Enalapril maleate
{{DrugProjectFormSinglePage |authorTag=Ahmed Zaghw, M.D. [1], Amr Marawan, M.D. [2], Sheng Shi, M.D. [3], Rabin Bista, M.B.B.S. [4] |genericName=Enalapril |aOrAn=an |drugClass=angiontensin converting enzyme inhibitor |indicationType=treatment |indication=hypertension, heart failure, left ventricular dysfunction after myocardial infarction, diabetic nephropathy |hasBlackBoxWarning=Yes |adverseReactions=hyperkalemia, dizziness, increase in serum blood urea nitrogen, increase in serum creatinine, fatigue |blackBoxWarningTitle=USE IN PREGNANCY |blackBoxWarningBody=When used in pregnancy during the second and third trimesters, ACE inhibitors can cause injury and even death to the developing fetus. When pregnancy is detected, enalapril maleate should be discontinued as soon as possible. |fdaLIADAdult======Hypertension=====
- Dosing Information
- Treatment with diuretic:
- Initial dosage: 2.5 mg for at least 4 hours
- Treatment without diuretic:
- Initial dose (not receiving a diuretic): Enalapril 5 mg PO qd, adjusted according to blood pressure response
- Usual dosage range: Enalapril 10—40 mg PO qd on two divided doses, adjust dose based on response (MAX 40 mg/day)
- Notice that:
- Diuretic should, if possible, be discontinued for two to three days before beginning therapy with Vasotec.
- In some patients treated once daily, the antihypertensive effect may diminish toward the end of the dosing interval. In such patients, an increase in dosage or twice daily administration should be considered. If blood pressure is not controlled with VASOTEC alone, a diuretic may be added. Concomitant administration of VASOTEC with potassium supplements, potassium salt substitutes, or potassium-sparing diuretics may lead to increases of serum potassium.
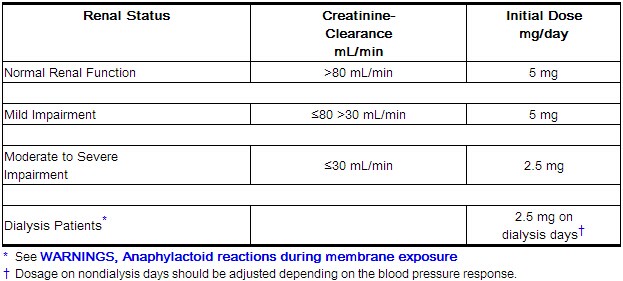
Dosage Adjustment in Hypertensive Patients with Renal Impairment
- Dosing information
- For patients with a creatinine clearance >30 mL/min (serum creatinine of up to approximately 3 mg/dL): As above.
- For patients with a creatinine clearance ≤30 mL/min (serum creatinine ≥3 mg/dL)
- Initial dosage: 2.5 mg PO qd
- Maxium dosage: 40 mg PO qd or until blood pressure is controlled.
Heart failure
- Dosing Information
- Initial dose : 2.5 mg PO qd or bid
- Maintenance dose: 2.5 - 20 mg PO qd or 10—20 mg PO bid, in a divided doses (MAX 40 mg/day)
- After the initial dose of VASOTEC, the patient should be observed under medical supervision for at least two hours and until blood pressure has stabilized for at least an additional hour. If possible, the dose of any concomitant diuretic should be reduced which may diminish the likelihood of hypotension. The appearance of hypotension after the initial dose of VASOTEC does not preclude subsequent careful dose titration with the drug, following effective management of the hypotension.
Asymptomatic Left Ventricular Dysfunction
- Dosing information
- Initial dosage: 2.5 mg PO bid
- Targeted daily dose: 20 mg/day in divided dose
- After the initial dose of VASOTEC, the patient should be observed under medical supervision for at least two hours and until blood pressure has stabilized for at least an additional hour. If possible, the dose of any concomitant diuretic should be reduced which may diminish the likelihood of hypotension. The appearance of hypotension after the initial dose of VASOTEC does not preclude subsequent careful dose titration with the drug, following effective management of the hypotension.
