First degree AV block
| First degree AV block | |
 |
|---|
|
First degree AV block Microchapters |
|
Diagnosis |
|---|
|
Treatment |
|
Case Studies |
|
First degree AV block On the Web |
|
American Roentgen Ray Society Images of First degree AV block |
Editor-In-Chief: C. Michael Gibson, M.S., M.D. [1]; Associate Editor(s)-in-Chief: Cafer Zorkun, M.D., Ph.D. [2]
Synonyms and keywords: Prolonged PR; PR prolongation; prolonged PR interval; long PR; PR interval lengthened; first-degree AV block; first-degree AVB; first-degree atrioventricular block
Overview
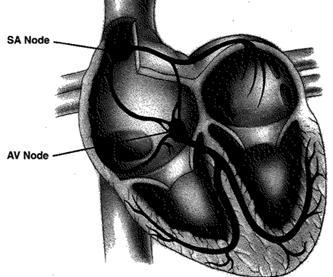
First degree AV block is a disease of the electrical conduction system of the heart in which the PR interval is lengthened or prolonged. In first degree heart block, the disease is almost always at the level of the atrioventricular node (AV node).
Pathophysiology
First degree AV block may be due to conduction delay in the AV node, His-Purkinje system (made up by the bundle of His and the Purkinje fibers), or a combination of the two. The majority of cases are due to a dysfuction of the AV node; however, when first degree heart block coexists with a bundle-branch block, the cause is more likely to be a conduction delay in the His-Purkinje system.
Causes of AV Block
Common Causes of First Degree AV Block
The most common causes of first degree heart block are an AV nodal disease, enhanced vagal tone (for example in athletes), myocarditis, acute myocardial infarction (especially acute inferior MI), electrolyte disturbances and drugs. The drugs that most commonly cause first degree heart block are those that increase the refractory time of the AV node, thereby slowing AV conduction. These include calcium channel blockers, beta-blockers, digitalis, cardiac glycosides and anything that increases cholinergic activity such as cholinesterase inhibitors.
Normal Variants
- PR prolongation can be found in 0.5% of healthy patients.
- Second degree block type I may be seen in healthy patients during sleep.
- Transient AV block can occur with vagal maneuvers.
ST Elevation MI
In acute ST elevation MI:
- First degree block occurs in 8% to 13% of patients.
- Second degree block occurs in 3.5% to 10% of patients.
- Complete heart block occurs in 2.5% to 8% of patients.
Inferior ST Elevation MI
- Inferior ST elevation MI: AV block is more common in patients with inferior MIs (1/3rd of patients).
- In 90% of patients the inferior wall is supplied by the RCA which gives off a branch to the AV node.
- As a rule the AV block is transient and normal function returns within a week of the acute episode.
Anterior ST Elevation MI
- The incidence of second degree AV block and third degree AV block is 5 to 7%.
- Block is the result of damage to the interventricular septum supplied by the LAD
- There is damage to the bundle branches either in the form of bilateral bundle branch block or trifascicular block.
- RBBB, RBBB + LAHB, RBBB + LPHB or LBBB often appear before the development of AV block.
- The PR is normal or minimally prolonged before the onset of second degree AV block or third degree AV block.
- Although the AV block is usually transient, there is a relatively high incidence of recurrence or high-degree AV block after the acute event .
- In addition to ischemia, fibrosis and calcification of the summit of the ventricular septum that involve the branching part of the bundle branches, may play a role in the genesis of the conduction defect.
- It used to be thought that CAD was the most frequent cause of chronic complete AV block, but it actually causes only 15% of cases.
Degenerative Diseases
- Sclerodegenerative disease of the bundle branches first described by Lenegre
- The pathologic process is called idiopathic bilateral bundle branch fibrosis and the heart block is called primary heart block
- This is the most common cause of chronic AV block (46%)
- Lev described similar degenerative lesions, which he referred to as sclerosis of the left side of the cardiac skeleton. There is progressive fibrosis and calcification of the mitral annulus, the central fibrous body, the pars membranacea, the base of the aorta, and the summit of the muscular ventricular septum. Various portions of the His bundle or the bundle branches may be involved, resulting in AV block.
Hypertension
- Chronic AV block in patients with HTN is thought to be due to CAD or sclerosis of the left side of the cardiac skeleton exacerbated by hypertension
Diseases of the Myocardium
- Acute rheumatic fever: PR prolongation is a common (25 to 95% of cases) sign in patients with acute rheumatic fever
- Type I second degree AV block may occur, but complete AV block is uncommon
- usually transient, disappears when the patient recovers
- Amyloidosis
- Ankylosing spondylitis
- Chagas disease
- Dermatomyositis
- Dilated cardiomyopathy results in various degrees of heart block are seen in 15% of patients
- Diphtheria
- HCM: 3% of patients with HCM will develop heart block
- Hemochromatosis
- Lyme disease
- Muscular dystrophy
- Myocarditis
- Sarcoid
- Scleroderma
- SLE
- Tumors, primary and secondary
Valvular Heart Disease
- Calcific aortic stenosis may be accompanied by chronic partial or complete AV block
- There is an extension of the calcification to involve the main bundle or its bifurcation, resulting in degeneration and necrosis of the conduction tissue
- May also occur in rheumatic mitral valve disease, but is less common
- Occasionally, massive calcification of the mitral annulus as an aging process may cause AV block
- May also be seen in bacterial endocarditis, especially of the aortic valve
- Ebstein's anomaly may be associated with first-degree AV block.
