Filgrastim: Difference between revisions
No edit summary |
No edit summary |
||
| Line 25: | Line 25: | ||
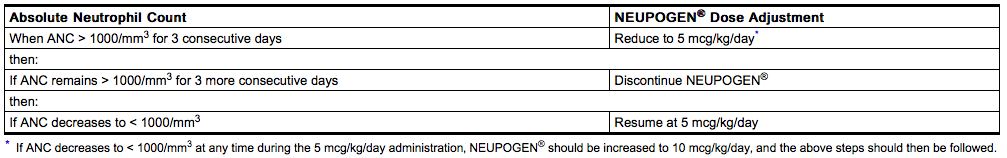
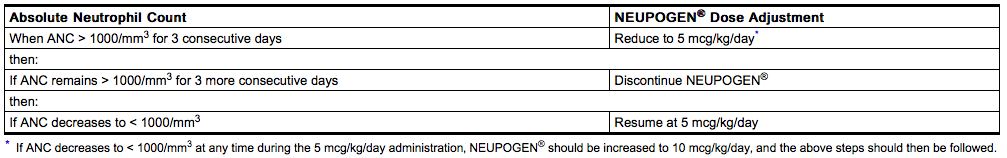
During the period of neutrophil recovery‚ the daily dose of NEUPOGEN® should be titrated against the neutrophil response as follows: | During the period of neutrophil recovery‚ the daily dose of NEUPOGEN® should be titrated against the neutrophil response as follows: | ||
[[File:Filgrastim_administration_01 | [[File:Filgrastim_administration_01.png|thumb|none|400px|This image is provided by the National Library of Medicine.]] | ||
<h4>Peripheral Blood Progenitor Cell Collection and Therapy in Cancer Patients</h4> | <h4>Peripheral Blood Progenitor Cell Collection and Therapy in Cancer Patients</h4> | ||
| Line 49: | Line 49: | ||
If required‚ NEUPOGEN® may be diluted in 5% dextrose. NEUPOGEN® diluted to concentrations between 5 and 15 mcg/mL should be protected from adsorption to plastic materials by the addition of Albumin (Human) to a final concentration of 2 mg/mL. When diluted in 5% dextrose or 5% dextrose plus Albumin (Human)‚ NEUPOGEN® is compatible with glass bottles‚ PVC and polyolefin IV bags‚ and polypropylene syringes. | If required‚ NEUPOGEN® may be diluted in 5% dextrose. NEUPOGEN® diluted to concentrations between 5 and 15 mcg/mL should be protected from adsorption to plastic materials by the addition of Albumin (Human) to a final concentration of 2 mg/mL. When diluted in 5% dextrose or 5% dextrose plus Albumin (Human)‚ NEUPOGEN® is compatible with glass bottles‚ PVC and polyolefin IV bags‚ and polypropylene syringes. | ||
Dilution of NEUPOGEN® to a final concentration of less than 5 mcg/mL is not recommended at any time. Do not dilute with saline at any time; product may precipitate. | Dilution of NEUPOGEN® to a final concentration of less than 5 mcg/mL is not recommended at any time. Do not dilute with saline at any time; product may precipitate. | ||
|offLabelAdultGuideSupport=<h4>[[Myelodysplastic syndrome]]</h4> | |||
* Developed by: [[American Society of Clinical Oncology|American Society of Clinical Oncology (ASCO)]] | |||
* Class of Recommendation: Not applicable | |||
* Level of Evidence: Not applicable | |||
* Dosing Information | |||
:* Intermittent CSF use may be considered in patients with severe neutropenia and recurrent infections. | |||
<h4>Cancer Patients Receiving [[Myelosuppressive Chemotherapy]]</h4> | |||
* Dosing information | |||
:* Recommended starting dosage: '''5 mcg/kg/day'''‚ administered as a single daily injection by SC bolus injection‚ by short IV infusion (15 to 30 minutes)‚ or by continuous SC or continuous IV infusion. | |||
::* A CBC and platelet count should be obtained before instituting NEUPOGEN® therapy and monitored twice weekly during therapy. | |||
::* Doses may be increased in increments of '''5 mcg/kg''' for each chemotherapy cycle‚ according to the duration and severity of the ANC nadir. | |||
:* NEUPOGEN® should be administered no earlier than 24 hours after the administration of cytotoxic chemotherapy. | |||
:* NEUPOGEN® should not be administered in the period 24 hours before the administration of chemotherapy. | |||
:* NEUPOGEN® should be administered daily for up to 2 weeks‚ until the ANC has reached 10‚000/mm3 following the expected chemotherapy-induced neutrophil nadir. | |||
:* The duration of NEUPOGEN® therapy needed to attenuate chemotherapy-induced neutropenia may be dependent on the myelosuppressive potential of the chemotherapy regimen employed. | |||
:* NEUPOGEN® therapy should be discontinued if the ANC surpasses 10‚000/mm3 after the expected chemotherapy-induced neutrophil nadir. | |||
|offLabelAdultNoGuideSupport=<h4>[[Agranulocytosis]]</h4> | |offLabelAdultNoGuideSupport=<h4>[[Agranulocytosis]]</h4> | ||
| Line 73: | Line 94: | ||
* Dosing information | * Dosing information | ||
:* '''100mcg/m(2) to 400 mcg/m(2)''' 10071455 | :* '''100mcg/m(2) to 400 mcg/m(2)''' 10071455 | ||
:* | |||
<h4>Infectious disease</h4> | |||
* Dosing information | |||
:* '''300 micrograms/day (mcg/day) subcutaneously to 480 mcg/day'''10803937 | |||
<h4>[[Leukemia]]</h4> | |||
* Dosing information | |||
:* '''5 micrograms/kilogram/day'''11426551 | |||
<h4>[[Mucositis]] following chemotherapy</h4> | |||
* Dosing information | |||
:* '''120 mcg (0.4 mL)'''9827976 | |||
|fdaLIADPed=<h4>Cancer Patients Receiving [[Myelosuppressive Chemotherapy]]</h4> | |||
* Dosing information | |||
:* Recommended starting dosage: '''5 mcg/kg/day'''‚ administered as a single daily injection by SC bolus injection‚ by short IV infusion (15 to 30 minutes)‚ or by continuous SC or continuous IV infusion. | |||
::* A CBC and platelet count should be obtained before instituting NEUPOGEN® therapy and monitored twice weekly during therapy. | |||
::* Doses may be increased in increments of '''5 mcg/kg''' for each chemotherapy cycle‚ according to the duration and severity of the ANC nadir. | |||
:* NEUPOGEN® should be administered no earlier than 24 hours after the administration of cytotoxic chemotherapy. | |||
:* NEUPOGEN® should not be administered in the period 24 hours before the administration of chemotherapy. | |||
:* NEUPOGEN® should be administered daily for up to 2 weeks‚ until the ANC has reached 10‚000/mm3 following the expected chemotherapy-induced neutrophil nadir. | |||
:* The duration of NEUPOGEN® therapy needed to attenuate chemotherapy-induced neutropenia may be dependent on the myelosuppressive potential of the chemotherapy regimen employed. | |||
:* NEUPOGEN® therapy should be discontinued if the ANC surpasses 10‚000/mm3 after the expected chemotherapy-induced neutrophil nadir. | |||
<h4>Cancer Patients Receiving [[Bone Marrow Transplant]]</h4> | |||
* Dosing information | |||
:* Recommended dosage following BMT: '''10 mcg/kg/day''' given as an IV infusion of 4 or 24 hours‚ or as a continuous 24-hour SC infusion. For patients receiving BMT‚ the first dose of NEUPOGEN® should be administered at least 24 hours after cytotoxic chemotherapy and at least 24 hours after bone marrow infusion. | |||