Dosage Adjustment in Patients with Heart Failure and Renal Impairment or Hyponatremia
- Dosing information
- For patients with heart failure who have hyponatremia (serum sodium less than 130 mEq/L) or with serum creatinine greater than 1.6 mg/dL
- Initial dosage: 2.5 mg/dayunder close medical supervision
- Max dosage: 40 mg/day(the dosage should be increased gradually)
Pediatric Hypertensive Patients
- Dosing information
- Usual recommended starting dose: 0.08 mg/kg (up to 5 mg) PO qd, adjusted according to blood pressure response
- Doses above 0.58 mg/kg (or in excess of 40 mg) have not been studied in pediatric patients.
- VASOTEC is not recommended in neonates and in pediatric patients with glomerular filtration rate <30 mL/min/1.73 m2, as no data are available.
|offLabelAdultGuideSupport=
Myocardial Infarction
- Class of Recommendation: Class IIa
- Level of Evidence: Not applicable
- Dosing information
- Not applicable
|offLabelAdultNoGuideSupport=
Cardiomyopathy
- Dosing information
- 2.5 mg or 5 mg qd or bid[1]
Aortic valve regurgitation
- Dosing information
Chyluria
- Dosing information
- 5 mg bid[4]
Prophylaxis treatment of Diabetes mellitus
- Dosing information
- 5-20 mg/day[5]
Diabetic nephropathy
- Dosing information
Direct current cardioversion
- Dosing information
- 10 mg PO bid to 20 mg bid[10]
Erythrocytosis
- Dosing information
|fdaLIADPed======Heart failure=====
- Dosing Information ( refractory to diuretic therapy )
- Initial dose : Enalapril 0.1 mg/kg/day PO
Hypertension
- Dosing Information
- Initial dose : Enalapril 0.08 mg/kg/day (up to 5 mg) PO
- Maintenance dose : adjust dose based on respons Enalapril (MAX dose 0.58 mg/kg or 40 mg/day)
|offLabelPedGuideSupport=There is limited information about the guideline-supported off-label use.
|offLabelPedNoGuideSupport=
Alport syndrome
- Dosing Information
- 40 mg/day [19]
Cardiomyopathy
- Dosing information
- 0.05 mg/kg/day-0.15 mg/kg/day[20]
Diabetic nephropathy
- Dosing information
- 0.2 mg/kg (max: 10 mg/day)[21]
Erythrocytosis
- Dosing information
- 0.5 mg/kg/day[22]
Prophylaxis treatment of Migraine
- Dosing information
- 10-25 mg/day[23]
Myocardial infarction
- Dosing information
- 2.5 mg/day[24]
Neurally-mediated syncope
- Dosing information
- 10 mg/day[25]
Renovascular hypertension
- Dosing information
- 5 mg/day[26]
|contraindications=* History of hypersensitivity or angioedema related to previous treatment with an angiotensin converting enzyme inhibitor.
- Patients with hereditary or idiopathic angioedema.
|warnings=====Anaphylactoid and Possibly Related Reactions====
- Presumably because angiotensin-converting enzyme inhibitors affect the metabolism of eicosanoids and polypeptides, including endogenous bradykinin, patients receiving ACE inhibitors (including enalaprilat) may be subject to a variety of adverse reactions, some of them serious.
Head and Neck Angioedema
- Angioedema of the face, extremities, lips, tongue, glottis and/or larynx has been reported in patients treated with angiotensin converting enzyme inhibitors, including enalaprilat. This may occur at any time during treatment. In such cases enalaprilat should be promptly discontinued and appropriate therapy and monitoring should be provided until complete and sustained resolution of signs and symptoms has occurred. In instances where swelling has been confined to the face and lips the condition has generally resolved without treatment, although antihistamines have been useful in relieving symptoms. Angioedema associated with laryngeal edema may be fatal. Where there is involvement of the tongue, glottis or larynx, likely to cause airway obstruction, appropriate therapy, e.g., subcutaneous epinephrine solution 1:1000 (0.3 mL to 0.5 mL) and/or measures necessary to ensure a patent airway, should be promptly provided.
