraguay.
- In tropical South America, influenza A viruses were most commonly reported. Influenza A (H3N2) viruses predominated in Brazil and Colombia, whereas influenza B viruses were more frequently reported in Ecuador. In Peru, influenza A (H3N2) and pH1N1 viruses cocirculated, but influenza B viruses also were identified.
- In the Caribbean and Central America, an increase in the number of influenza B viruses was reported in July and August, particularly in Honduras, Jamaica, and Nicaragua, with influenza A viruses cocirculating in Guatemala and Panama.
Europe and North America
- In Europe and North America, influenza activity was low, and small numbers of pH1N1, influenza A (H3N2), and influenza B viruses were identified.
Asia
- In South Asia and Southeast Asia, a decrease in influenza activity was observed during August and September, and influenza A (H3N2) predominated in Cambodia, India, China, and Vietnam, with smaller numbers of influenza B viruses reported.
- In Thailand, influenza B viruses were more frequently reported in July and August, but influenza A (H3N2) and pH1N1 viruses also were identified.
South Africa
- In South Africa, influenza activity began to increase in late May and decreased in early August. Influenza A (H3N2) viruses predominated in that country, but pH1N1 and influenza B viruses also were reported.
Australia and New Zealand
- In Australia and New Zealand, influenza activity began to increase in late July and remained elevated through mid-September. Influenza A viruses predominated in both countries.