Drugs
- When second degree AV block is induced, it is always of the Type I variety
- When complete block occurs, the QRS complexes are narrow because the block is of the AV node
- The ventricular response rate is more rapid than that due to organic lesions, and increased automaticity of the AV junctional pacemaker may be responsible.
- Quinidine and Procainamide may produce slight prolongation of the PR
- β blockers may cause AV block
- Diltiazem and verapamil may cause AV conduction delay and PR interval prolongation
Congenital
- Occurs in the absence of other evidence of organic heart disease
- Site is usually proximal to the bifurcation of the His bundle, most often in the AV node
- Narrow QRS with a rate > 40 beats per minute
- Frequently seen in those with corrected transposition of the great vessels, and occasionally in ASDs and Ebstein's anomaly
Trauma
- May be induced during open heart surgery in the area of AV conduction tissue
- Seen in patients operated on for the correction of VSD, tetralogy of Fallot, and endocardial cushion defect.
- May be due to edema, transient ischemia, or actual disruption of the conduction tissue. The block may therefore be permanent or transient.
- Also reported with both penetrating and non-penetrating trauma of the chest
Epidemiology and Demographics
Incidence
The incidence of first degree AV block is 13 per 100,000 persons.
Prevalence
First degree AV block has a prevalence in the normal (young adult) population of 65-110 per 100,000.
Natural History, Complications and Prognosis
Natural History
Isolated first degree heart block has few if any clinical consequences. There are no symptoms or signs associated with it, and there is little danger of progression to complete heart block.
Complications
Individuals who have first degree block as part of a triad of first degree heart block, right bundle branch block, and either left anterior fascicular block or left posterior fascicular block (known as trifascicular block) may be at an increased risk of progression to complete heart block.
Diagnosis
In normal individuals, the AV node slows the conduction of electrical impulse through the heart. This is manifest on a surface EKG as the PR interval. The normal PR interval is from 120 milliseconds (ms) to 200 milliseconds (ms) in duration. This is measured from the initial deflection of the P wave to the beginning of the QRS complex.