Intestinal Angioedema
- Intestinal angioedema has been reported in patients treated with ACE inhibitors. These patients presented with abdominal pain (with or without nausea or vomiting); in some cases there was no prior history of facial angioedema and C-1 esterase levels were normal. The angioedema was diagnosed by procedures including abdominal CT scan or ultrasound, or at surgery, and symptoms resolved after stopping the ACE inhibitor. Intestinal angioedema should be included in the differential diagnosis of patients on ACE inhibitors presenting with abdominal pain.
Anaphylactoid reactions during desensitization
- Two patients undergoing desensitizing treatment with hymenoptera venom while receiving ACE inhibitors sustained life-threatening anaphylactoid reactions. In the same patients, these reactions were avoided when ACE inhibitors were temporarily withheld, but they reappeared upon inadvertent rechallenge.
Anaphylactoid reactions during membrane exposure
- Anaphylactoid reactions have been reported in patients dialyzed with high-flux membranes and treated concomitantly with an ACE inhibitor. Anaphylactoid reactions have also been reported in patients undergoing low-density lipoprotein apheresis with dextran sulfate absorption.
Hypotension
- Excessive hypotension is rare in uncomplicated hypertensive patients treated with enalaprilat alone. Patients with heart failure given enalaprilat commonly have some reduction in blood pressure, especially with the first dose, but discontinuation of therapy for continuing symptomatic hypotension usually is not necessary when dosing instructions are followed; caution should be observed when initiating therapy. Patients at risk for excessive hypotension, sometimes associated with oliguria and/or progressive azotemia, and rarely with acute renal failure and/or death, include those with the following conditions or characteristics: heart failure, hyponatremia, high dose diuretic therapy, recent intensive diuresis or increase in diuretic dose, renal dialysis, or severe volume and/or salt depletion of any etiology. It may be advisable to eliminate the diuretic (except in patients with heart failure), reduce the diuretic dose or increase salt intake cautiously before initiating therapy with enalaprilat in patients at risk for excessive hypotension who are able to tolerate such adjustments. In patients at risk for excessive hypotension, therapy should be started under very close medical supervision and such patients should be followed closely for the first two weeks of treatment and whenever the dose of enalapril and/or diuretic is increased. Similar considerations may apply to patients with ischemic heart or cerebrovascular disease, in whom an excessive fall in blood pressure could result in a myocardial infarction or cerebrovascular accident.
- If excessive hypotension occurs, the patient should be placed in the supine position and, if necessary, receive an intravenous infusion of normal saline. A transient hypotensive response is not a contraindication to further doses of enalaprilat, which usually can be given without difficulty once the blood pressure has stabilized. If symptomatic hypotension develops, a dose reduction or discontinuation of enalaprilat or concomitant diuretic may be necessary.
Neutropenia/Agranulocytosis
- Another angiotensin converting enzyme inhibitor, captopril, has been shown to cause agranulocytosis and bone marrow depression, rarely in uncomplicated patients but more frequently in patients with renal impairment especially if they also have a collagen vascular disease. Available data from clinical trials of enalapril are insufficient to show that enalapril does not cause agranulocytosis at similar rates. Marketing experience has revealed cases of neutropenia or agranulocytosis in which a causal relationship to enalapril cannot be excluded. Periodic monitoring of white blood cell counts in patients with collagen vascular disease and renal disease should be considered.
Hepatic Failure
- Rarely, ACE inhibitors have been associated with a syndrome that starts with cholestatic jaundice and progresses to fulminant hepatic necrosis, and (sometimes) death. The mechanism of this syndrome is not understood. Patients receiving ACE inhibitors who develop jaundice or marked elevations of hepatic enzymes should discontinue the ACE inhibitor and receive appropriate medical follow-up.
Fetal/Neonatal Morbidity and Mortality
- ACE inhibitors can cause fetal and neonatal morbidity and death when administered to pregnant women. Several dozen cases have been reported in the world literature. When pregnancy is detected, ACE inhibitors should be discontinued as soon as possible.
- In a published restrospective epidemiological study, infants whose mothers had taken an ACE inhibitor during their first trimester of pregnancy appeared to have an increased risk of major congenital malformations compared with infants whose mothers had not undergone first trimester exposure to ACE inhibitor drugs. The number of cases of birth defects is small and the findings of this study have not yet been repeated.
