Hemorrhoids
| Hemorrhoids | |
 | |
|---|---|
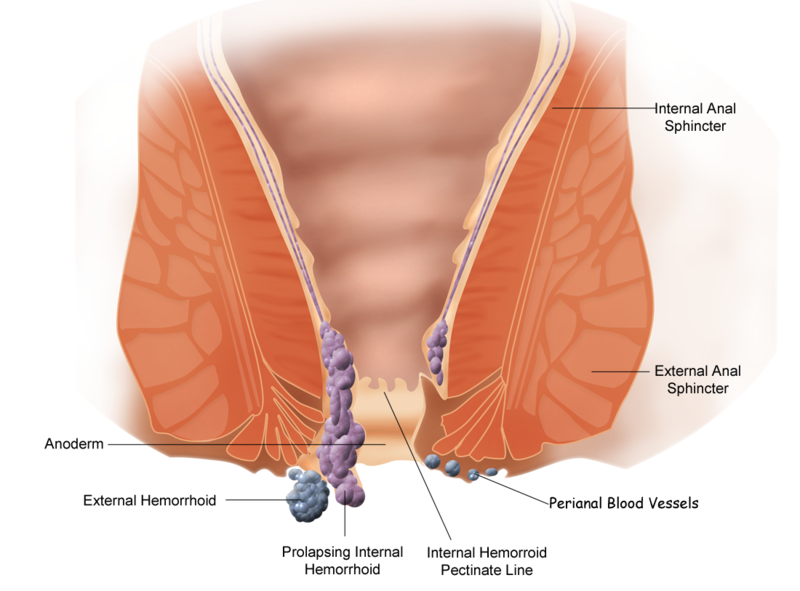
| Schematic demonstrating the anatomy of hemorrhoids. | |
| ICD-10 | I84 |
| ICD-9 | 455 |
| MedlinePlus | 000292 |
|
WikiDoc Resources for Hemorrhoids |
|
Articles |
|---|
|
Most recent articles on Hemorrhoids Most cited articles on Hemorrhoids |
|
Media |
|
Powerpoint slides on Hemorrhoids |
|
Evidence Based Medicine |
|
Clinical Trials |
|
Ongoing Trials on Hemorrhoids at Clinical Trials.gov Clinical Trials on Hemorrhoids at Google
|
|
Guidelines / Policies / Govt |
|
US National Guidelines Clearinghouse on Hemorrhoids
|
|
Books |
|
News |
|
Commentary |
|
Definitions |
|
Patient Resources / Community |
|
Patient resources on Hemorrhoids Discussion groups on Hemorrhoids Patient Handouts on Hemorrhoids Directions to Hospitals Treating Hemorrhoids Risk calculators and risk factors for Hemorrhoids
|
|
Healthcare Provider Resources |
|
Causes & Risk Factors for Hemorrhoids |
|
Continuing Medical Education (CME) |
|
International |
|
|
|
Business |
|
Experimental / Informatics |
For patient information click here
Editor-In-Chief: Dr Ajit Naniksingh Kukreja {M.S, F.I.C.S [USA], LL.B}
Associate Editor-In-Chief: Mohammed A. Sbeih, M.D.[1] Phone:617-849-2629
Overview
Hemorrhoids, haemorrhoids, emerods, or piles are varicosities or swelling and inflammation of veins in the rectum and anus.
Prevalence
Hemorrhoids are common. In the USA, the prevalence is about 4.4%.[1][2] It is estimated that approximately one half of all Americans have had this condition by the age of 50, and that 50% to 85% of the world's population will be affected by hemorrhoids at some time in their life. However, only a small number seek medical treatment. Annually, only about 500,000 in the U.S. are medically treated for massive hemorrhage, with 10 to 20% of them requiring surgeries.
The common man in general tolerates the disease for a long time ,self treating with lot of ointments available over the counter and seeks medical aid only when intolerable
The main reasons for seeking delayed advise are as follows: 1] Myths about the surgical treatment 2] Postoperative pain 3] Fear of incontinence after surgery
But the latest in Biomedical engineering has a lot to offer in newer modalities of management of hemorrhoids
Causes
The causes of hemorrhoids include genetic predisposition (weak rectal vein walls and/or valves), straining during bowel movements, and too much pressure on the rectal veins due to poor muscle tone or poor posture. Similarly, sitting for prolonged periods of time can cause hemorrhoids. Hypertension, particularly in the portal vein, can also cause hemorrhoids because of the connections between the portal vein and the vena cava which occur in the rectal wall - known as portocaval anastomoses.[3]
Additional factors that can influence the course of hemorrhoids (mostly by increasing rectal vein pressure), especially for those with a genetic predisposition, are obesity and a sedentary lifestyle.