In first degree heart block, the diseased AV node conducts the electrical activity slower. This is seen as a PR interval greater than 200 milliseconds (ms) in length on the surface EKG. It is usually an incidental finding on a routine EKG.
First degree heart block does not require any particular evaluation except for electrolyte and drug screens especially if an overdose is suspected.
Electrocardiographic Findings
- PR interval is greater than 0.20 seconds = 200 miliseconds
- Each P wave is followed by a QRS
- Range of PR interval is between 0.21 and 0.40 seconds
- P wave may be mistaken for a T wave or a U wave
- The PR interval is more variable in those without heart disease
- In patients with a narrow QRS, His-Bundle recordings show that the conduction delay is in the AV node, with prolongation of the atrial His (AH) time, rarely is a prolonged His ventricular (HV) time responsible.
- In patients with PR prolongation and QRS prolongation, then the conduction delay may occur in various regions of the conduction system
EKG Examples
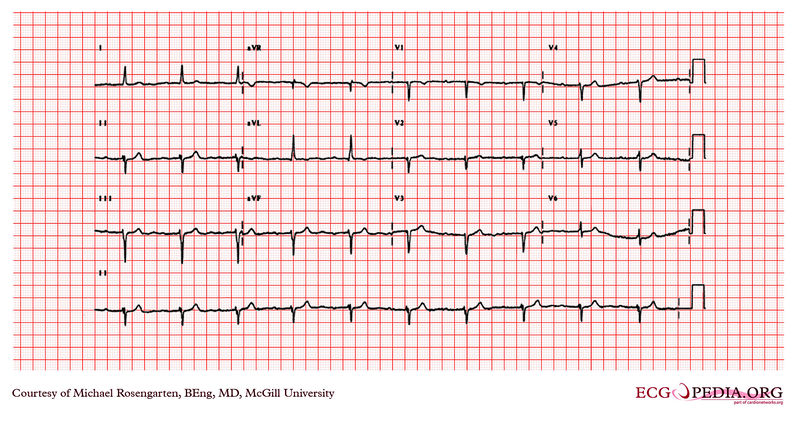
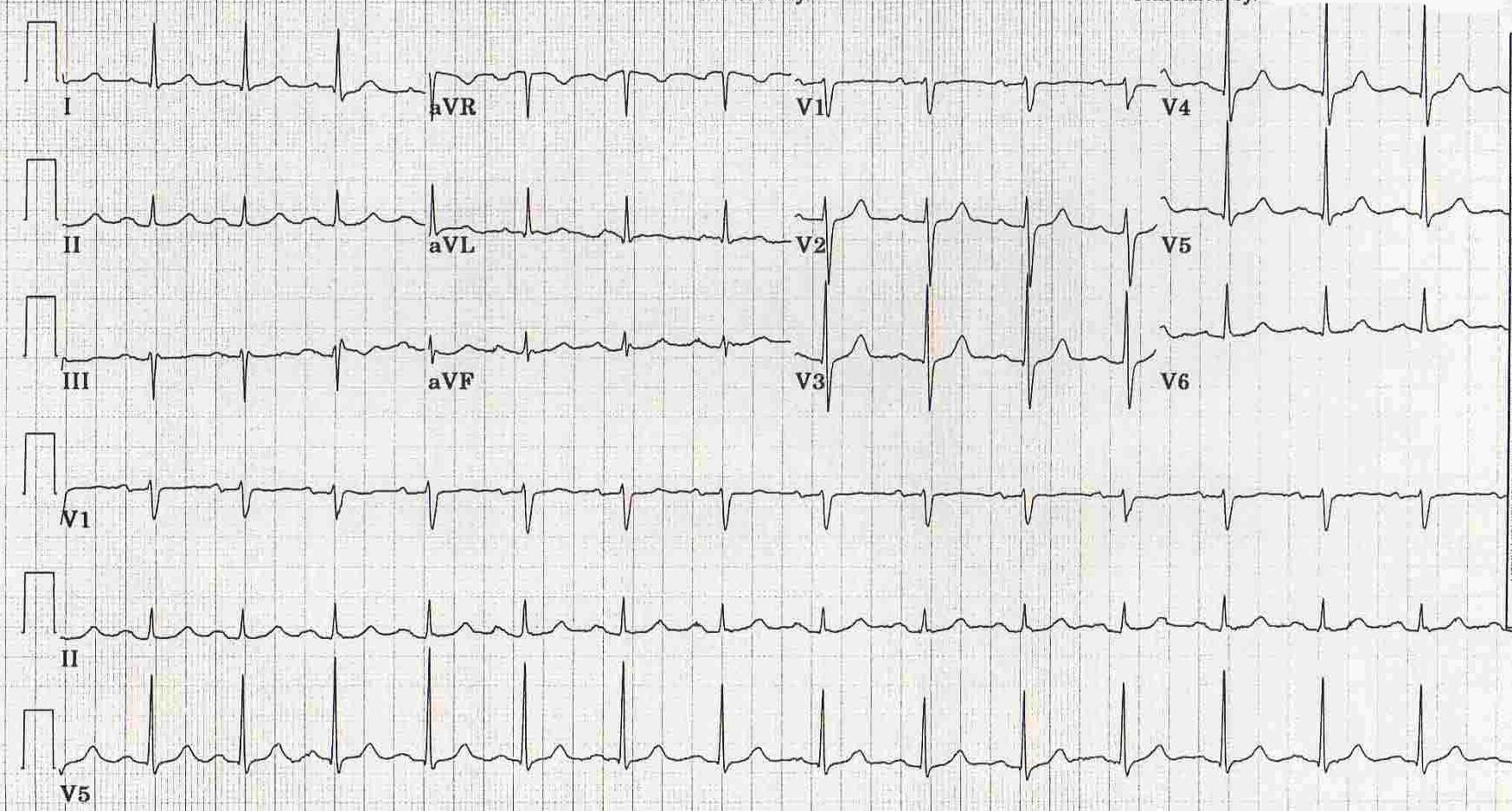
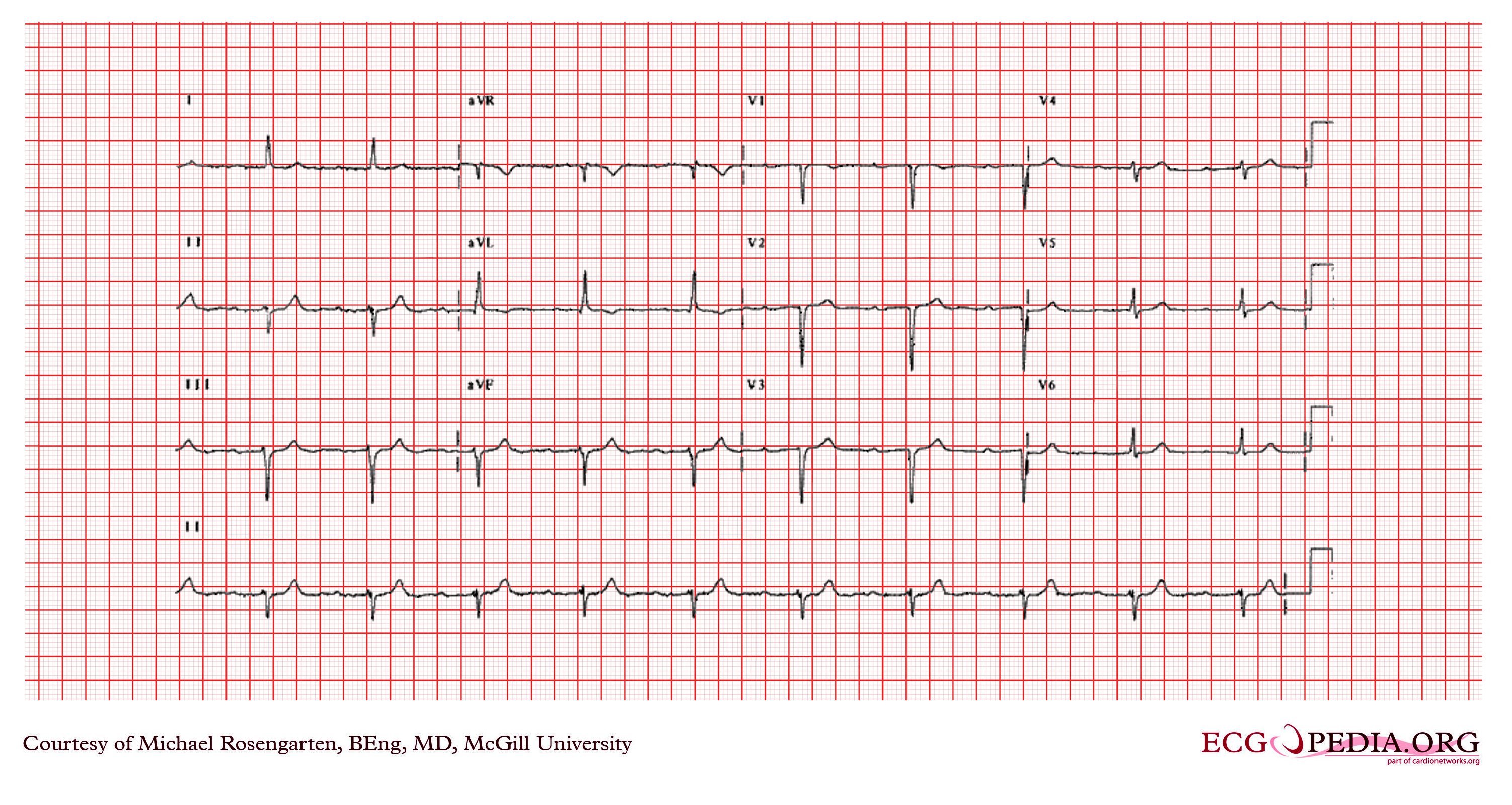