- The use of ACE inhibitors during the second and third trimesters of pregnancy has been associated with fetal and neonatal injury, including hypotension, neonatal skull hypoplasia, anuria, reversible or irreversible renal failure, and death. Oligohydramnios has also been reported, presumably resulting from decreased fetal renal function; oligohydramnios in this setting has been associated with fetal limb contractures, craniofacial deformation, and hypoplastic lung development. Prematurity, intrauterine growth retardation, and patent ductus arteriosus have also been reported, although it is not clear whether these occurrences were due to the ACE-inhibitor exposure.
- These adverse effects do not appear to have resulted from intrauterine ACE-inhibitor exposure that has been limited to the first trimester. Mothers whose embryos and fetuses are exposed to ACE inhibitors only during the first trimester should be so informed. Nonetheless, when patients become pregnant, physicians should make every effort to discontinue the use of enalaprilat as soon as possible.
- Rarely (probably less often than once in every thousand pregnancies), no alternative to ACE inhibitors will be found. In these rare cases, the mothers should be apprised of the potential hazards to their fetuses, and serial ultrasound examinations should be performed to assess the intraamniotic environment.
- If oligohydramnios is observed, enalaprilat should be discontinued unless it is considered lifesaving for the mother. Contraction stress testing (CST), a non-stress test (NST), or biophysical profiling (BPP) may be appropriate, depending upon the week of pregnancy. Patients and physicians should be aware, however, that oligohydramnios may not appear until after the fetus has sustained irreversible injury.
- Infants with histories of in utero exposure to ACE inhibitors should be closely observed for hypotension, oliguria, and hyperkalemia. If oliguria occurs, attention should be directed toward support of blood pressure and renal perfusion. Exchange transfusion or dialysis may be required as means of reversing hypotension and/or substituting for disordered renal function. Enalapril, which crosses the placenta, has been removed from neonatal circulation by peritoneal dialysis with some clinical benefit, and theoretically may be removed by exchange transfusion, although there is no experience with the latter procedure.
- No teratogenic effects of enalapril were seen in studies of pregnant rats and rabbits. On a body surface area basis, the doses used were 57 times and 12 times, respectively, the maximum recommended human daily dose (MRHDD).
|clinicalTrials=* Enalaprilat has been evaluated for safety in more than 10,000 patients, including over 1000 patients treated for one year or more. enalaprilat has been found to be generally well tolerated in controlled clinical trials involving 2987 patients.
- For the most part, adverse experiences were mild and transient in nature. In clinical trials, discontinuation of therapy due to clinical adverse experiences was required in 3.3 percent of patients with hypertension and in 5.7 percent of patients with heart failure. The frequency of adverse experiences was not related to total daily dosage within the usual dosage ranges. In patients with hypertension the overall percentage of patients treated with enalaprilat reporting adverse experiences was comparable to placebo.
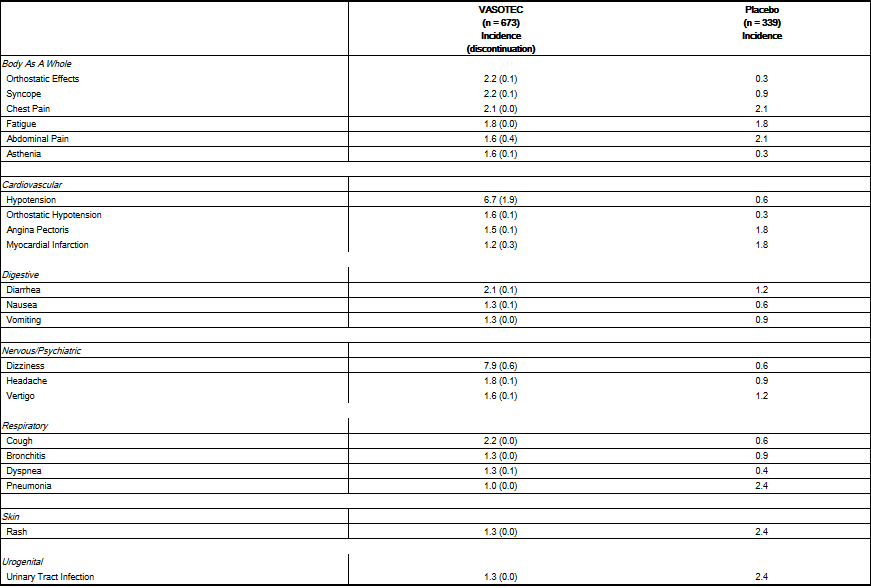
Hypertension
- Adverse experiences occurring in greater than one percent of patients with hypertension treated with enalaprilat in controlled clinical trials are shown below. In patients treated with enalaprilat, the maximum duration of therapy was three years; in placebo treated patients the maximum duration of therapy was 12 weeks.