During the period of neutrophil recovery‚ the daily dose of NEUPOGEN® should be titrated against the neutrophil response as follows: | |||
[[File:Filgrastim_administration_01.png|thumb|none|400px|This image is provided by the National Library of Medicine.]] | |||
<h4>Peripheral Blood Progenitor Cell Collection and Therapy in Cancer Patients</h4> | |||
* Dosing information | |||
:* Recommended dosage for the mobilization of PBPC: '''10 mcg/kg/day SC'''‚ either as a bolus or a continuous infusion. It is recommended that NEUPOGEN® be given for at least 4 days before the first leukapheresis procedure and continued until the last leukapheresis. Although the optimal duration of NEUPOGEN® administration and leukapheresis schedule have not been established‚ administration of NEUPOGEN® for 6 to 7 days with leukaphereses on days 5‚ 6‚ and 7 was found to be safe and effective. Neutrophil counts should be monitored after 4 days of NEUPOGEN®, and NEUPOGEN® dose modification should be considered for those patients who develop a WBC count > 100‚000/mm3. | |||
In all clinical trials of NEUPOGEN® for the mobilization of PBPC‚ NEUPOGEN® was also administered after reinfusion of the collected cells. | |||
<h4>Patients With [[Severe Chronic Neutropenia]]</h4> | |||
* Dosing information | |||
:* NEUPOGEN® should be administered to those patients in whom a diagnosis of [[congenital]]‚ [[cyclic]]‚ or [[idiopathic neutropenia]] has been definitively confirmed. Other diseases associated with [[neutropenia]] should be ruled out. | |||
:* Starting Dose: | |||
::* [[Congenital Neutropenia]]: The recommended daily starting dose is '''6 mcg/kg BID SC''' every day. | |||
::* Idiopathic or [[Cyclic Neutropenia]]: The recommended daily starting dose is '''5 mcg/kg injection SC qd'''. | |||
:* Dose Adjustments: | |||
::* Chronic daily administration is required to maintain clinical benefit. Absolute neutrophil count should not be used as the sole indication of efficacy. The dose should be individually adjusted based on the patient's clinical course as well as ANC. In the SCN postmarketing surveillance study, the reported median daily doses of NEUPOGEN® were: '''6.0 mcg/kg''' (congenital neutropenia), '''2.1 mcg/kg''' ([[cyclic neutropenia]]), and '''1.2 mcg/kg''' ([[idiopathic neutropenia]]). In rare instances, patients with congenital neutropenia have required doses of NEUPOGEN® ≥ 100 mcg/kg/day. | |||
<u>Dilution</u> | |||
If required‚ NEUPOGEN® may be diluted in 5% dextrose. NEUPOGEN® diluted to concentrations between 5 and 15 mcg/mL should be protected from adsorption to plastic materials by the addition of Albumin (Human) to a final concentration of 2 mg/mL. When diluted in 5% dextrose or 5% dextrose plus Albumin (Human)‚ NEUPOGEN® is compatible with glass bottles‚ PVC and polyolefin IV bags‚ and polypropylene syringes. | |||
Dilution of NEUPOGEN® to a final concentration of less than 5 mcg/mL is not recommended at any time. Do not dilute with saline at any time; product may precipitate. | |||
|offLabelPedGuideSupport=There is limited information regarding <i>Off-Label Guideline-Supported Use</i> of Filgrastim in pediatric patients. | |offLabelPedGuideSupport=There is limited information regarding <i>Off-Label Guideline-Supported Use</i> of Filgrastim in pediatric patients. | ||
|offLabelPedNoGuideSupport=<h4>[[Aplastic anemia]]</h4> | |offLabelPedNoGuideSupport=<h4>[[Aplastic anemia]]</h4> | ||
| Line 79: | Line 158: | ||
* Dosing information | * Dosing information | ||
:* Not applicable 10979946 | :* Not applicable 10979946 | ||
<h4>[[Neutropenia]] - Pre-[[eclampsia]]</h4> | |||
* Dosing information | |||
:* '''5 or 10 micrograms/kilogram (mcg/kg)/day'''9794941 | |||
<h4>[[Septicemia]] of newborn</h4> | |||
* Dosing information | |||
:* Not applicable 11391341 | |||
<h4>[[Shwachman syndrome]]</h4> | |||
* Dosing information | |||
:* Not applicable 1700246 | |||
|contraindications=NEUPOGEN® is contraindicated in patients with known [[hypersensitivity]] to E coli-derived proteins‚ filgrastim‚ or any component of the product. | |||
|warnings='''<i>Allergic Reactions</i>''' | |||
Allergic-type reactions occurring on initial or subsequent treatment have been reported in < 1 in 4000 patients treated with NEUPOGEN®. These have generally been characterized by systemic symptoms involving at least two body systems‚ most often skin (rash‚ urticaria‚ facial edema)‚ respiratory (wheezing‚ dyspnea)‚ and cardiovascular (hypotension‚ tachycardia). Some reactions occurred on initial exposure. Reactions tended to occur within the first 30 minutes after administration and appeared to occur more frequently in patients receiving NEUPOGEN® IV. Rapid resolution of symptoms occurred in most cases after administration of antihistamines‚ steroids‚ bronchodilators‚ and/or epinephrine. Symptoms recurred in more than half the patients who were rechallenged. | |||
'''<i>[[SPLENIC RUPTURE]]</i>''' | |||
'''SPLENIC RUPTURE, INCLUDING FATAL CASES, HAS BEEN REPORTED FOLLOWING THE ADMINISTRATION OF NEUPOGEN®. INDIVIDUALS RECEIVING NEUPOGEN® WHO REPORT LEFT UPPER ABDOMINAL AND/OR SHOULDER TIP PAIN SHOULD BE EVALUATED FOR AN ENLARGED SPLEEN OR SPLENIC RUPTURE.''' | |||
'''<i>[[Acute Respiratory Distress Syndrome]] (ARDS)</i>''' | |||
Acute respiratory distress syndrome (ARDS) has been reported in patients receiving NEUPOGEN®, and is postulated to be secondary to an influx of neutrophils to sites of inflammation in the lungs. Patients receiving NEUPOGEN® who develop fever, lung infiltrates, or respiratory distress should be evaluated for the possibility of ARDS. In the event that ARDS occurs, NEUPOGEN® should be withheld until resolution of ARDS or discontinued. Patients should receive appropriate medical management for this condition. | |||
'''<i>[[Alveolar Hemorrhage]] and [[Hemoptysis]]</i>''' | |||
