|
|
| (22 intermediate revisions by 4 users not shown) |
| Line 1: |
Line 1: |
| __NOTOC__ | | __NOTOC__ |
| | {| class="infobox" style="float:right;" |
| | |- |
| | | [[File:Siren.gif|30px|link=Hemolytic anemia resident survival guide]]|| <br> || <br> |
| | | [[Hemolytic anemia resident survival guide|'''Resident'''<br>'''Survival'''<br>'''Guide''']] |
| | |} |
| {{Infobox_Disease | | {{Infobox_Disease |
| | Name = Hemolytic anemia | | | Name = Hemolytic anemia |
| Line 16: |
Line 21: |
| '''For patient information on this, click [[Hemolytic anemia (patient information)|here]]''' | | '''For patient information on this, click [[Hemolytic anemia (patient information)|here]]''' |
|
| |
|
| {{CMG}} | | {{CMG}} {{shyam}} |
|
| |
|
| {{SK}} Haemolytic anaemia | | {{SK}} Haemolytic anaemia |
|
| |
|
| ==Overview== | | ==[[Hemolytic anemia overview|Overview]]== |
| '''Hemolytic anemia''' is [[anemia]] due to [[hemolysis]], the abnormal breakdown of [[red blood cell]]s either in the [[blood vessel]]s (intravascular hemolysis) or elsewhere in the body (extravascular). It has numerous possible causes, ranging from relatively harmless to life-threatening. The general classification of hemolytic anemia is either acquired or inherited. Treatment depends on the cause and nature of the breakdown.
| |
|
| |
|
| In a healthy person, a red blood cell survives 90 to 120 days (on average) in the circulation, so about 1% of human red blood cells break down each day. The [[spleen]] (part of the [[reticulo-endothelial system]]) is the main organ which removes old and damaged RBCs from the circulation. In health the break down and removal of RBCs from the circulation is matched by the production of new RBCs in the [[bone marrow]].
| | ==[[Hemolytic anemia historical perspective|Historical Perspective]]== |
|
| |
|
| When the rate of breakdown increases, the body compensates by producing more RBCs, but if compensation is inadequate clinical problems can appear. Breakdown of RBCs can exceed the rate that the body can make RBCs and so anemia can develop. The breakdown products of [[hemoglobin]] will accumulate in the blood causing [[jaundice]] and be excreted in the urine causing the urine to become dark brown in colour.
| | ==[[Hemolytic anemia classification|Classification]]== |
|
| |
|
| ==Symptoms== | | ==[[Hemolytic anemia pathophysiology|Pathophysiology]]== |
| Signs of [[anemia]] are generally present ([[Fatigue (physical)|fatigue]], later [[heart failure]]). Jaundice may be present.
| |
| *certain aspects of the medical history can suggest a cause for hemolysis (drugs, [[fava bean]] or other sensitivity, [[heart valve prosthesis|prosthetic heart valve]], or another medical illness)
| |
|
| |
|
| Clinical findings in haemolytic anaemias:
| | ==[[Hemolytic anemia causes|Causes]]== |
| # increased serum [[bilirubin]] levels in blood, therefore [[jaundice]]
| |
| # pallor in mucous membrane and skin
| |
| # increased urobilinogen in urine. urine turns dark on standing
| |
| # [[Splenomegaly]]
| |
| # Pigmented [[gallstone]]s may be found
| |
|
| |
|
| ==Tests== | | ==[[Hemolytic anemia epidemiology and demographics|Epidemiology and Demographics]]== |
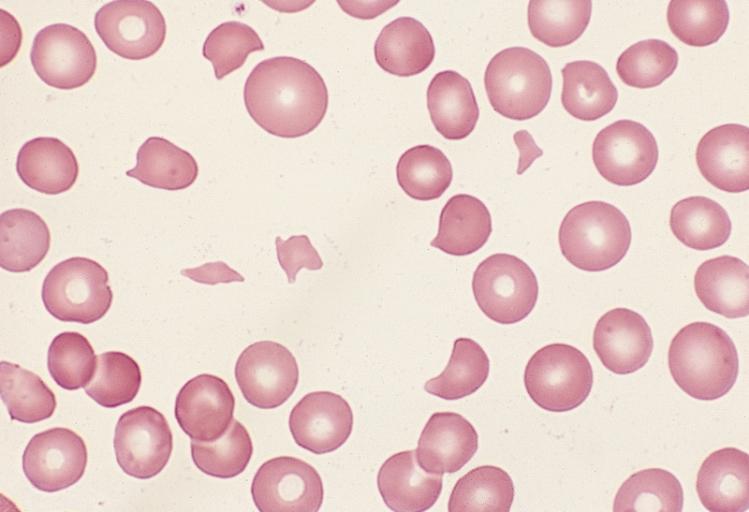
| *[[Peripheral blood smear]] microscopy:
| |
| **fragments of the red blood cells ("[[schistocyte]]s") can be present
| |
| **some red blood cells may appear smaller and rounder than usual ([[spherocyte]]s)
| |
| **[[Reticulocytosis|reticulocytes]] are present in elevated numbers. This may be overlooked if a special [[staining (biology)|stain]] is not used.