Heart Failure
- Adverse experiences occurring in greater than one percent of patients with heart failure treated with enalaprilat are shown below. The incidences represent the experiences from both controlled and uncontrolled clinical trials (maximum duration of therapy was approximately one year). In the placebo treated patients, the incidences reported are from the controlled trials (maximum duration of therapy is 12 weeks). The percentage of patients with severe heart failure (NYHA Class IV) was 29 percent and 43 percent for patients treated with enalaprilat and placebo, respectively.
- Other serious clinical adverse experiences occurring since the drug was marketed or adverse experiences occurring in 0.5 to 1.0 percent of patients with hypertension or heart failure in clinical trials are listed below and, within each category, are in order of decreasing severity.
- Body As A Whole: Anaphylactoid reactions.
Cardiovascular
- Cardiac arrest; myocardial infarction or cerebrovascular accident, possibly secondary to excessive hypotension in high risk patients, Hypotension; pulmonary embolism and infarction; pulmonary edema; rhythm disturbances including atrial tachycardia and bradycardia; atrial fibrillation; palpitation, Raynaud's phenomenon.
Digestive
- Ileus, pancreatitis, hepatic failure, hepatitis (hepatocellular [proven on rechallenge] or cholestatic jaundice), melena, anorexia, dyspepsia, constipation, glossitis, stomatitis, dry mouth.
Hematologic
- Rare cases of neutropenia, thrombocytopenia and bone marrow depression.
Musculoskeletal
Nervous/Psychiatric
- Depression, confusion, ataxia, somnolence, insomnia, nervousness, peripheral neuropathy (e.g., paresthesia, dysesthesia), dream abnormality.
Respiratory
- Bronchospasm, rhinorrhea, sore throat and hoarseness, asthma, upper respiratory infection, pulmonary infiltrates, eosinophilic pneumonitis.
Skin
- Exfoliative dermatitis, toxic epidermal necrolysis, Stevens-Johnson syndrome, pemphigus, herpes zoster, erythema multiforme, urticaria, pruritus, alopecia, flushing, diaphoresis, photosensitivity.
Special Senses
- Blurred vision, taste alteration, anosmia, tinnitus, conjunctivitis, dry eyes, tearing.
Urogenital
- Renal failure, oliguria, renal dysfunction, flank pain, gynecomastia, impotence.
Miscellaneous
- A symptom complex has been reported which may include some or all of the following: a positive ANA, an elevated erythrocyte sedimentation rate, arthralgia/arthritis, myalgia/myositis, fever, serositis, vasculitis, leukocytosis, eosinophilia, photosensitivity, rash and other dermatologic manifestations.
Angioedema
- Angioedema has been reported in patients receiving enalaprilat, with an incidence higher in black than in non-black patients. Angioedema associated with laryngeal edema may be fatal. If angioedema of the face, extremities, lips, tongue, glottis and/or larynx occurs, treatment with enalaprilat should be discontinued and appropriate therapy instituted immediately.
Hypotension
- In the hypertensive patients, hypotension occurred in 0.9 percent and syncope occurred in 0.5 percent of patients following the initial dose or during extended therapy. Hypotension or syncope was a cause for discontinuation of therapy in 0.1 percent of hypertensive patients. In heart failure patients, hypotension occurred in 6.7 percent and syncope occurred in 2.2 percent of patients. Hypotension or syncope was a cause for discontinuation of therapy in 1.9 percent of patients with heart failure.