Alveolar hemorrhage manifesting as pulmonary infiltrates and hemoptysis requiring hospitalization has been reported in healthy donors undergoing PBPC mobilization. Hemoptysis resolved with discontinuation of NEUPOGEN®. The use of NEUPOGEN® for PBPC mobilization in healthy donors is not an approved indication. | |||
'''<i>[[Sickle Cell Disorders]]</i>''' | |||
Severe sickle cell crises, in some cases resulting in death, have been associated with the use of NEUPOGEN® in patients with sickle cell disorders. Only physicians qualified by specialized training or experience in the treatment of patients with sickle cell disorders should prescribe NEUPOGEN® for such patients, and only after careful consideration of the potential risks and benefits. | |||
'''<i>Patients With Severe Chronic [[Neutropenia]]</i>''' | |||
The safety and efficacy of NEUPOGEN® in the treatment of neutropenia due to other hematopoietic disorders (eg‚ myelodysplastic syndrome [MDS]) have not been established. Care should be taken to confirm the diagnosis of SCN before initiating NEUPOGEN® therapy. | |||
MDS and AML have been reported to occur in the natural history of congenital neutropenia without cytokine therapy.17 Cytogenetic abnormalities, transformation to MDS, and AML have also been observed in patients treated with NEUPOGEN® for SCN. Based on available data including a postmarketing surveillance study, the risk of developing MDS and AML appears to be confined to the subset of patients with congenital neutropenia. Abnormal cytogenetics and MDS have been associated with the eventual development of myeloid leukemia. The effect of NEUPOGEN® on the development of abnormal cytogenetics and the effect of continued NEUPOGEN® administration in patients with abnormal cytogenetics or MDS are unknown. If a patient with SCN develops abnormal cytogenetics or myelodysplasia‚ the risks and benefits of continuing NEUPOGEN® should be carefully considered. | |||
==PRECAUTIONS== | |||
===<u>General</u>=== | |||
''' Simultaneous Use With Chemotherapy and Radiation Therapy''' | |||
The safety and efficacy of NEUPOGEN® given simultaneously with cytotoxic chemotherapy have not been established. Because of the potential sensitivity of rapidly dividing myeloid cells to cytotoxic chemotherapy‚ do not use NEUPOGEN® in the period 24 hours before through 24 hours after the administration of cytotoxic chemotherapy (see DOSAGE AND ADMINISTRATION). | |||
The efficacy of NEUPOGEN® has not been evaluated in patients receiving chemotherapy associated with delayed myelosuppression (e.g., nitrosoureas), with mitomycin C, or with myelosuppressive doses of antimetabolites such as 5-fluorouracil. | |||
The safety and efficacy of NEUPOGEN® have not been evaluated in patients receiving concurrent radiation therapy. Simultaneous use of NEUPOGEN® with chemotherapy and radiation therapy should be avoided. | |||
'''Potential Effect on Malignant Cells''' | |||
NEUPOGEN® is a growth factor that primarily stimulates neutrophils. However‚ the possibility that NEUPOGEN® can act as a growth factor for any tumor type cannot be excluded. In a randomized study evaluating the effects of NEUPOGEN® versus placebo in patients undergoing remission induction for AML, there was no significant difference in remission rate, disease-free, or overall survival (see CLINICAL EXPERIENCE). | |||
The safety of NEUPOGEN® in chronic myeloid leukemia (CML) and myelodysplasia has not been established. | |||
When NEUPOGEN® is used to mobilize PBPC‚ tumor cells may be released from the marrow and subsequently collected in the leukapheresis product. The effect of reinfusion of tumor cells has not been well studied‚ and the limited data available are inconclusive. | |||
'''Leukocytosis''' | |||
<i>'''Cancer Patients Receiving Myelosuppressive Chemotherapy'''</i> | |||
White blood cell counts of 100‚000/mm3 or greater were observed in approximately 2% of patients receiving NEUPOGEN® at doses above 5 mcg/kg/day. There were no reports of adverse events associated with this degree of leukocytosis. In order to avoid the potential complications of excessive leukocytosis‚ a CBC is recommended twice per week during NEUPOGEN® therapy (see LABORATORY MONITORING). | |||
'''Premature Discontinuation of NEUPOGEN® Therapy''' | |||
<i>'''Cancer Patients Receiving Myelosuppressive Chemotherapy'''</i> | |||
A transient increase in neutrophil counts is typically seen 1 to 2 days after initiation of NEUPOGEN® therapy. However‚ for a sustained therapeutic response‚ NEUPOGEN® therapy should be continued following chemotherapy until the post-nadir ANC reaches 10‚000/mm3. Therefore‚ the premature discontinuation of NEUPOGEN® therapy‚ prior to the time of recovery from the expected neutrophil nadir‚ is generally not recommended (see DOSAGE AND ADMINISTRATION). | |||
<i>'''Immunogenicity'''</i> | |||
As with all therapeutic proteins, there is a potential for immunogenicity. The incidence of antibody development in patients receiving NEUPOGEN® has not been adequately determined. While available data suggest that a small proportion of patients developed binding antibodies to filgrastim, the nature and specificity of these antibodies has not been adequately studied. In clinical studies comparing NEUPOGEN® and Neulasta®, the incidence of antibodies binding to NEUPOGEN® was 3% (11/333). In these 11 patients, no evidence of a neutralizing response was observed using a cell-based bioassay. The detection of antibody formation is highly dependent on the sensitivity and specificity of the assay, and the observed incidence of antibody positivity in an assay may be influenced by several factors including timing of sampling, sample handling, concomitant medications, and underlying disease. Therefore, comparison of the incidence of antibodies to NEUPOGEN® with the incidence of antibodies to other products may be misleading. | |||