| |
| *The level of Unconjugated [[bilirubin]] in the blood is elevated. This may lead to [[jaundice]].
| |
| *The level of [[lactate dehydrogenase]] (LDH) in the blood is elevated
| |
| *[[Haptoglobin]] levels are decreased
| |
| *The direct [[Coombs test]] is positive, if hemolysis is caused by an immune process.
| |
| *Haemosiderin in the urine indicates chronic intravascular haemolysis. There is also urobilinogen in the urine.
| |
|
| |
|
| (Images shown below are courtesy of Melih Aktan MD, Istanbul Medical Faculty - Turkey, and Hospital Universitario La Fe Servicio Hematologia)
| | ==[[Hemolytic anemia risk factors|Risk Factors]]== |
|
| |
|
| <div align="left">
| | ==[[Hemolytic anemia screening|Screening]]== |
| <gallery heights="175" widths="175">
| |
| Image:Microangiopathic hemolytic anemia 0001.jpg|Microangiopathic hemolytic anemia
| |
| Image:Microangiopathic hemolytic anemia 0002.jpg|Microangiopathic hemolytic anemia
| |
| </gallery>
| |
| </div>
| |
|
| |
|
| ==Classification of hemolytic anaemias== | | ==[[Hemolytic anemia differential diagnosis|Differentiating Hemolytic anemia from other Diseases]]== |
| Causes of haemolytic anaemis can be either genetic or acquired.
| |
| ===Genetic===
| |
| *Genetic conditions of RBC membrane
| |
| **[[Hereditary spherocytosis]]
| |
| **[[Hereditary elliptocytosis]]
| |
| *Genetic conditions of RBC metabolism ([[enzyme]] defects)
| |
| **[[Glucose-6-phosphate dehydrogenase deficiency]] (G6PD or favism)
| |
| **[[Pyruvate kinase deficiency]]
| |
| *Genetic conditions of haemoglobin
| |
| **[[Sickle cell anaemia]]
| |
| **[[Thalassaemia]]
| |
| ===Acquired===
| |
| Acquired haemolytic anaemia can be further divided into immune and non-immune mediated.
| |
|
| |
|
| '''Immune mediated hemolytic anaemia''' (direct [[Coombs test]] is positive)
| | ==[[Hemolytic anemia natural history, complications and prognosis|Natural History, Complications and Prognosis]]== |
| *[[Autoimmune hemolytic anemia]]
| |
| **[[Warm antibody autoimmune hemolytic anemia]]
| |
| ***Idiopathic
| |
| ***[[Systemic lupus erythematosus]] (SLE)
| |
| ***[[Evans' syndrome]] (antiplatelet antibodies and haemolytic antibodies)
| |
| **[[Cold agglutinin disease|Cold antibody autoimmune hemolytic anemia]]
| |
| ***[[Idiopathic cold hemagglutinin syndrome]]
| |
| ***[[Infectious mononucleosis]] and mycoplasma ( atypical) pneumonia
| |
| ***[[Paroxysmal cold hemoglobinuria]] (rare)
| |
| *[[Alloimmune]] hemolytic anemia
| |
| **[[Haemolytic disease of the newborn]] (HDN)
| |
| ***[[Rh disease]] (Rh D)
| |
| ***[[ABO hemolytic disease of the newborn]]
| |
| ***[[Anti-Kell hemolytic disease of the newborn]]
| |
| ***[[Rhesus c hemolytic disease of the newborn]]
| |
| ***[[Hemolytic disease of the newborn (anti-RhE)|Rhesus E hemolytic disease of the newborn]]
| |
| ***Other [[Blood type|blood group]] incompatibility (RhC, Rhe, [[Kidd antigen system|Kidd]], [[Duffy antigen|Duffy]], MN, P and others)
| |
| **Alloimmune hemolytic [[Blood transfusion#Complications|blood transfusion]] reactions (ie from a non-compatible [[blood type]])
| |
| *Drug induced immune mediated hemolytic anaemia
| |
| **[[Penicillin]] (high dose)
| |
| **[[Methyldopa]]
| |
|
| |
|
| '''Non-immune mediated haemolytic anaemia''' (direct [[Coombs test]] is negative)
| | ==Diagnosis== |
| *[[Medication|Drugs]] (i.e., some drugs and other ingested substances lead to haemolysis by direct action on RBCs)
| | [[Hemolytic anemia history and symptoms|History and Symptoms]] | [[Hemolytic anemia physical examination|Physical Examination]] | [[Hemolytic anemia laboratory findings|Laboratory Findings]] | [[Hemolytic anemia x ray|X Ray]] | [[Hemolytic anemia CT scan|CT Scan]] | [[Hemolytic anemia MRI scan|MRI Scan]] | [[Hemolytic anemia Echocardiography or ultrasound|Echocardiography or Ultrasound]] | [[Hemolytic anemia imaging findings|Imaging Findings]] | [[Hemolytic anemia Other Imaging Findings|Other imaging findings]] | [[Hemolytic anemia other diagnostic studies|Other Diagnostic Studies]] |
