Fat embolism syndrome: Difference between revisions
No edit summary |
(No difference)
|
Revision as of 16:38, 30 March 2010
For patient information click here
| Fat embolism syndrome | ||
| ICD-10 | O88.8, T79.1 | |
|---|---|---|
| ICD-9 | 673.8 | |
| DiseasesDB | 4766 | |
| eMedicine | med/652 | |
| MeSH | C14.907.355.350.454 | |
Editor-In-Chief: C. Michael Gibson, M.S., M.D. [1]
Overview
A fat embolism is a type of embolism that is often (but not always) caused by physical trauma. Fat emboli can occur whenever there is a *Pulmonary embolism
- CT pulmonary angiogram. The original description of fat embolism was in 1873 by Von Bergmann: “Ein fall todlicher fettembolie.” The fat embolism syndrome (FES) is characterized by the triad of hypoxemia, mental status changes and petechiae. The syndrome is usually trauma related and seen with closed fractures of the long bones or pelvis.
Epidemiology and Demographics
Patients with long bone fractures have a 1-20% chance of developing FES. It has been reported in liposuction, fatty liver, burns, bone marrot transplant (BMT) and bone marrow (BM) harvesting, bone tumor lysis, and sickle cell disease.
Pathophysiology
The pathogenesis of FES is not completely defined. It is thought to be caused by blockage of vessels from systemic embolization of fat globules. Echocardiographic reports have demonstrated echogenic material passing through the right atrium followed by increased pulmonary pressures and right heart pressures and subsequent paradoxical embolization of this material through a patent foramen ovale (PFO).
The fat induces a toxic, inflammatory reaction. This inflammatory reaction is thought to be related to the production of free fatty acids. Studies have shown that neutral fatty acids are not toxic , however, they are hydrolyzed over many hours to substances proven to cause ARDS in animal models. Not surprisingly, C-reactive protein is usually elevated in these patients. Levels of lipoprotein lipase, and free fatty acids (FFA) are noted in animal models.
Natural History
The syndrome typically occurs 12-24 hrs after the inciting event. It can occur as early as 12 hrs and as late as 2 weeks. Patients are often dyspneic, tachypneic and hypoxic. 50% of patients with FES require mechanical ventilation and progression to adult respiratory distress syndrome (ARDS) may develop.
The majority of patients develop neurologic abnormalities, usually after the development of respiratory distress. The usualy demonstrate an acute confusional state that may progress to coma. In most cases, if the patient survives, the neurologic abnormalities are transient.
The petichial rash is the last finding to develop. It occurs in only 30-50% of patients with FES. It is most often found on the head, neck, anterior thorax, subconjunctiva and axilla. It usually resolves in 5-7 days.
Scotoma, fever, lipiduria, disseminated intravascular coagulation (DIC) and cardiogenic shock are seen.
Diagnosis
FES is a clinical diagnosis. Chest X-rays are normal in the majority. Some may have evidence of consolidation, edema or hemmorhage, usually in the periphery. Pulmonary ventilation/perfusion scans (V/Q scans) demonstrate multiple subsegmental perfusion defects.
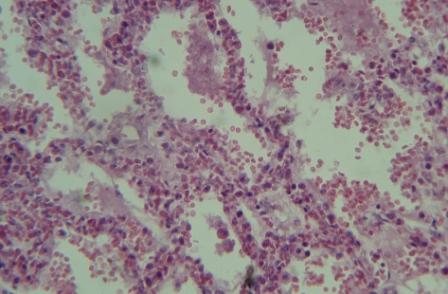
The recovery of fat from pulmonary artery (PA) catheter wedged blood, sputum and urine is nonspecific. One study found fat in 50% of sera from patients with long bone fractures who had no evidence of FES. Bronchoscopy and bronchoalveolar lavage (BAL) seem to be more specific by demonstrating fat droplets in alveolar macrophages.
Chest X Ray
Echocardiography
Echocardiographic reports have demonstrated echogenic material passing through the right atrium followed by increased pulmonary pressures and right heart pressures and subsequent paradoxical embolization of this material through a patent foramen ovale (PFO).
Other Diagnostic Studies
Treatment
Mortality occurs in 5-15% of patients. Early immobilization of fractures and operative rather than conservative management decrease the risk of FES. Some studies have shown a benefit in steroid prophylaxis for patients at high risk for FES (closed pelvic fracture), while others have not. There is no benefit to steroids after FES has developed.
References
Acknowledgements
Source of Initial Content: Morning report notes prepared by Editor-In-Chief: C. Michael Gibson, M.S., M.D. [2] and Dr. Duane Pinto
External links
Template:Consequences of external causes Template:SIB
- ↑ Gerald L. Weinhouse. Fat Embolism Syndrome.