Hemorrhagic stroke pathophysiology: Difference between revisions
| Line 67: | Line 67: | ||
**Secondary to prolonged [[hypertension]] (occurs when an artery branches in a weakened area of artery's wall) | **Secondary to prolonged [[hypertension]] (occurs when an artery branches in a weakened area of artery's wall) | ||
*Rupture of an abnormal connection between arteries and veins ([[arteriovenous malformation AVM]]) | *Rupture of an abnormal connection between arteries and veins ([[arteriovenous malformation AVM]]) | ||
*Inflamed artery | *Inflamed artery ([[Septic emboli]]) travels to an artery that supplies the brain, and causes inflammation and as a result the inflamed artery may weaken and rupture | ||
===Gross pathology=== | ===Gross pathology=== | ||
Latest revision as of 22:31, 5 December 2016
|
Hemorrhagic stroke Microchapters |
|
Diagnosis |
|---|
|
Treatment |
|
AHA/ASA Guidelines for the Management of Spontaneous Intracerebral Hemorrhage (2015) |
|
AHA/ASA Guidelines for the Management of Aneurysmal Subarachnoid Hemorrhage (2012) |
|
AHA/ASA Guideline Recommendation for the Primary Prevention of Stroke (2014) |
|
AHA/ASA Guideline Recommendations for Prevention of Stroke in Women (2014) Sex-Specific Risk Factors
Risk Factors Commoner in Women |
|
Case Studies |
|
Hemorrhagic stroke pathophysiology On the Web |
|
American Roentgen Ray Society Images of Hemorrhagic stroke pathophysiology |
|
Risk calculators and risk factors for Hemorrhagic stroke pathophysiology |
Editor-In-Chief: C. Michael Gibson, M.S., M.D. [1]; Associate Editor(s)-in-Chief: Sara Mehrsefat, M.D. [2]
Overview
Pathophysiology
A hemorrhagic stroke, or cerebral hemorrhage, is a form of stroke that occurs when a blood vessel in the brain ruptures or bleeds. Like ischemic strokes, hemorrhagic strokes interrupt the brain's blood supply because the bleeding vessel can no longer carry the blood to its target tissue. In addition, blood irritates brain tissue, disrupting the delicate chemical balance, and, if the bleeding continues, it can cause increased intracranial pressure which physically impinges on brain tissue and restricts blood flow into the brain. In this respect, hemorrhagic strokes are more dangerous than their more common counterpart, ischemic strokes. There are two types of hemorrhagic stroke: intracerebral hemorrhage, and subarachnoid hemorrhage. Amphetamine abuse quintuples, and cocaine abuse doubles, the risk of hemorrhagic strokes.
Intracerebral hemorrhage
The exact cause of brain damage following intracerebral hemorrhage is unknown. It is thought that ICH may result in brain injury by following mechanisms:[1][2]
- Neuronal ischemia following decreased blood flow to the area surrounding the clot
- Overexpression of matrix metalloproteinases (MMPs) which may result in the breakdown of the blood brain barrier and edema
Intraparenchymal hemorrhage
- High blood pressure and aging blood vessels are the most common causes of intracerebral hemorrhage (intraparenchymal hemorrhage).Hypertensive Intracerebral hemorrhage (ICH) usually results from spontaneous rupture of a small artery deep in the brain.[3][4] Breaks in the vessel wall usually occurs following chronic hypertension. Prolonged hypertentsion usually result in intimal hyperplasia and hyalinosis, which may result in focal necrosis and cause in vessel wall breaks. Massive hemorrhage may occur when the patients have a bleeding disorder and clotting system is unable to control the bleeding.[5]
- Intracerebral hemorrhage can also caused by an arteriovenous malformation (AVM). AVM occurs as a result of abnormal connection between arteries and veins in the brain and can result in vessels break and bleed into the brain.
- Additionally, In older people, an abnormal protein called amyloid may accumulate in arteries of the brain and result in amyloid antipathy. Cerebral amyloid angiopathy weakens the arteries and can cause hemorrhage.
Anatomical locations
The most common sites include:
- Basal ganglia (especially the putamen)
- Thalamus
- Cerebellum
- Pons
The small arteries in these areas seem more sensitive to hypertension and as a result, it may progress to vascular injury.
If intracerebral hemorrhage (ICH) occurs in other brain areas or in non hypertensive patients, the other causes of intracerebral hemorrhage should be considered such as:
- Neoplasms
- Hemorrhagic disorders
- Vascular malformations
- Cerebral amyloid angiopathy
Intraventricular hemorrhage
Intraventricular hemorrhage (IVH) can be:[6][7]
- Primary, confined to the ventricles
- Secondary, originating as an extension of an ICH
Most IVH is secondary and related to hypertensive hemorrhages involving the basal ganglia and thalamus.