Cytopenias resulting from an antibody response to exogenous growth factors have been reported on rare occasions in patients treated with other recombinant growth factors. There is a theoretical possibility that an antibody directed against filgrastim may cross-react with endogenous G-CSF, resulting in immune-mediated neutropenia; however, this has not been reported in clinical studies or in post-marketing experience. Patients who develop hypersensitivity to filgrastim (NEUPOGEN®) may have allergic or hypersensitivity reactions to other E coli-derived proteins. | |||
'''Cutaneous Vasculitis''' | |||
Cutaneous vasculitis has been reported in patients treated with NEUPOGEN®. In most cases‚ the severity of cutaneous vasculitis was moderate or severe. Most of the reports involved patients with SCN receiving long-term NEUPOGEN® therapy. Symptoms of vasculitis generally developed simultaneously with an increase in the ANC and abated when the ANC decreased. Many patients were able to continue NEUPOGEN® at a reduced dose. | |||
'''Thrombocytopenia''' | |||
Thrombocytopenia has been reported in patients receiving NEUPOGEN®. Platelet counts should be monitored closely. | |||
'''<u>Information for Patients and Caregivers</u>''' | |||
Patients should be referred to the “Information for Patients and Caregivers” labeling included with the package insert in each dispensing pack of NEUPOGEN® vials or NEUPOGEN® prefilled syringes. The “Information for Patients and Caregivers” labeling provides information about neutrophils and neutropenia and the safety and efficacy of NEUPOGEN®. It is not intended to be a disclosure of all known or possible effects. | |||
<u>'''Laboratory Monitoring'''</u> | |||
<i>'''Cancer Patients Receiving Myelosuppressive Chemotherapy'''</i> | |||
A CBC and platelet count should be obtained prior to chemotherapy‚ and at regular intervals (twice per week) during NEUPOGEN® therapy. Following cytotoxic chemotherapy‚ the neutrophil nadir occurred earlier during cycles when NEUPOGEN® was administered‚ and WBC differentials demonstrated a left shift‚ including the appearance of promyelocytes and myeloblasts. In addition‚ the duration of severe neutropenia was reduced and was followed by an accelerated recovery in the neutrophil counts. | |||
<i>'''Cancer Patients Receiving Bone Marrow Transplant'''</i> | |||
Frequent CBCs and platelet counts are recommended (at least 3 times per week) following marrow transplantation. | |||
<i>'''Patients With Severe Chronic Neutropenia'''</i> | |||
During the initial 4 weeks of NEUPOGEN® therapy and during the 2 weeks following any dose adjustment‚ a CBC with differential and platelet count should be performed twice weekly. Once a patient is clinically stable‚ a CBC with differential and platelet count should be performed monthly during the first year of treatment. Thereafter, if clinically stable, routine monitoring with regular CBCs (i.e., as clinically indicated but at least quarterly) is recommended. Additionally, for those patients with congenital neutropenia, annual bone marrow and cytogenetic evaluations should be performed throughout the duration of treatment. | |||
In clinical trials‚ the following laboratory results were observed: | |||
* Cyclic fluctuations in the neutrophil counts were frequently observed in patients with congenital or idiopathic neutropenia after initiation of NEUPOGEN® therapy. | |||
* Platelet counts were generally at the upper limits of normal prior to NEUPOGEN® therapy. With NEUPOGEN® therapy‚ platelet counts decreased but usually remained within normal limits (see ADVERSE REACTIONS). | |||
* Early myeloid forms were noted in peripheral blood in most patients‚ including the appearance of metamyelocytes and myelocytes. Promyelocytes and myeloblasts were noted in some patients. | |||
* Relative increases were occasionally noted in the number of circulating eosinophils and basophils. No consistent increases were observed with NEUPOGEN® therapy. | |||
* As in other trials‚ increases were observed in serum uric acid‚ lactic dehydrogenase‚ and serum alkaline phosphatase. | |||
|alcohol=Alcohol-Filgrastim interaction has not been established. Talk to your doctor about the effects of taking alcohol with this medication. | |alcohol=Alcohol-Filgrastim interaction has not been established. Talk to your doctor about the effects of taking alcohol with this medication. | ||
}} | }} | ||
Revision as of 15:31, 21 August 2014
Editor-In-Chief: C. Michael Gibson, M.S., M.D. [1]; Associate Editor(s)-in-Chief: Sheng Shi, M.D. [2]
Disclaimer
WikiDoc MAKES NO GUARANTEE OF VALIDITY. WikiDoc is not a professional health care provider, nor is it a suitable replacement for a licensed healthcare provider. WikiDoc is intended to be an educational tool, not a tool for any form of healthcare delivery. The educational content on WikiDoc drug pages is based upon the FDA package insert, National Library of Medicine content and practice guidelines / consensus statements. WikiDoc does not promote the administration of any medication or device that is not consistent with its labeling. Please read our full disclaimer here.
Overview
Filgrastim is {{{aOrAn}}} {{{drugClass}}} that is FDA approved for the {{{indicationType}}} of Cancer Patients Receiving Myelosuppressive Chemotherapy, Patients With Acute Myeloid Leukemia Receiving Induction or Consolidation Chemotherapy, Cancer Patients Receiving Bone Marrow Transplant, Patients Undergoing Peripheral Blood Progenitor Cell Collection and Therapy, Patients With Severe Chronic Neutropenia. Common adverse reactions include Bone pain.
Adult Indications and Dosage
FDA-Labeled Indications and Dosage (Adult)
Cancer Patients Receiving Myelosuppressive Chemotherapy
- Dosing information
- Recommended starting dosage: 5 mcg/kg/day‚ administered as a single daily injection by SC bolus injection‚ by short IV infusion (15 to 30 minutes)‚ or by continuous SC or continuous IV infusion.
- A CBC and platelet count should be obtained before instituting NEUPOGEN® therapy and monitored twice weekly during therapy.
- Doses may be increased in increments of 5 mcg/kg for each chemotherapy cycle‚ according to the duration and severity of the ANC nadir.