Fetal/Neonatal Morbidity and Mortality
Cough
Pediatric Patients
- The adverse experience profile for pediatric patients appears to be similar to that seen in adult patients.
Clinical Laboratory Test Findings
Serum Electrolytes
Creatinine, Blood Urea Nitrogen
- In controlled clinical trials minor increases in blood urea nitrogen and serum creatinine, reversible upon discontinuation of therapy, were observed in about 0.2 percent of patients with essential hypertension treated with enalaprilat alone. Increases are more likely to occur in patients receiving concomitant diuretics or in patients with renal artery stenosis. In patients with heart failure who were also receiving diuretics with or without digitalis, increases in blood urea nitrogen or serum creatinine, usually reversible upon discontinuation of enalaprilat and/or other concomitant diuretic therapy, were observed in about 11 percent of patients. Increases in blood urea nitrogen or creatinine were a cause for discontinuation in 1.2 percent of patients.
Hematology
- Small decreases in hemoglobin and hematocrit (mean decreases of approximately 0.3 g percent and 1.0 vol percent, respectively) occur frequently in either hypertension or congestive heart failure patients treated with enalaprilat but are rarely of clinical importance unless another cause of anemia coexists. In clinical trials, less than 0.1 percent of patients discontinued therapy due to anemia. Hemolytic anemia, including cases of hemolysis in patients with G-6-PD deficiency, has been reported; a causal relationship to enalapril cannot be excluded.
Liver Function Tests
- Elevations of liver enzymes and/or serum bilirubin have occurred.
|postmarketing=FDA Package Insert for Enalapril maleate contains no information regarding Postmarketing Experience. |drugInteractions=====Hypotension====
Patients on Diuretic Therapy
- Patients on diuretics and especially those in whom diuretic therapy was recently instituted, may occasionally experience an excessive reduction of blood pressure after initiation of therapy with enalapril. The possibility of hypotensive effects with enalapril can be minimized by either discontinuing the diuretic or increasing the salt intake prior to initiation of treatment with enalapril. If it is necessary to continue the diuretic, provide close medical supervision after the initial dose for at least two hours and until blood pressure has stabilized for at least an additional hour.
Agents Causing Renin Release
- The antihypertensive effect of enalaprilat is augmented by antihypertensive agents that cause renin release (e.g., diuretics).
Non-steroidal Anti-inflammatory Agents
- In some patients with compromised renal function who are being treated with non-steroidal anti-inflammatory drugs, the co-administration of enalapril may result in a further deterioration of renal function. These effects are usually reversible.
- In a clinical pharmacology study, indomethacin or sulindac was administered to hypertensive patients receiving enalaprilat. In this study there was no evidence of a blunting of the antihypertensive action of enalaprilat. However, reports suggest that NSAIDs may diminish the antihypertensive effect of ACE inhibitors. This interaction should be given consideration in patients taking NSAIDs concomitantly with ACE inhibitors.
Other Cardiovascular Agents
- Enalaprilat has been used concomitantly with beta adrenergic-blocking agents, methyldopa, nitrates, calcium-blocking agents, hydralazine, prazosin and digoxin without evidence of clinically significant adverse interactions.
Agents Increasing Serum Potassium
- Enalaprilat attenuates potassium loss caused by thiazide-type diuretics. Potassium-sparing diuretics (e.g., spironolactone, triamterene, or amiloride), potassium supplements, or potassium-containing salt substitutes may lead to significant increases in serum potassium. Therefore, if concomitant use of these agents is indicated because of demonstrated hypokalemia, they should be used with caution and with frequent monitoring of serum potassium. Potassium sparing agents should generally not be used in patients with heart failure receiving enalaprilat.
Lithium
- Lithium toxicity has been reported in patients receiving lithium concomitantly with drugs which cause elimination of sodium, including ACE inhibitors. A few cases of lithium toxicity have been reported in patients receiving concomitant enalaprilat and lithium and were reversible upon discontinuation of both drugs. It is recommended that serum lithium levels be monitored frequently if enalapril is administered concomitantly with lithium.