Shown below is an image of an electrocardiogram of a 64 year-old man with a history of coronary artery disease. The patient was taking amiodarone, metoprolol, and Vasotec at the time of this recording. This was a routine recording. The electrocardiogram shows sinus rhythm with a prolonged P wave > 120 milliseconds. The P wave is notched in the inferior leads. This is consistent with a left atrial abnormality. The PR interval is long at 200 milliseconds and is diagnostic of first-degree heart block. The Q waves in the inferior leads suggest an inferior wall infarction.
Copyleft image obtained courtesy of ECGpedia, http://en.ecgpedia.org/wiki/Main_Page
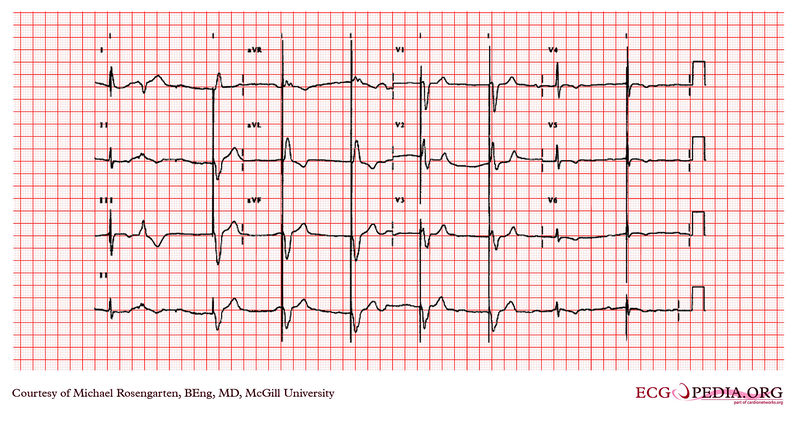
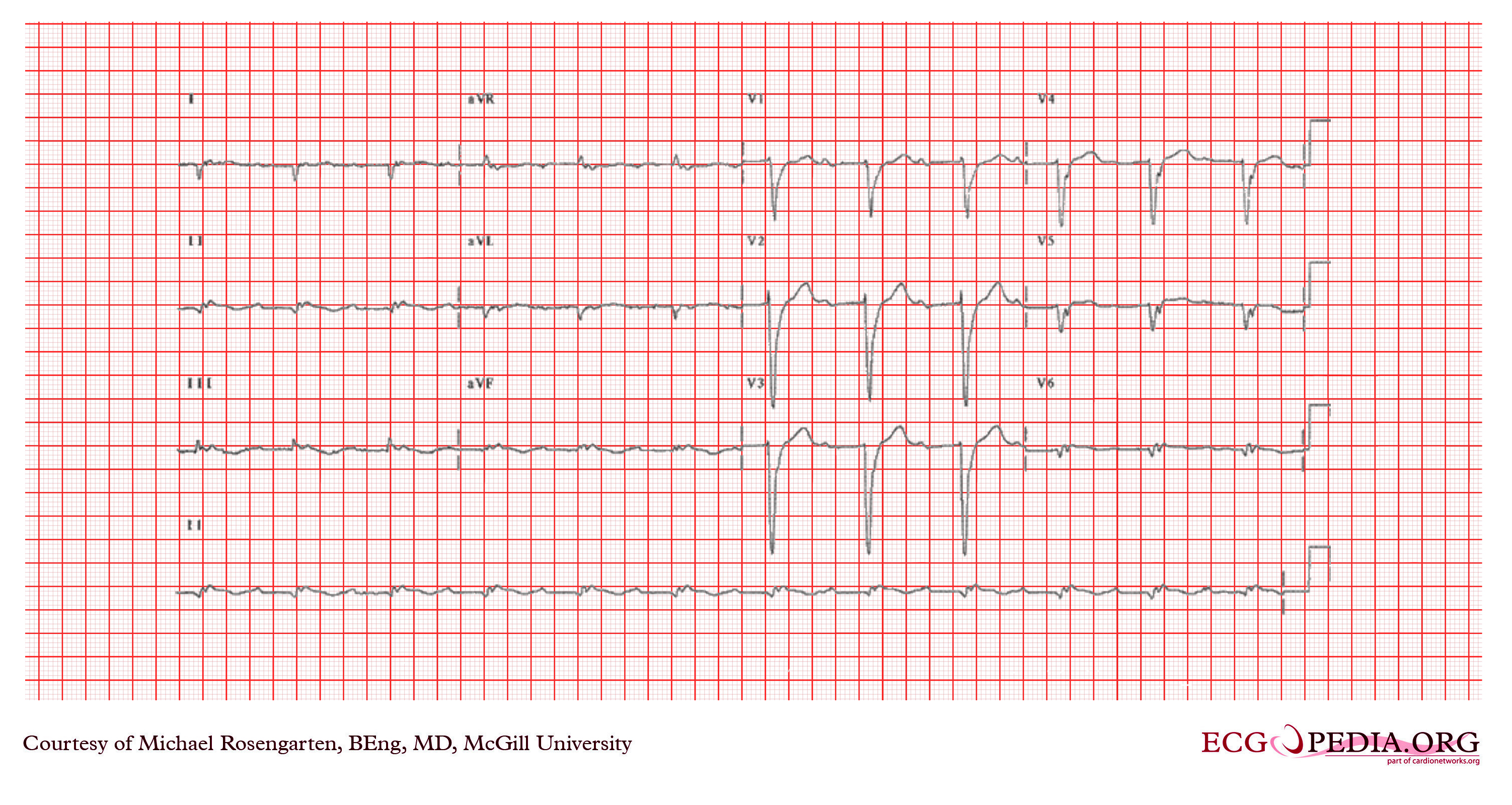
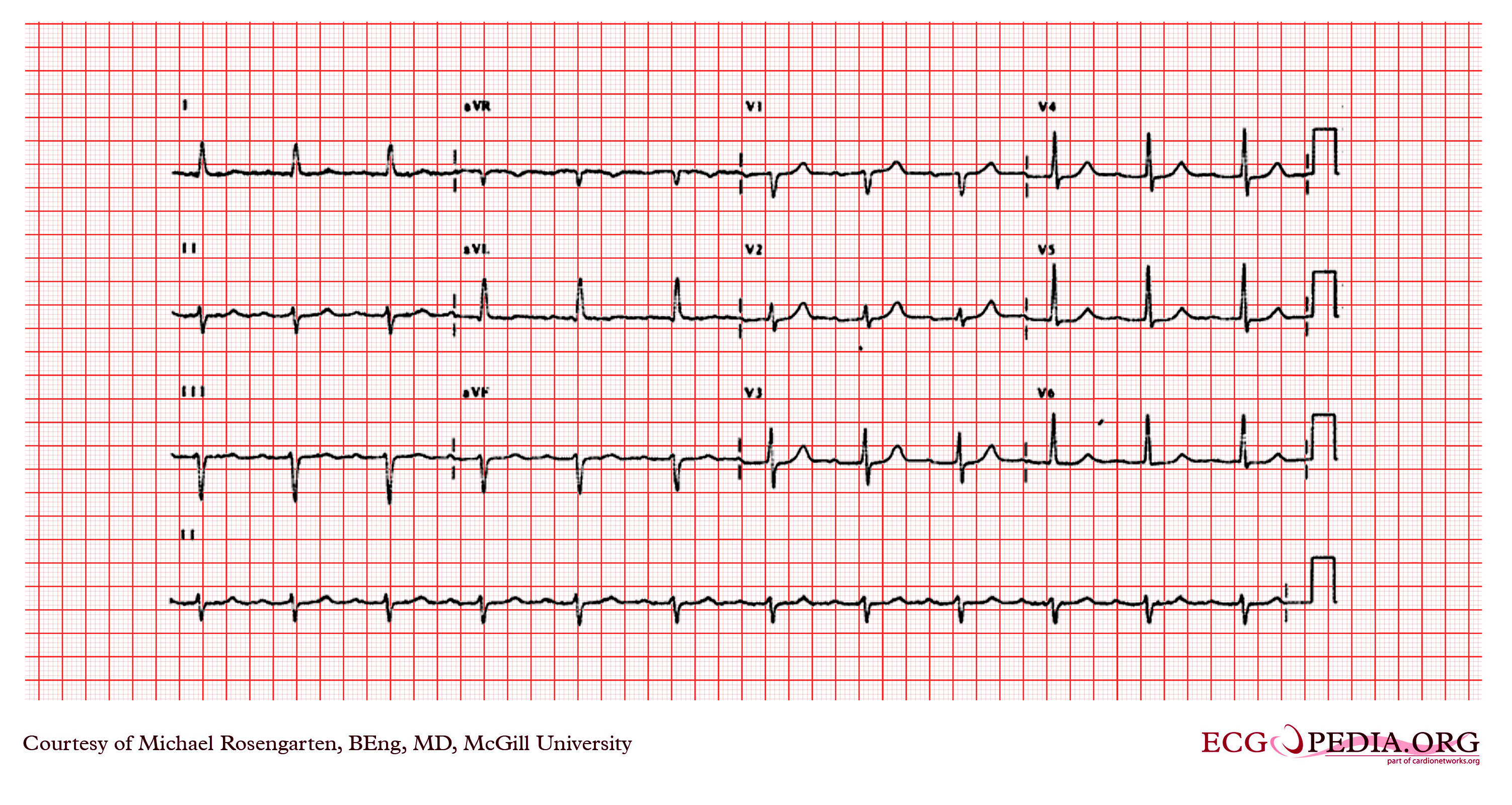
Shown below is the electrocardiogram of a 77 year old man with a history of coronary artery disease. He was taking Monopril, metoprolol, ASA and Hytrin. The electrocardiogram shows sinus rhythm with a marked first degree heart block ( about 360ms). There is also a poor R wave progression across the precordial leads and a Q wave in V2 suggestive of a previous anterior wall infarction. The QRS also has a left axis deviation best described as a left anterior hemi-block.