- NEUPOGEN® should be administered no earlier than 24 hours after the administration of cytotoxic chemotherapy.
- NEUPOGEN® should not be administered in the period 24 hours before the administration of chemotherapy.
- NEUPOGEN® should be administered daily for up to 2 weeks‚ until the ANC has reached 10‚000/mm3 following the expected chemotherapy-induced neutrophil nadir.
- The duration of NEUPOGEN® therapy needed to attenuate chemotherapy-induced neutropenia may be dependent on the myelosuppressive potential of the chemotherapy regimen employed.
- NEUPOGEN® therapy should be discontinued if the ANC surpasses 10‚000/mm3 after the expected chemotherapy-induced neutrophil nadir.
Cancer Patients Receiving Bone Marrow Transplant
- Dosing information
- Recommended dosage following BMT: 10 mcg/kg/day given as an IV infusion of 4 or 24 hours‚ or as a continuous 24-hour SC infusion. For patients receiving BMT‚ the first dose of NEUPOGEN® should be administered at least 24 hours after cytotoxic chemotherapy and at least 24 hours after bone marrow infusion.
During the period of neutrophil recovery‚ the daily dose of NEUPOGEN® should be titrated against the neutrophil response as follows:
Peripheral Blood Progenitor Cell Collection and Therapy in Cancer Patients
- Dosing information
- Recommended dosage for the mobilization of PBPC: 10 mcg/kg/day SC‚ either as a bolus or a continuous infusion. It is recommended that NEUPOGEN® be given for at least 4 days before the first leukapheresis procedure and continued until the last leukapheresis. Although the optimal duration of NEUPOGEN® administration and leukapheresis schedule have not been established‚ administration of NEUPOGEN® for 6 to 7 days with leukaphereses on days 5‚ 6‚ and 7 was found to be safe and effective. Neutrophil counts should be monitored after 4 days of NEUPOGEN®, and NEUPOGEN® dose modification should be considered for those patients who develop a WBC count > 100‚000/mm3.
In all clinical trials of NEUPOGEN® for the mobilization of PBPC‚ NEUPOGEN® was also administered after reinfusion of the collected cells.
Patients With Severe Chronic Neutropenia
- Dosing information
- NEUPOGEN® should be administered to those patients in whom a diagnosis of congenital‚ cyclic‚ or idiopathic neutropenia has been definitively confirmed. Other diseases associated with neutropenia should be ruled out.
- Starting Dose:
- Congenital Neutropenia: The recommended daily starting dose is 6 mcg/kg BID SC every day.
- Idiopathic or Cyclic Neutropenia: The recommended daily starting dose is 5 mcg/kg injection SC qd.
- Dose Adjustments:
- Chronic daily administration is required to maintain clinical benefit. Absolute neutrophil count should not be used as the sole indication of efficacy. The dose should be individually adjusted based on the patient's clinical course as well as ANC. In the SCN postmarketing surveillance study, the reported median daily doses of NEUPOGEN® were: 6.0 mcg/kg (congenital neutropenia), 2.1 mcg/kg (cyclic neutropenia), and 1.2 mcg/kg (idiopathic neutropenia). In rare instances, patients with congenital neutropenia have required doses of NEUPOGEN® ≥ 100 mcg/kg/day.
Dilution
If required‚ NEUPOGEN® may be diluted in 5% dextrose. NEUPOGEN® diluted to concentrations between 5 and 15 mcg/mL should be protected from adsorption to plastic materials by the addition of Albumin (Human) to a final concentration of 2 mg/mL. When diluted in 5% dextrose or 5% dextrose plus Albumin (Human)‚ NEUPOGEN® is compatible with glass bottles‚ PVC and polyolefin IV bags‚ and polypropylene syringes. Dilution of NEUPOGEN® to a final concentration of less than 5 mcg/mL is not recommended at any time. Do not dilute with saline at any time; product may precipitate.
Off-Label Use and Dosage (Adult)
Guideline-Supported Use
Myelodysplastic syndrome
- Developed by: American Society of Clinical Oncology (ASCO)
- Class of Recommendation: Not applicable
- Level of Evidence: Not applicable
- Dosing Information
- Intermittent CSF use may be considered in patients with severe neutropenia and recurrent infections.
Cancer Patients Receiving Myelosuppressive Chemotherapy
- Dosing information
- Recommended starting dosage: 5 mcg/kg/day‚ administered as a single daily injection by SC bolus injection‚ by short IV infusion (15 to 30 minutes)‚ or by continuous SC or continuous IV infusion.
- A CBC and platelet count should be obtained before instituting NEUPOGEN® therapy and monitored twice weekly during therapy.
- Doses may be increased in increments of 5 mcg/kg for each chemotherapy cycle‚ according to the duration and severity of the ANC nadir.
- NEUPOGEN® should be administered no earlier than 24 hours after the administration of cytotoxic chemotherapy.
- NEUPOGEN® should not be administered in the period 24 hours before the administration of chemotherapy.
- NEUPOGEN® should be administered daily for up to 2 weeks‚ until the ANC has reached 10‚000/mm3 following the expected chemotherapy-induced neutrophil nadir.
- The duration of NEUPOGEN® therapy needed to attenuate chemotherapy-induced neutropenia may be dependent on the myelosuppressive potential of the chemotherapy regimen employed.
- NEUPOGEN® therapy should be discontinued if the ANC surpasses 10‚000/mm3 after the expected chemotherapy-induced neutrophil nadir.
Non–Guideline-Supported Use
Agranulocytosis
- Dosing information
- 350 micrograms/day 7507240
- 5 micrograms/kg/day subcutaneously for 7 days 7512460
- 300 micrograms/day subcutaneously7525175
Aplastic anemia
- Dosing information
- 20 milligrams/kilogram/day (mg/kg/day)
- Dosing information
- 6 micrograms/kilogram/day subcutaneously 12803133
Febrile neutropenia
- Dosing information
- 100mcg/m(2) to 400 mcg/m(2) 10071455
Infectious disease
- Dosing information
- 300 micrograms/day (mcg/day) subcutaneously to 480 mcg/day10803937
Leukemia
- Dosing information
- 5 micrograms/kilogram/day11426551
Mucositis following chemotherapy
- Dosing information
- 120 mcg (0.4 mL)9827976
Pediatric Indications and Dosage
FDA-Labeled Indications and Dosage (Pediatric)
Cancer Patients Receiving Myelosuppressive Chemotherapy
- Dosing information
- Recommended starting dosage: 5 mcg/kg/day‚ administered as a single daily injection by SC bolus injection‚ by short IV infusion (15 to 30 minutes)‚ or by continuous SC or continuous IV infusion.