Gold
- Nitritoid reactions (symptoms include facial flushing, nausea, vomiting and hypotension) have been reported rarely in patients on therapy with injectable gold (sodium aurothiomalate) and concomitant ACE inhibitor therapy including enalaprilat.
Carcinogenesis, Mutagenesis, Impairment of Fertility
- There was no evidence of a tumorigenic effect when enalapril was administered for 106 weeks to male and female rats at doses up to 90 mg/kg/day or for 94 weeks to male and female mice at doses up to 90 and 180 mg/kg/day, respectively. These doses are 26 times (in rats and female mice) and 13 times (in male mice) the maximum recommended human daily dose (MRHDD) when compared on a body surface area basis.
- Neither enalapril maleate nor the active diacid was mutagenic in the Ames microbial mutagen test with or without metabolic activation. Enalapril was also negative in the following genotoxicity studies: rec-assay, reverse mutation assay with E. coli, sister chromatid exchange with cultured mammalian cells, and the micronucleus test with mice, as well as in an in vivo cytogenic study using mouse bone marrow.
- There were no adverse effects on reproductive performance of male and female rats treated with up to 90 mg/kg/day of enalapril (26 times the MRHDD when compared on a body surface area basis).
|FDAPregCat=D |useInPregnancyFDA=Use of drugs that act on the renin-angiotensin system during the second and third trimesters of pregnancy reduces fetal renal function and increases fetal and neonatal morbidity and death. Resulting oligohydramnios can be associated with fetal lung hypoplasia and skeletal deformations. Potential neonatal adverse effects include skull hypoplasia, anuria, hypotension, renal failure, and death. When pregnancy is detected, discontinue Enalapril as soon as possible. These adverse outcomes are usually associated with use of these drugs in the second and third trimester of pregnancy. Most epidemiologic studies examining fetal abnormalities after exposure to antihypertensive use in the first trimester have not distinguished drugs affecting the renin-angiotensin system from other antihypertensive agents. Appropriate management of maternal hypertension during pregnancy is important to optimize outcomes for both mother and fetus. In the unusual case that there is no appropriate alternative to therapy with drugs affecting the renin-angiotensin system for a particular patient, apprise the mother of the potential risk to the fetus. Perform serial ultrasound examinations to assess the intra-amniotic environment. If oligohydramnios is observed, discontinue Enalapril, unless it is considered lifesaving for the mother. Fetal testing may be appropriate, based on the week of pregnancy. Patients and physicians should be aware, however, that oligohydramnios may not appear until after the fetus has sustained irreversible injury. Closely observe infants with histories of in utero exposure to Enalapril for hypotension, oliguria, and hyperkalemia. No teratogenic effects of enalapril were seen in studies of pregnant rats and rabbits. On a body surface area basis, the doses used were 57 times and 12 times, respectively, the maximum recommended human daily dose (MRHDD). |useInLaborDelivery=FDA Package Insert for Enalapril maleate contains no information regarding During Labor and Delivery. |useInNursing=FDA Package Insert for Enalapril maleate contains no information regarding During Nursing. |useInPed=* The effects of enalapril maleate as an Antihypertensive have been established in hypertensive pediatric patients age 1 month to 16 years. Use of enalapril maleate in these age groups is supported by evidence from adequate and well-controlled studies of enalapril maleate in pediatric and adult patients as well as by published literature in pediatric patients.
- For pediatric hypertensive patients, the usual recommended starting dose is 0.08 mg/kg (up to 5 mg) once daily. Dosage should be adjusted according to blood pressure response. Doses above 0.58 mg/kg (or in excess of 40 mg) have not been studied in pediatric patients.