Copyleft image obtained courtesy of ECGpedia, http://en.ecgpedia.org/wiki/Main_Page
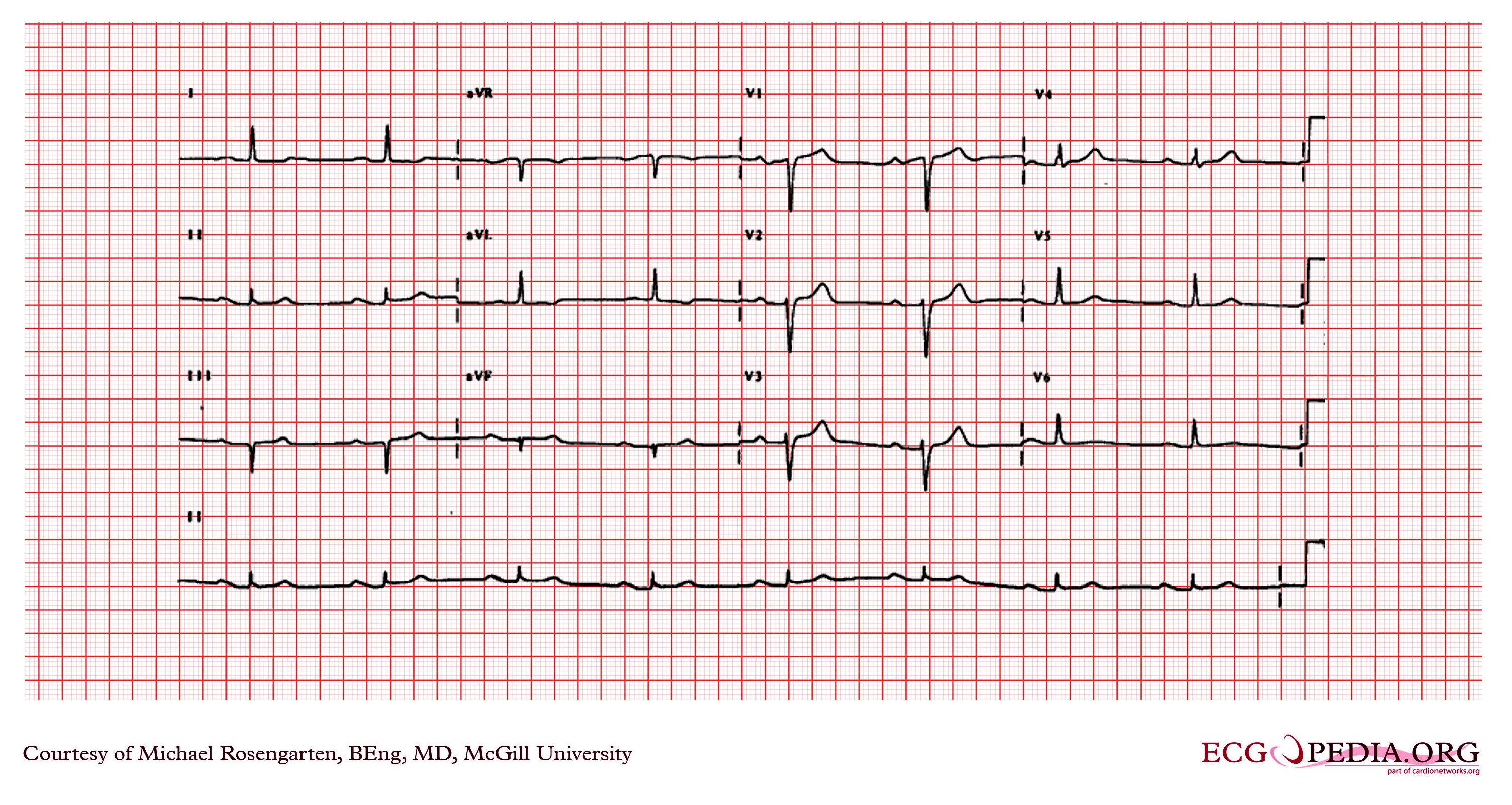
Shown below is an electrocardiogram from a 87 year old man with a history of atrial fibrillation. His medications were coumadin and Monopril. The cardiogram shows sinus rhythm with rate of about 50/min, and a marked first degree heart block with a pr interval of about 350ms.