- A CBC and platelet count should be obtained before instituting NEUPOGEN® therapy and monitored twice weekly during therapy.
- Doses may be increased in increments of 5 mcg/kg for each chemotherapy cycle‚ according to the duration and severity of the ANC nadir.
- NEUPOGEN® should be administered no earlier than 24 hours after the administration of cytotoxic chemotherapy.
- NEUPOGEN® should not be administered in the period 24 hours before the administration of chemotherapy.
- NEUPOGEN® should be administered daily for up to 2 weeks‚ until the ANC has reached 10‚000/mm3 following the expected chemotherapy-induced neutrophil nadir.
- The duration of NEUPOGEN® therapy needed to attenuate chemotherapy-induced neutropenia may be dependent on the myelosuppressive potential of the chemotherapy regimen employed.
- NEUPOGEN® therapy should be discontinued if the ANC surpasses 10‚000/mm3 after the expected chemotherapy-induced neutrophil nadir.
Cancer Patients Receiving Bone Marrow Transplant
- Dosing information
- Recommended dosage following BMT: 10 mcg/kg/day given as an IV infusion of 4 or 24 hours‚ or as a continuous 24-hour SC infusion. For patients receiving BMT‚ the first dose of NEUPOGEN® should be administered at least 24 hours after cytotoxic chemotherapy and at least 24 hours after bone marrow infusion.
During the period of neutrophil recovery‚ the daily dose of NEUPOGEN® should be titrated against the neutrophil response as follows:
Peripheral Blood Progenitor Cell Collection and Therapy in Cancer Patients
- Dosing information
- Recommended dosage for the mobilization of PBPC: 10 mcg/kg/day SC‚ either as a bolus or a continuous infusion. It is recommended that NEUPOGEN® be given for at least 4 days before the first leukapheresis procedure and continued until the last leukapheresis. Although the optimal duration of NEUPOGEN® administration and leukapheresis schedule have not been established‚ administration of NEUPOGEN® for 6 to 7 days with leukaphereses on days 5‚ 6‚ and 7 was found to be safe and effective. Neutrophil counts should be monitored after 4 days of NEUPOGEN®, and NEUPOGEN® dose modification should be considered for those patients who develop a WBC count > 100‚000/mm3.
In all clinical trials of NEUPOGEN® for the mobilization of PBPC‚ NEUPOGEN® was also administered after reinfusion of the collected cells.
Patients With Severe Chronic Neutropenia
- Dosing information
- NEUPOGEN® should be administered to those patients in whom a diagnosis of congenital‚ cyclic‚ or idiopathic neutropenia has been definitively confirmed. Other diseases associated with neutropenia should be ruled out.
- Starting Dose:
- Congenital Neutropenia: The recommended daily starting dose is 6 mcg/kg BID SC every day.
- Idiopathic or Cyclic Neutropenia: The recommended daily starting dose is 5 mcg/kg injection SC qd.
- Dose Adjustments:
- Chronic daily administration is required to maintain clinical benefit. Absolute neutrophil count should not be used as the sole indication of efficacy. The dose should be individually adjusted based on the patient's clinical course as well as ANC. In the SCN postmarketing surveillance study, the reported median daily doses of NEUPOGEN® were: 6.0 mcg/kg (congenital neutropenia), 2.1 mcg/kg (cyclic neutropenia), and 1.2 mcg/kg (idiopathic neutropenia). In rare instances, patients with congenital neutropenia have required doses of NEUPOGEN® ≥ 100 mcg/kg/day.
Dilution
If required‚ NEUPOGEN® may be diluted in 5% dextrose. NEUPOGEN® diluted to concentrations between 5 and 15 mcg/mL should be protected from adsorption to plastic materials by the addition of Albumin (Human) to a final concentration of 2 mg/mL. When diluted in 5% dextrose or 5% dextrose plus Albumin (Human)‚ NEUPOGEN® is compatible with glass bottles‚ PVC and polyolefin IV bags‚ and polypropylene syringes. Dilution of NEUPOGEN® to a final concentration of less than 5 mcg/mL is not recommended at any time. Do not dilute with saline at any time; product may precipitate.
Off-Label Use and Dosage (Pediatric)
Guideline-Supported Use
There is limited information regarding Off-Label Guideline-Supported Use of Filgrastim in pediatric patients.
Non–Guideline-Supported Use
Aplastic anemia
- Dosing information
- Not applicable 10979946
Neutropenia - Pre-eclampsia
- Dosing information
- 5 or 10 micrograms/kilogram (mcg/kg)/day9794941
Septicemia of newborn
- Dosing information
- Not applicable 11391341
Shwachman syndrome
- Dosing information
- Not applicable 1700246
Contraindications
NEUPOGEN® is contraindicated in patients with known hypersensitivity to E coli-derived proteins‚ filgrastim‚ or any component of the product.
Warnings
Allergic Reactions
Allergic-type reactions occurring on initial or subsequent treatment have been reported in < 1 in 4000 patients treated with NEUPOGEN®. These have generally been characterized by systemic symptoms involving at least two body systems‚ most often skin (rash‚ urticaria‚ facial edema)‚ respiratory (wheezing‚ dyspnea)‚ and cardiovascular (hypotension‚ tachycardia). Some reactions occurred on initial exposure. Reactions tended to occur within the first 30 minutes after administration and appeared to occur more frequently in patients receiving NEUPOGEN® IV. Rapid resolution of symptoms occurred in most cases after administration of antihistamines‚ steroids‚ bronchodilators‚ and/or epinephrine. Symptoms recurred in more than half the patients who were rechallenged.
SPLENIC RUPTURE, INCLUDING FATAL CASES, HAS BEEN REPORTED FOLLOWING THE ADMINISTRATION OF NEUPOGEN®. INDIVIDUALS RECEIVING NEUPOGEN® WHO REPORT LEFT UPPER ABDOMINAL AND/OR SHOULDER TIP PAIN SHOULD BE EVALUATED FOR AN ENLARGED SPLEEN OR SPLENIC RUPTURE.
Acute Respiratory Distress Syndrome (ARDS)
Acute respiratory distress syndrome (ARDS) has been reported in patients receiving NEUPOGEN®, and is postulated to be secondary to an influx of neutrophils to sites of inflammation in the lungs. Patients receiving NEUPOGEN® who develop fever, lung infiltrates, or respiratory distress should be evaluated for the possibility of ARDS. In the event that ARDS occurs, NEUPOGEN® should be withheld until resolution of ARDS or discontinued. Patients should receive appropriate medical management for this condition.