Increased straining during bowel movements, (e.g. constipation, diarrhea) may lead to hemorrhoids. [4]
Pregnancy causes hypertension and increases strain during bowel movements, and thus hemorrhoids are often associated with pregnancy.
Excessive consumption of alcohol or caffeine can both cause hemorrhoids.[5] Both can cause diarrhea. Alcohol can also cause alcoholic liver disease leading to portal hypertension. Caffeine on the other hand can cause general hypertension.
Food
Dehydration can cause a hard stool or chronic constipation which can lead to hemorrhoidal irritation. An excess of lactic acid in the stool, a product of excessive consumption of dairy products such as cheese, can cause irritation and a reduction of consumption can bring relief. Vitamin E deficiency is also a common cause.
Food considered "probiotic", such as yogurt with active culture, may help keep the gut functioning normally and thus help prevent flare-ups, as will the consumption of fruit.
Complete List of Differential Diagnoses[6]
- Anal fissure or fistula
- Condylomata acuminata
- External hemorrhoids
- External skin tag
- Hypertrophied anal papilla
- Internal hemorrhoids
- Perirectal abscess
- Rectal cavernous hemangioma
- Rectal or anal cancer
- Rectal polyp
- Rectal prolapse
- Rectal varices
Types of hemorrhoids

- (I84.3-I84.5) External hemorrhoids are those that occur outside of the anal verge (the distal end of the anal canal). They are sometimes painful, and can be accompanied by swelling and irritation. Itching, although often thought to be a symptom from external hemorrhoids, is more commonly due to skin irritation.
- (I84.3) External hemorrhoids are prone to thrombosis: if the vein ruptures and a blood clot develops, the hemorrhoid becomes a thrombosed hemorrhoid.[7]
- (I84.0-I84.2) Internal hemorrhoids are those that occur inside the rectum. As this area lacks pain receptors, internal hemorrhoids are usually not painful and most people are not aware that they have them. Internal hemorrhoids, however, may bleed when irritated.
- (I84.1) Untreated internal hemorrhoids can lead to two severe forms of hemorrhoids: prolapsed and strangulated hemorrhoids:
By degree of prolapse
The most common grading system was developed by Banov:[8][9]
- Grading of Internal Hemorrhoids
- Grade I: The hemorrhoids do not prolapse.
- Grade II: The hemorrhoids prolapse upon defecation but spontaneously reduce.
- Grade III: The hemorrhoids prolapse upon defecation, but must be manually reduced.
- Grade IV: The hemorrhoids are prolapsed and cannot be manually reduced.
Prevention
Prevention of hemorrhoids includes drinking more fluids, eating more dietary fiber (such as fiber supplements, fruits and vegetables, and cereals high in fiber), exercising, practicing better posture, and reducing bowel movement strain and time. Hemorrhoid sufferers should avoid using laxatives and should strictly limit time straining during bowel movement. Wearing tight clothing and underwear will also contribute to irritation and poor muscle tone in the region and promote hemorrhoid development. Some sufferers report a more comfortable experience without underwear or wearing only very lightweight panties, etc.
Fluids emitted by the intestinal tract may contain irritants that may increase the fissures associated with hemorrhoids. Washing the anus with cool water and soap may reduce the swelling and increase blood supply for quicker healing and may remove irritating fluid.
Kegel exercises for the pelvic floor may also prove helpful.
Many people do not get a sufficient supply of dietary fiber (20 to 25 grams daily) and small changes in a person's daily diet can help tremendously in both prevention and treatment of hemorrhoids.
Use of squat toilets
Based on their very low incidence in the developing world, where people squat for bodily functions, hemorrhoids have been attributed to the use of the unnatural "sitting" toilet.[10][11] In 1987, an Israeli physician, Dr. Berko Sikirov, published a study testing this hypothesis by having hemorrhoid sufferers convert to squat toilets.[12] Eighteen of the 20 patients were completely relieved of their symptoms (pain and bleeding) with no recurrence, even 30 months after completion of the study. This chart summarizes the results.