The first complex on the left is a fusion between the patient's native QRS and the pacemaker spike (this is normal operation) this is followed by a PVC. Note the small blip following the PVC is artifact and is not a failure to capture of the pacemaker. The pacemaker is working well as a VVI pacer set at 50/min. The large spikes suggest a unipolar lead.
Copyleft image obtained courtesy of ECGpedia, http://en.ecgpedia.org/wiki/Main_Page
Shown below is an electrocardiogram demonstrating sinus rhythm with first degree heart block (PR segment > 200ms.) Note the P waves in the inferior leads are greater than 120 ms. in duration, which suggests left atrial abnormality.
Copyleft image obtained courtesy of ECGpedia, http://en.ecgpedia.org/wiki/Main_Page
Shown below is an electrocardiogram with a sinus rhythm. The PR interval is prolonged (>200ms) and the QRS is a left ward axis (<-30 degrees). The EKG shows a first degree heart block and a left anterior fascicular block.

Copyleft image obtained courtesy of ECGpedia, http://en.ecgpedia.org/wiki/Main_Page
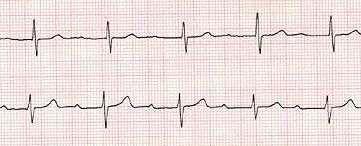
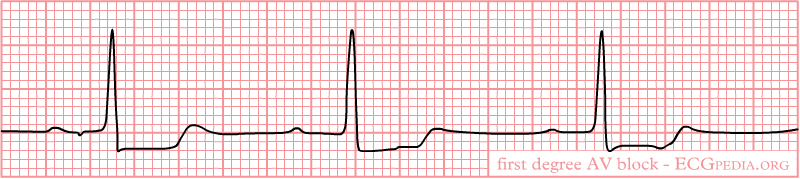
Shown below is an electrocardiogram of first degree AV block with increased PR interval.
Copyleft image obtained courtesy of ECGpedia, http://en.ecgpedia.org/wiki/Main_Page
Shown below is an electrocardiogram of first degree AV block with increased PR interval.
Copyleft image obtained courtesy of ECGpedia, http://en.ecgpedia.org/wiki/Main_Page
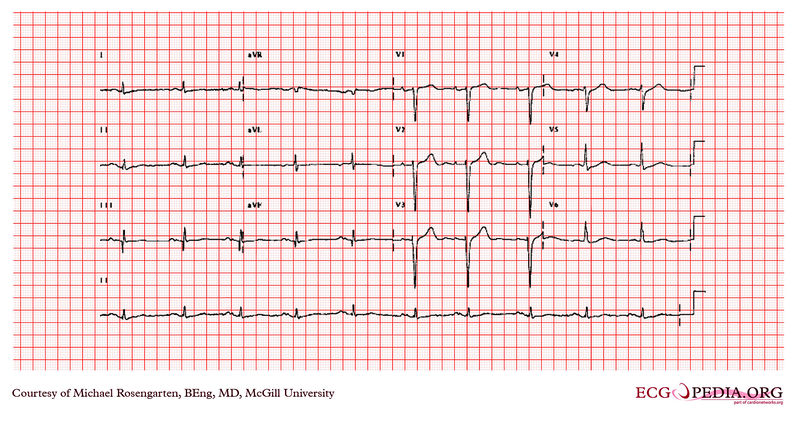
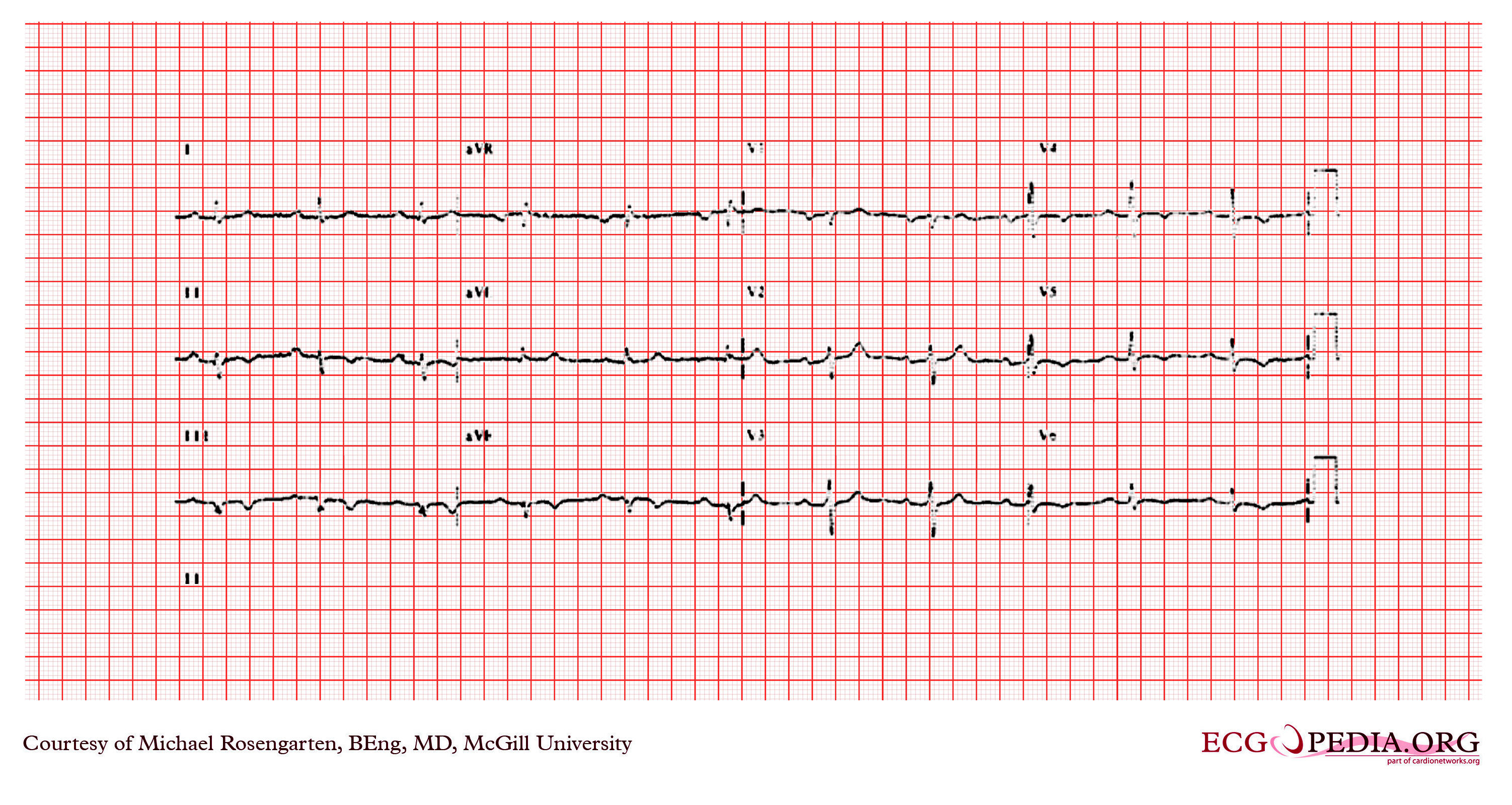
Shown below is an electrocardiogram demonstrating a regular rhythm at a rate of 65/min. The PR interval is 400 ms, the QRS is approximately 110 ms, and there are Qs waves in I, II, aVL, and poor R waves in the precordial leads. This is sinus rhythm with a marked first degree heart block. The QRS suggests an extensive anterior/lateral myocardial infarction.
Copyleft image obtained courtesy of ECGpedia, http://en.ecgpedia.org/wiki/Main_Page
Shown below is an electrocardiogram with sinus rhythm and a marked first degree heart block. In this case the PR interval is about 400 ms. A Holter monitor showed second degree but not third degree A/V block.

Copyleft image obtained courtesy of ECGpedia, http://en.ecgpedia.org/wiki/Main_Page
Shown below is an electrocardiogram with a first degree AV block
Copyleft image obtained courtesy of ECGpedia, http://en.ecgpedia.org/wiki/Main_Page