Microbleeds
It is a clinically silent cerebral microbleeds directly into the brain tissue. It is thought that intimal hyperplasia and hyalinosis following hypertension and amyloid disposition may result in pseudoaneurysm formation and blood vessel leakage.[8][9]
Associated conditions
Anatomical locations
The microbleeds anatomical locations are varies with their etiology:[9]
- Hypertensive microbleeds
- Deep subcortical and infratentorial regions
- Amyloid microbleeds
- Superficial lobar regions of the cerebral hemispheres
Subarachnoid hemorrhage

Subarachnoid hemorrhage is considered a stroke when it occurs spontaneously (not result from external forces and head trauma).
A spontaneous hemorrhage in the brain usually results from:
- Sudden rupture of an aneurysm in an artery in the brain
- Congenital aneurysms
- Secondary to prolonged hypertension (occurs when an artery branches in a weakened area of artery's wall)
- Rupture of an abnormal connection between arteries and veins (arteriovenous malformation AVM)
- Inflamed artery (Septic emboli) travels to an artery that supplies the brain, and causes inflammation and as a result the inflamed artery may weaken and rupture
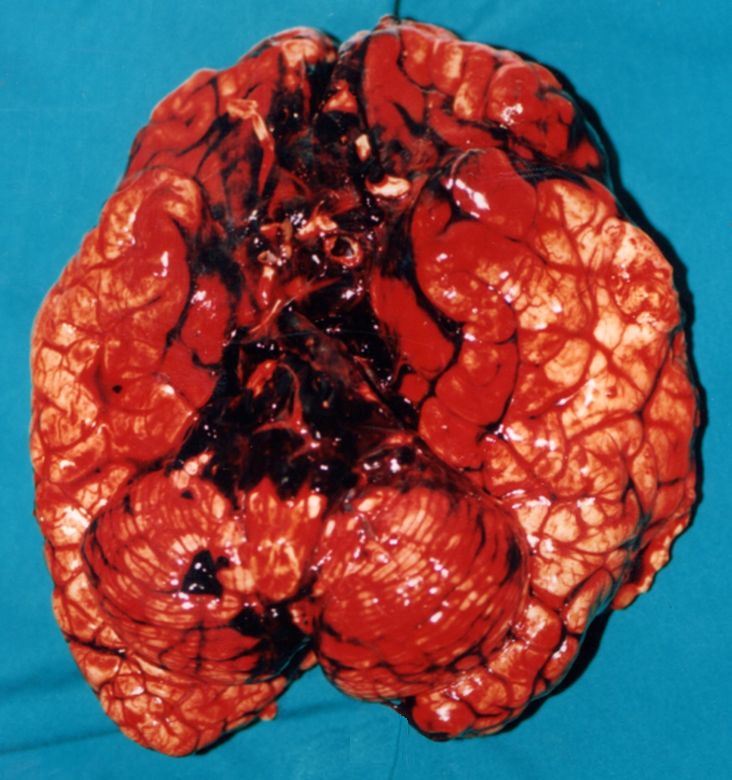
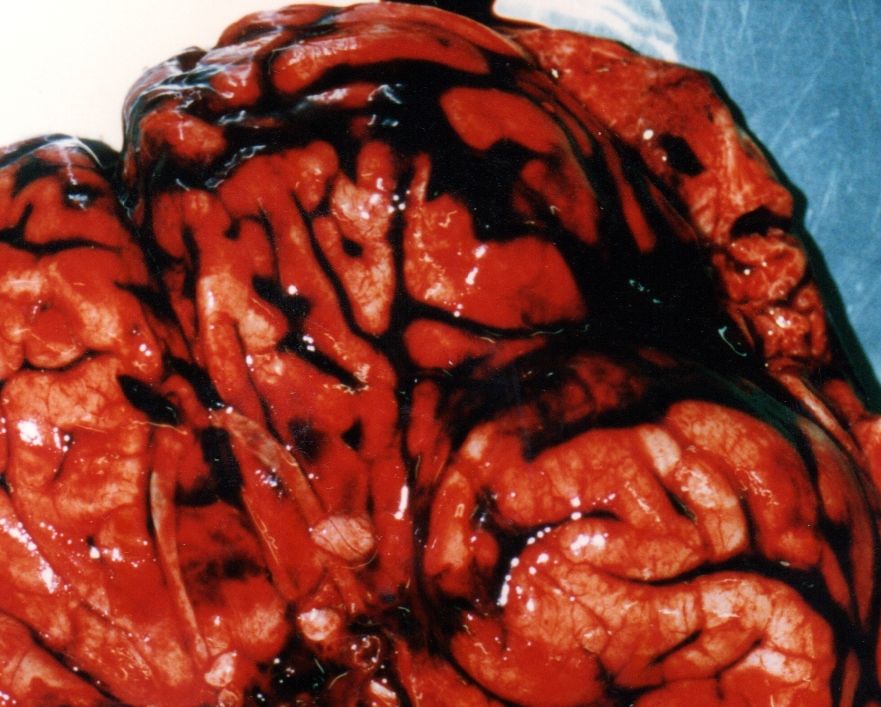
Gross pathology
The following are images associated with gross pathology of cerebral hemorrhage:
References
- ↑ Lee KR, Kawai N, Kim S, Sagher O, Hoff JT (1997). "Mechanisms of edema formation after intracerebral hemorrhage: effects of thrombin on cerebral blood flow, blood-brain barrier permeability, and cell survival in a rat model". J Neurosurg. 86 (2): 272–8. doi:10.3171/jns.1997.86.2.0272. PMID 9010429.