No follow-up studies have ever been published. The American Society of Colon & Rectal Surgeons is silent regarding the therapeutic value of squatting.
Examination
After visual examination of the anus and surrounding area for external or prolapsed hemorrhoids, a doctor would conduct a digital examination. In addition to probing for hemorrhoidal bulges, a doctor would also look for indications of rectal tumor or polyp, enlarged prostate and abscesses.
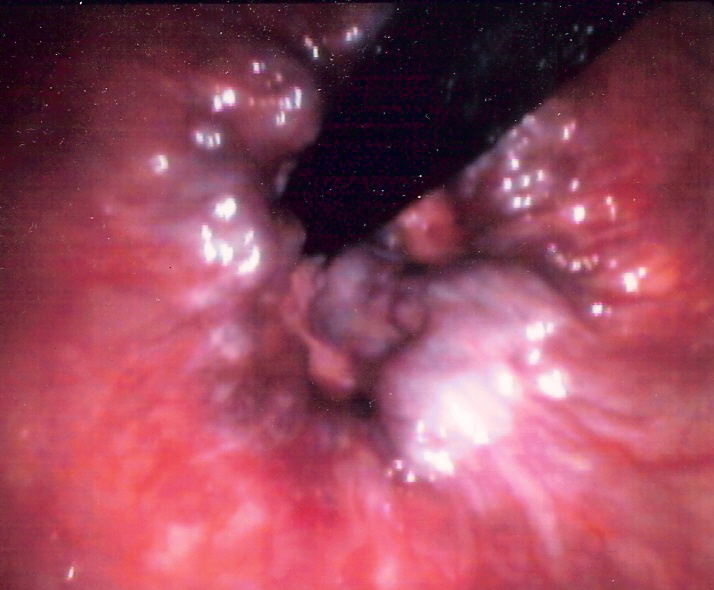
Visual confirmation of hemorrhoids can be done by doing an anoscopy, using a medical device called an anoscope. This device is basically a hollow tube with a light attached at one end that allows the doctor to see the internal hemorrhoids, as well as polyps in the rectum.
If warranted, more detailed examinations, such as sigmoidoscopy and colonoscopy can be performed. In sigmoidoscopy, the last 60cm of the colon and rectum are examined whereas in colonoscopy the entire bowel is examined.
A pathologist will look for dilated vascular spaces which exhibit thrombosis and recanalization.
Treatments
Treatments for hemorrhoids vary in their cost, risk, and effectiveness. Different cultures and individuals approach treatment differently. Some of the treatments used are listed here in increasing order of intrusiveness and cost.
For many people, hemorrhoids are mild and temporary conditions that heal spontaneously or by the same measures recommended for prevention. There is no medicine that will cure hemorrhoids, but local treatments such as warm sitz baths, using a bidet, extendable showerhead, cold compress, or topical analgesic (such as Nupercainal), can provide temporary relief. Consistent use of medicated creams during the early stages of a hemorrhoid flare-up will also provide relief and may stave off further development and irritation. However, creams containing steroid preparations weaken the skin and may contribute to further flare-ups. Keep the area clean and dry, with some lubrication provided by hemorrhoidal creams or a lubricant. Ointment or suppositories such as Proctosedyl [13][14] and Faktu [15] can also relieve the symptoms.
Natural treatments
Some people claim to have successfully applied natural procedures for treatment or reversal of chronic conditions. These procedures largely echo the prevention measures. However, self-care measures, including herbal or "natural" remedies, should not be undertaken without medical consent to avoid possible drug interactions. They include:
- Diet-The condition is caused by overeating and by simply dieting for a week (or more), the hemorrhoids will self-heal. No other treatment will be required.
- Reducing regional pressure in such ways as improving posture and muscle tone, or in severe cases, undergoing a profound psychophysical reeducation, by a method such as the Alexander Technique.
- Taking herbs and dietary supplements that strengthen vein walls, such as butcher's broom, horse chestnut, bromelain, and Japanese pagoda tree extracts. Drinking 99% pure aloe juice can also relieve itching and swelling.
- Topical application of natural astringents and soothing agents, such as Witch hazel (astringent), cranesbill, aloe vera, and honey
- Drinking chamomile tea several times a day
- Eating fiber-rich bulking agents such as plantain and Psyllium seed husks to help create soft stool that is easy to pass to lessen the irritation of existing hemorrhoids.