Shown below is an electrocardiogram depicting sinus rhythm with a first degree A/V block (>200ms). There is terminal P wave negativity in V1 suggestive of left atrial abnormality. There is left anterior fascicular block (axis < -30 degrees). The ST segment is slightly elevated in leads II and aVF with T wave inversion suggesting inferior ischemia or infarction.
Copyleft image obtained courtesy of ECGpedia, http://en.ecgpedia.org/wiki/Main_Page
Shown below is an electrocardiogram depicting a first degree heart block with a left anterior hemi-block.
Copyleft image obtained courtesy of ECGpedia, http://en.ecgpedia.org/wiki/Main_Page
Shown below is an electrocardiogram depicting sinus rhythm with a prolonged PR interval (>120ms.) which is first degree A/V block. There is also a left axis deviation (axis between -30 and -90 degrees) with R waves in the inferior leads. This axis deviation is consitent with a left anterior fasicular block.
Copyleft image obtained courtesy of ECGpedia, http://en.ecgpedia.org/wiki/Main_Page
Treatment
- Correction of reversible causes of the block such as ischemia, medications, electrolyte imbalances, and vagotonic conditions should be considered.
- Treatment in emergency situations are atropine and an external pacer.
- Implantation of permanent pacemakers is not usually indicated in first degree heart block.
- This condition does not require admission unless there is an associated myocardial infarction. Even though it usually does not progress to higher forms of heart block, it may require outpatient follow up and monitoring of the EKG especially if there is an associated bundle branch block.
- There are some special situations in which placement of a permanent pacemaker is indicated in first degree heart blocks.
- Special situations when placement of permanent pacemakers is indicated in first degree heart block are: pacemaker syndrome (loss of atrioventricular synchrony) and in some neuromuscular conditions associated with first degree heart block such as myotonic muscular dystrophy, Kearns-Sayre syndrome, Erb's dystrophy (limb-girdle), and peroneal muscular atrophy)
- A dual chamber DDD pacemaker is preferred over a single chambered VVI pacemakers as it maintains physiologic AV synchrony. A dual-chamber artificial pacemaker is a type of device that typically listens for a pulse from the SA node and sends a pulse to the AV node at an appropriate interval, essentially completing the connection between the two nodes. Pacemakers in this role are usually programmed to enforce a minimum heart rate.