Alveolar Hemorrhage and Hemoptysis
Alveolar hemorrhage manifesting as pulmonary infiltrates and hemoptysis requiring hospitalization has been reported in healthy donors undergoing PBPC mobilization. Hemoptysis resolved with discontinuation of NEUPOGEN®. The use of NEUPOGEN® for PBPC mobilization in healthy donors is not an approved indication.
Severe sickle cell crises, in some cases resulting in death, have been associated with the use of NEUPOGEN® in patients with sickle cell disorders. Only physicians qualified by specialized training or experience in the treatment of patients with sickle cell disorders should prescribe NEUPOGEN® for such patients, and only after careful consideration of the potential risks and benefits.
Patients With Severe Chronic Neutropenia
The safety and efficacy of NEUPOGEN® in the treatment of neutropenia due to other hematopoietic disorders (eg‚ myelodysplastic syndrome [MDS]) have not been established. Care should be taken to confirm the diagnosis of SCN before initiating NEUPOGEN® therapy. MDS and AML have been reported to occur in the natural history of congenital neutropenia without cytokine therapy.17 Cytogenetic abnormalities, transformation to MDS, and AML have also been observed in patients treated with NEUPOGEN® for SCN. Based on available data including a postmarketing surveillance study, the risk of developing MDS and AML appears to be confined to the subset of patients with congenital neutropenia. Abnormal cytogenetics and MDS have been associated with the eventual development of myeloid leukemia. The effect of NEUPOGEN® on the development of abnormal cytogenetics and the effect of continued NEUPOGEN® administration in patients with abnormal cytogenetics or MDS are unknown. If a patient with SCN develops abnormal cytogenetics or myelodysplasia‚ the risks and benefits of continuing NEUPOGEN® should be carefully considered.
PRECAUTIONS
General
Simultaneous Use With Chemotherapy and Radiation Therapy
The safety and efficacy of NEUPOGEN® given simultaneously with cytotoxic chemotherapy have not been established. Because of the potential sensitivity of rapidly dividing myeloid cells to cytotoxic chemotherapy‚ do not use NEUPOGEN® in the period 24 hours before through 24 hours after the administration of cytotoxic chemotherapy (see DOSAGE AND ADMINISTRATION). The efficacy of NEUPOGEN® has not been evaluated in patients receiving chemotherapy associated with delayed myelosuppression (e.g., nitrosoureas), with mitomycin C, or with myelosuppressive doses of antimetabolites such as 5-fluorouracil. The safety and efficacy of NEUPOGEN® have not been evaluated in patients receiving concurrent radiation therapy. Simultaneous use of NEUPOGEN® with chemotherapy and radiation therapy should be avoided.
Potential Effect on Malignant Cells
NEUPOGEN® is a growth factor that primarily stimulates neutrophils. However‚ the possibility that NEUPOGEN® can act as a growth factor for any tumor type cannot be excluded. In a randomized study evaluating the effects of NEUPOGEN® versus placebo in patients undergoing remission induction for AML, there was no significant difference in remission rate, disease-free, or overall survival (see CLINICAL EXPERIENCE). The safety of NEUPOGEN® in chronic myeloid leukemia (CML) and myelodysplasia has not been established. When NEUPOGEN® is used to mobilize PBPC‚ tumor cells may be released from the marrow and subsequently collected in the leukapheresis product. The effect of reinfusion of tumor cells has not been well studied‚ and the limited data available are inconclusive.
Leukocytosis
Cancer Patients Receiving Myelosuppressive Chemotherapy
White blood cell counts of 100‚000/mm3 or greater were observed in approximately 2% of patients receiving NEUPOGEN® at doses above 5 mcg/kg/day. There were no reports of adverse events associated with this degree of leukocytosis. In order to avoid the potential complications of excessive leukocytosis‚ a CBC is recommended twice per week during NEUPOGEN® therapy (see LABORATORY MONITORING).
Premature Discontinuation of NEUPOGEN® Therapy
Cancer Patients Receiving Myelosuppressive Chemotherapy
A transient increase in neutrophil counts is typically seen 1 to 2 days after initiation of NEUPOGEN® therapy. However‚ for a sustained therapeutic response‚ NEUPOGEN® therapy should be continued following chemotherapy until the post-nadir ANC reaches 10‚000/mm3. Therefore‚ the premature discontinuation of NEUPOGEN® therapy‚ prior to the time of recovery from the expected neutrophil nadir‚ is generally not recommended (see DOSAGE AND ADMINISTRATION).
Immunogenicity
As with all therapeutic proteins, there is a potential for immunogenicity. The incidence of antibody development in patients receiving NEUPOGEN® has not been adequately determined. While available data suggest that a small proportion of patients developed binding antibodies to filgrastim, the nature and specificity of these antibodies has not been adequately studied. In clinical studies comparing NEUPOGEN® and Neulasta®, the incidence of antibodies binding to NEUPOGEN® was 3% (11/333). In these 11 patients, no evidence of a neutralizing response was observed using a cell-based bioassay. The detection of antibody formation is highly dependent on the sensitivity and specificity of the assay, and the observed incidence of antibody positivity in an assay may be influenced by several factors including timing of sampling, sample handling, concomitant medications, and underlying disease. Therefore, comparison of the incidence of antibodies to NEUPOGEN® with the incidence of antibodies to other products may be misleading. Cytopenias resulting from an antibody response to exogenous growth factors have been reported on rare occasions in patients treated with other recombinant growth factors. There is a theoretical possibility that an antibody directed against filgrastim may cross-react with endogenous G-CSF, resulting in immune-mediated neutropenia; however, this has not been reported in clinical studies or in post-marketing experience. Patients who develop hypersensitivity to filgrastim (NEUPOGEN®) may have allergic or hypersensitivity reactions to other E coli-derived proteins.
Cutaneous Vasculitis
Cutaneous vasculitis has been reported in patients treated with NEUPOGEN®. In most cases‚ the severity of cutaneous vasculitis was moderate or severe. Most of the reports involved patients with SCN receiving long-term NEUPOGEN® therapy. Symptoms of vasculitis generally developed simultaneously with an increase in the ANC and abated when the ANC decreased. Many patients were able to continue NEUPOGEN® at a reduced dose.