- Using the squatting position for bowel movements.[16]
The combination of internal and external remedies is particularly recommended, e.g. witch-hazel suppositories combined with frequent cups of strong chamomile tea.[17]
Oral dietary supplementation can help to treat and prevent many complications of hemorrhoids, and natural botanicals such as Butchers Broom, Horse Chestnut, and bioflavonoids can be an effective addition to hemorrhoid treatment.[18]
Butcher's Broom
Butcher’s broom extract, or Ruscus aculeatus, contains ruscogenins that have anti-inflammatory and vasoconstrictor effects. Supplementation with Butcher’s Broom helps tighten and strengthen veins. Butcher’s broom has traditionally been used to treat venous problems including hemorrhoids and varicose veins.[19][20][21]
Horse Chestnut
Horse chestnut extract, or Aesculus hippocastanum, contains a saponin known as aescin, that has anti-inflammatory, anti-edema, and venotonic actions. Aescin improves tone in vein walls, thereby strengthening the support structure of the vein. Double blind studies have shown that supplementation with horse chestnut helps relieve the pain and swelling associated with chronic venous insufficiency.[22][23]
Bilberry Bioflavonoid
Bilberry extract, or Vaccinium myrtillus, is an anthocyanoside bioflavonoid. Supplementation with this potent flavonoid protects and maintains venous strength and function.[19][24]
Medical treatments
Some people require the following medical treatments for chronic or severe hemorrhoids:
- Rubber band ligation
- sometimes called Baron ligation. Elastic bands are applied onto an internal hemorrhoid to cut off its blood supply.[25] Within several days, the withered hemorrhoid is sloughed off during normal bowel movement.
- Hemorrhoidolysis/Galvanic Electrotherapy
- desiccation of the hemorrhoid by electrical current.
- Sclerotherapy (injection therapy)
- sclerosant or hardening agent is injected into hemorrhoids. This causes the vein walls to collapse and the hemorrhoids to shrivel up.
- Cryosurgery
- a frozen tip of a cryoprobe is used to destroy hemorrhoidal tissues.[26] Rarely used anymore because of side effects.
- Laser, infrared or BICAP coagulation
- laser, infrared beam, or electricity is used to cauterize the affected tissues. Lasers are now much less popular. Infrared coagulation has been studied in comparison with RBL and found to be as effective in hemorrhoids up to grade III. These are the most readily available non-surgical procedures in the US.
- Hemorrhoidectomy
- a true surgical procedure to excise and remove hemorrhoids. Has possible correlation with incontinence issues later in life; in addition, many patients complain that pain during recovery is severe. For this reason is often now recommended only for severe (grade IV) hemorrhoids.
- Stapled Hemorrhoidectomy
- Also called the procedure for prolapse and hemorrhoids, it is designed to resect soft tissue proximal to the dentate line, which disrupts the blood flow to the hemorrhoids. It is generally less painful than complete removal of hemorrhoids and also allows for faster recovery times. It's meant for hemorrhoids that fall out or bleed and is not helpful for painful outside conditions.
- Enema
- This Practice is used to clean the rectum. While it is a simple procedure, it can be complicated by hemorrhoids, so in such cases, it should be done by a doctor. In an enema, water is injected into the rectum and then flushed out, cleaning the area.
- Doppler Guided Hemorrhoidal Artery Ligation
- The only evidence based surgery for all grades of hemorrhoids. It does not involve cutting tissues or even a stay at the hospital; patients are usually back to work on the same day. It is the best treatment for bleeding piles, as the bleeding stops immediately. [27]
Diseases with similar symptoms
Symptoms associated with rectal cancer, anal fissure, anal abscess, anal fistula, and other diseases may be similar to those produced by hemorrhoids and may be reduced by the topical analgesic methods described above. For this reason, it is a good idea to consult with a physician when these symptoms are encountered, particularly for the first time, and periodically should the problem continue. In the US, colonoscopy is recommended as a general diagnostic for those over age 50 (40 with family history of bowel cancers); a clear (normal) scope is good for 10 years.
References
- ↑ Hemorrhoid at eMedicine
- ↑ Johanson JF, Sonnenberg A (1990). "The prevalence of hemorrhoids and chronic constipation. An epidemiologic study". Gastroenterology. 98 (2): 380–6. PMID 2295392.