| *[[Toxin]]s (e.g., snake venom)
| |
| *Trauma
| |
| **Mechanical ([[heart valve]]s, extensive vascular surgery, microvascular disease)
| |
| *[[Microangiopathic hemolytic anemia]] (a specific subtype with causes such as TTP, HUS, DIC and HELLP syndrome)
| |
| *Infections
| |
| **[[Malaria]]
| |
| **[[Babesiosis]]
| |
| **[[Septicaemia]]
| |
| *Membrane disorders
| |
| **[[Paroxysmal nocturnal hemoglobinuria]] (rare acquired clonal disorder of red blood cell surface proteins)
| |
| **[[Liver disease]]
| |
|
| |
|
| ==Drug induced hemolysis== | | ==Treatment== |
| Drug induced hemolysis has large clinical relevance. It occurs when drugs actively provoke red cell destruction. Four mechanisms are described below.
| | [[Hemolytic anemia medical therapy|Medical therapy]] | [[Hemolytic anemia surgery|Surgery]] | [[Hemolytic anemia primary prevention|Primary Prevention]] | [[Hemolytic anemia cost-effectiveness of therapy|Cost-Effectiveness of Therapy]] | [[Hemolytic anemia future or investigational therapies|Future or Investigational Therapies]] |
|
| |
|
| ===Immune=== | | ==Case Studies== |
|
| |
|
| [[Penicillin]] in high doses can induce immune mediated hemolysis via the [[hapten]] mechanism in which antibodies are targeted against the combination of penicillin in association with red blood cells. Complement is activated by the attached antibody leading to the removal of red blood cells by the spleen. | | [[Hemolytic anemia case study one|Case #1]] |
|
| |
|
| The drug itself can be targeted by the immune system, e.g. by IgE in a Type I hypersensitivity reaction to penicillin, rarely leading to anaphylaxis.
| |
|
| |
|
| ===Non-immune===
| |
|
| |
| Non-immune drug induced hemolysis can occur via oxidative mechanisms. This is particularly likely to occur when there is an enzyme deficiency in the antioxidant defence system of the red blood cells. An example is where antimalarial oxidant drugs like primaquine damage red blood cells in [[Glucose-6-phosphate dehydrogenase deficiency]] in which the red blood cells are more susceptible to oxidative stress due to reduced NADPH production consequent to the enzyme deficiency.
| |
|
| |
| Some drugs cause RBC (red blood cell) lysis even in normal individuals. These include [[dapsone]] and [[sulfasalazine]].
| |
|
| |
| Non-immune drug-induced hemolysis can also arise from drug-induced damage to cell volume control mechanisms; for example drugs can directly or indirectly impair regulatory volume decrease mechanisms, which become activated during [[hypotonic]] RBC swelling to return the cell to a normal volume. The consequence of the drugs actions are irreversible cell swelling and lysis (e.g. [[ouabain]] at very high doses).
| |
|
| |
| ==Differential diagnosis==
| |
| *'''Ineffective hematopoiesis''' is sometimes misdiagnosed as hemolysis.
| |
| ** Clinically these conditions may share many features of hemolysis
| |
| ** Red cell breakdown occurs before a fully developed red cell is released into the circulation.
| |
| ** Examples: [[thalassemia]], [[myelodysplastic syndrome]]
| |
| * [[Megaloblastic anemia]] due to deficiency in [[vitamin B12]] or [[folic acid]].
| |
|
| |
| ==Therapy==
| |
| Definitive therapy depends on the cause.
| |
|
| |
| *Symptomatic treatment can be given by [[blood transfusion]], if there is marked anaemia.
| |
| *In severe immune-related hemolytic anemia, [[steroid]] therapy is sometimes necessary.
| |
| *Sometimes [[splenectomy]] can be helpful where extravascular heamolysis is predominant (ie most of the red blood cells are being removed by the
| |
| spleen).
| |
|
| |
|
| {{Hematology}} | | {{Hematology}} |