Thrombocytopenia
Thrombocytopenia has been reported in patients receiving NEUPOGEN®. Platelet counts should be monitored closely.
Information for Patients and Caregivers
Patients should be referred to the “Information for Patients and Caregivers” labeling included with the package insert in each dispensing pack of NEUPOGEN® vials or NEUPOGEN® prefilled syringes. The “Information for Patients and Caregivers” labeling provides information about neutrophils and neutropenia and the safety and efficacy of NEUPOGEN®. It is not intended to be a disclosure of all known or possible effects.
Laboratory Monitoring
Cancer Patients Receiving Myelosuppressive Chemotherapy
A CBC and platelet count should be obtained prior to chemotherapy‚ and at regular intervals (twice per week) during NEUPOGEN® therapy. Following cytotoxic chemotherapy‚ the neutrophil nadir occurred earlier during cycles when NEUPOGEN® was administered‚ and WBC differentials demonstrated a left shift‚ including the appearance of promyelocytes and myeloblasts. In addition‚ the duration of severe neutropenia was reduced and was followed by an accelerated recovery in the neutrophil counts.
Cancer Patients Receiving Bone Marrow Transplant
Frequent CBCs and platelet counts are recommended (at least 3 times per week) following marrow transplantation.
Patients With Severe Chronic Neutropenia
During the initial 4 weeks of NEUPOGEN® therapy and during the 2 weeks following any dose adjustment‚ a CBC with differential and platelet count should be performed twice weekly. Once a patient is clinically stable‚ a CBC with differential and platelet count should be performed monthly during the first year of treatment. Thereafter, if clinically stable, routine monitoring with regular CBCs (i.e., as clinically indicated but at least quarterly) is recommended. Additionally, for those patients with congenital neutropenia, annual bone marrow and cytogenetic evaluations should be performed throughout the duration of treatment. In clinical trials‚ the following laboratory results were observed:
- Cyclic fluctuations in the neutrophil counts were frequently observed in patients with congenital or idiopathic neutropenia after initiation of NEUPOGEN® therapy.
- Platelet counts were generally at the upper limits of normal prior to NEUPOGEN® therapy. With NEUPOGEN® therapy‚ platelet counts decreased but usually remained within normal limits (see ADVERSE REACTIONS).
- Early myeloid forms were noted in peripheral blood in most patients‚ including the appearance of metamyelocytes and myelocytes. Promyelocytes and myeloblasts were noted in some patients.
- Relative increases were occasionally noted in the number of circulating eosinophils and basophils. No consistent increases were observed with NEUPOGEN® therapy.
- As in other trials‚ increases were observed in serum uric acid‚ lactic dehydrogenase‚ and serum alkaline phosphatase.
Adverse Reactions
Clinical Trials Experience
There is limited information regarding Filgrastim Clinical Trials Experience in the drug label.
Postmarketing Experience
There is limited information regarding Filgrastim Postmarketing Experience in the drug label.
Drug Interactions
There is limited information regarding Filgrastim Drug Interactions in the drug label.
Use in Specific Populations
Pregnancy
Pregnancy Category (FDA):
There is no FDA guidance on usage of Filgrastim in women who are pregnant.
Pregnancy Category (AUS):
There is no Australian Drug Evaluation Committee (ADEC) guidance on usage of Filgrastim in women who are pregnant.
Labor and Delivery
There is no FDA guidance on use of Filgrastim during labor and delivery.
Nursing Mothers
There is no FDA guidance on the use of Filgrastim in women who are nursing.
Pediatric Use
There is no FDA guidance on the use of Filgrastim in pediatric settings.
Geriatic Use
There is no FDA guidance on the use of Filgrastim in geriatric settings.
Gender
There is no FDA guidance on the use of Filgrastim with respect to specific gender populations.
Race
There is no FDA guidance on the use of Filgrastim with respect to specific racial populations.
Renal Impairment
There is no FDA guidance on the use of Filgrastim in patients with renal impairment.
Hepatic Impairment
There is no FDA guidance on the use of Filgrastim in patients with hepatic impairment.
Females of Reproductive Potential and Males
There is no FDA guidance on the use of Filgrastim in women of reproductive potentials and males.
Immunocompromised Patients
There is no FDA guidance one the use of Filgrastim in patients who are immunocompromised.
Administration and Monitoring
Administration
There is limited information regarding Filgrastim Administration in the drug label.
Monitoring
There is limited information regarding Filgrastim Monitoring in the drug label.
IV Compatibility
There is limited information regarding the compatibility of Filgrastim and IV administrations.
Overdosage
There is limited information regarding Filgrastim overdosage. If you suspect drug poisoning or overdose, please contact the National Poison Help hotline (1-800-222-1222) immediately.
Pharmacology
There is limited information regarding Filgrastim Pharmacology in the drug label.
Mechanism of Action
There is limited information regarding Filgrastim Mechanism of Action in the drug label.
Structure
There is limited information regarding Filgrastim Structure in the drug label.
Pharmacodynamics
There is limited information regarding Filgrastim Pharmacodynamics in the drug label.
Pharmacokinetics
There is limited information regarding Filgrastim Pharmacokinetics in the drug label.
Nonclinical Toxicology
There is limited information regarding Filgrastim Nonclinical Toxicology in the drug label.
Clinical Studies
There is limited information regarding Filgrastim Clinical Studies in the drug label.
How Supplied
There is limited information regarding Filgrastim How Supplied in the drug label.
Storage
There is limited information regarding Filgrastim Storage in the drug label.
Images
Drug Images
{{#ask: Page Name::Filgrastim |?Pill Name |?Drug Name |?Pill Ingred |?Pill Imprint |?Pill Dosage |?Pill Color |?Pill Shape |?Pill Size (mm) |?Pill Scoring |?NDC |?Drug Author |format=template |template=DrugPageImages |mainlabel=- |sort=Pill Name }}
Package and Label Display Panel
{{#ask: Label Page::Filgrastim |?Label Name |format=template |template=DrugLabelImages |mainlabel=- |sort=Label Page }}
Patient Counseling Information
There is limited information regarding Filgrastim Patient Counseling Information in the drug label.
Precautions with Alcohol
Alcohol-Filgrastim interaction has not been established. Talk to your doctor about the effects of taking alcohol with this medication.
Brand Names
There is limited information regarding Filgrastim Brand Names in the drug label.
Look-Alike Drug Names
There is limited information regarding Filgrastim Look-Alike Drug Names in the drug label.
Drug Shortage Status
Price
References
The contents of this FDA label are provided by the National Library of Medicine.