- ↑ "Causes of Hemorrhoids". Mayo Clinic. Nov 28, 2006. Retrieved 2007-12-07.
- ↑ Harms R (Nov 3, 2007). "Hemorrhoids during pregnancy: Treatment options". MayoClinic. Retrieved 2007-11-28.
- ↑ Burney RE (November 2005). "Hemorrhoids". University of Michigan Health System. Retrieved 2007-11-28.
- ↑ isbn=140510368X Kahan, Scott, Smith, Ellen G. In A Page: Signs and Symptoms. Malden, Massachusetts: Blackwell Publishing, 2004:75
- ↑ E. Gojlan, Pathology, 2nd ed. Mosby Elsevier, Rapid Review series.
- ↑
- ↑ Banov L, Knoepp LF, Erdman LH, Alia RT (1985). "Management of hemorrhoidal disease". J S C Med Assoc. 81 (7): 398–401. PMID 3861909.
- ↑ Sikirov BA (1989). "Primary constipation: an underlying mechanism". Med. Hypotheses. 28 (2): 71–3. PMID 2927355.
- ↑ Sikirov D (2003). "Comparison of straining during defecation in three positions: results and implications for human health". Dig. Dis. Sci. 48 (7): 1201–5. PMID 12870773.
- ↑ Sikirov BA (1987). "Management of hemorrhoids: a new approach". Isr. J. Med. Sci. 23 (4): 284–6. PMID 3623887.
- ↑ http://www.netdoctor.co.uk/medicines/100002157.html
- ↑ http://www.medbroadcast.com/drug_info_details.asp?brand_name_id=946
- ↑ http://www.vghks.gov.tw/ph/%E8%99%95%E6%96%B9%E9%9B%86/drug/faktu.htm
- ↑ Christine Dimmer, Brian Martin, Noeline Reeves and Frances Sullivan (1996). "Squatting for the Prevention of Hemorrhoids". Townsend Letter for Doctors & Patients (159): 66–70. Unknown parameter
|month=ignored (help) - ↑ K. Kraft and C. Hobbs, Pocket Guide to Herbal Medicine. New York: Thieme.
- ↑ MacKay D (2001). "Hemorrhoids and varicose veins: a review of treatment options" (PDF). Altern Med Rev. 6 (2): 126–40. PMID 11302778.
- ↑ 19.0 19.1 Pizzorno JE and Murray MT, eds., ed. (1998). Encyclopedia of Natural Medicine (revised 2nd edition ed.). CA: Prima Publishing. p. 829.
- ↑ Rudofsky G (1989). "[Improving venous tone and capillary sealing. Effect of a combination of Ruscus extract and hesperidine methyl chalcone in healthy probands in heat stress]". Fortschr. Med. (in German). 107 (19): 52, 55–8. PMID 2668140.
- ↑ Cappelli R, Nicora M, Di Perri T (1988). "Use of extract of Ruscus aculeatus in venous disease in the lower limbs". Drugs Exp Clin Res. 14 (4): 277–83. PMID 3048951.
- ↑ Pittler MH, Ernst E (1998). "Horse-chestnut seed extract for chronic venous insufficiency. A criteria-based systematic review". Arch Dermatol. 134 (11): 1356–60. PMID 9828868.
- ↑ Diehm C, Trampisch HJ, Lange S, Schmidt C (1996). "Comparison of leg compression stocking and oral horse-chestnut seed extract therapy in patients with chronic venous insufficiency". Lancet. 347 (8997): 292–4. PMID 8569363.
- ↑ Murray MT. (1996). Encyclopedia of Nutritional Supplements. NY: Three Rivers Press. p. 326.
- ↑ Longman RJ, Thomson WH (2006). "A prospective study of outcome from rubber band ligation of piles". Colorectal Dis. 8 (2): 145–8. doi:10.1111/j.1463-1318.2005.00873.x. PMID 16412076.
- ↑ MacLeod JH (1982). "In defense of cryotherapy for hemorrhoids. A modified method". Dis. Colon Rectum. 25 (4): 332–5. PMID 6979469.
- ↑ Scheyer M, Antonietti E, Rollinger G, Mall H, Arnold S (2006). "Doppler-guided hemorrhoidal artery ligation". Am. J. Surg. 191 (1): 89–93. doi:10.1016/j.amjsurg.2005.10.007. PMID 16399113.