- ↑ Mendelow AD (1993). "Mechanisms of ischemic brain damage with intracerebral hemorrhage". Stroke. 24 (12 Suppl): I115–7, discussion I118-9. PMID 8249006.
- ↑ Folsom AR, Yatsuya H, Mosley TH, Psaty BM, Longstreth WT (2012). "Risk of intraparenchymal hemorrhage with magnetic resonance imaging-defined leukoaraiosis and brain infarcts". Ann Neurol. 71 (4): 552–9. doi:10.1002/ana.22690. PMC 3377969. PMID 22522444.
- ↑ Delgado Almandoz JE, Schaefer PW, Goldstein JN, Rosand J, Lev MH, González RG; et al. (2010). "Practical scoring system for the identification of patients with intracerebral hemorrhage at highest risk of harboring an underlying vascular etiology: the Secondary Intracerebral Hemorrhage Score". AJNR Am J Neuroradiol. 31 (9): 1653–60. doi:10.3174/ajnr.A2156. PMC 3682824. PMID 20581068.
- ↑ Garcia JH, Ho KL (1992). "Pathology of hypertensive arteriopathy". Neurosurg Clin N Am. 3 (3): 497–507. PMID 1633473.
- ↑ Engelhard HH, Andrews CO, Slavin KV, Charbel FT. Current manage- ment of intraventricular hemorrhage. Surg Neurol. 2003;60:15–21.
- ↑ Huttner HB, Hartmann M, Köhrmann M, Neher M, Stippich C, Hähnel S, Kress B. Repeated digital substraction angiography after perimesencephalic subarachnoid hemorrhage? J Neuroradiol. 2006;33:87–89.
- ↑ Altmann-Schneider I, Trompet S, de Craen AJ, van Es AC, Jukema JW, Stott DJ; et al. (2011). "Cerebral microbleeds are predictive of mortality in the elderly". Stroke. 42 (3): 638–44. doi:10.1161/STROKEAHA.110.595611. PMID 21233474.
- ↑ 9.0 9.1 Liu W, Liu R, Sun W, Peng Q, Zhang W, Xu E; et al. (2012). "Different impacts of blood pressure variability on the progression of cerebral microbleeds and white matter lesions". Stroke. 43 (11): 2916–22. doi:10.1161/STROKEAHA.112.658369. PMID 22949472.
- ↑ Poels MM, Ikram MA, van der Lugt A, Hofman A, Krestin GP, Breteler MM; et al. (2011). "Incidence of cerebral microbleeds in the general population: the Rotterdam Scan Study". Stroke. 42 (3): 656–61. doi:10.1161/STROKEAHA.110.607184. PMID 21307170.
- ↑ Klarenbeek P, van Oostenbrugge RJ, Rouhl RP, Knottnerus IL, Staals J (2013). "Higher ambulatory blood pressure relates to new cerebral microbleeds: 2-year follow-up study in lacunar stroke patients". Stroke. 44 (4): 978–83. doi:10.1161/STROKEAHA.111.676619. PMID 23449261.
- ↑ Goos JD, Henneman WJ, Sluimer JD, Vrenken H, Sluimer IC, Barkhof F; et al. (2010). "Incidence of cerebral microbleeds: a longitudinal study in a memory clinic population". Neurology. 74 (24): 1954–60. doi:10.1212/WNL.0b013e3181e396ea. PMID 20548041.
- ↑ Jeerakathil T, Wolf PA, Beiser A, Hald JK, Au R, Kase CS; et al. (2004). "Cerebral microbleeds: prevalence and associations with cardiovascular risk factors in the Framingham Study". Stroke. 35 (8): 1831–5. doi:10.1161/01.STR.0000131809.35202.1b. PMID 15155954.