- Enalapril maleate is not recommended in neonates and in pediatric patients with glomerular filtration rate less than 30 mL/min/1.73 m2, as no data are available.
|useInGeri=FDA Package Insert for Enalapril maleate contains no information regarding Geriatrics. |useInGender=FDA Package Insert for Enalapril maleate contains no information regarding Gender. |useInRace=FDA Package Insert for Enalapril maleate contains no information regarding Race. |useInRenalImpair=FDA Package Insert for Enalapril maleate contains no information regarding Renal Impairment. |useInHepaticImpair=FDA Package Insert for Enalapril maleate contains no information regarding Hepatic Impairment. |useInReproPotential=FDA Package Insert for Enalapril maleate contains no information regarding Females of Reproductive Potential and Males. |useInImmunocomp=FDA Package Insert for Enalapril maleate contains no information regarding Immunocompromised Patients. |administration=* Preparation of Suspension (for 200 mL of a 1.0 mg/mL suspension)
- Add 50 mL of Bicitra®1 to a polyethylene terephthalate (PET) bottle containing ten 20 mg tablets of VASOTEC and shake for at least 2 minutes. Let concentrate stand for 60 minutes. Following the 60-minute hold time, shake the concentrate for an additional minute. Add 150 mL of Ora-Sweet SF™2 to the concentrate in the PET bottle and shake the suspension to disperse the ingredients. The suspension should be refrigerated at 2-8°C (36-46°F) and can be stored for up to 30 days. Shake the suspension before each use.
|monitoring=FDA Package Insert for Enalapril maleate contains no information regarding Drug Monitoring.
|IVCompat=FDA Package Insert for Enalapril maleate contains no information regarding IV Compatibility.
|overdose=Limited data are available in regard to overdosage in humans.
Single oral doses of enalapril above 1,000 mg/kg and ≥1,775 mg/kg were associated with lethality in mice and rats, respectively.
The most likely manifestation of overdosage would be hypotension, for which the usual treatment would be intravenous infusion of normal saline solution.
Enalaprilat may be removed from general circulation by hemodialysis and has been removed from neonatal circulation by peritoneal dialysis, Anaphylactoid reactions during membrane exposure.
|drugBox={{Drugbox2
| verifiedrevid = 458951007
| IUPAC_name = (2S)-1-[(2S)-2-{[(2S)-1-ethoxy-1-oxo-4-phenylbutan-2-yl]amino}propanoyl]pyrrolidine-2-carboxylic acid
(Diagrams above are enalapril and enalaprilat, respectively. Data below refers to enalapril unless indicated)
| image = Enalapril_drugbox_01.svg.png
| width = 200
| image2 = Enalapril_drugbox_01.png
| tradename = Enalapril | Drugs.com = Monograph | MedlinePlus = a686022 | pregnancy_category = C,D | legal_status = Rx-only | routes_of_administration = I.V. and P.O.
| bioavailability = 60% (oral) | protein_bound = | metabolism = hepatic (to enalaprilat) | elimination_half-life = 11 hours (enalaprilat) | excretion = renal
| CASNo_Ref =
| CAS_number_Ref =
| CAS_number = 75847-73-3
| ATC_prefix = C09
| ATC_suffix = AA02
| ATC_supplemental =
| PubChem = 5388962
| DrugBank_Ref =
| DrugBank = DB00584
| ChemSpiderID_Ref =
| ChemSpiderID = 4534998
| UNII_Ref =
| UNII = 69PN84IO1A
| KEGG_Ref =
| KEGG = D07892
| ChEBI_Ref =
| ChEBI = 4784
| ChEMBL_Ref =
| ChEMBL = 578
| C=20 | H=28 | N=2 | O=5
| molecular_weight = 376.447 g/mol
| smiles = O=C(O)[C@H]2N(C(=O)[C@@H](N[C@H](C(=O)OCC)CCc1ccccc1)C)CCC2
| InChI = 1/C20H28N2O5/c1-3-27-20(26)16(12-11-15-8-5-4-6-9-15)21-14(2)18(23)22-13-7-10-17(22)19(24)25/h4-6,8-9,14,16-17,21H,3,7,10-13H2,1-2H3,(H,24,25)/t14-,16-,17-/m0/s1
| InChIKey = GBXSMTUPTTWBMN-XIRDDKMYBI
| StdInChI_Ref =
| StdInChI = 1S/C20H28N2O5/c1-3-27-20(26)16(12-11-15-8-5-4-6-9-15)21-14(2)18(23)22-13-7-10-17(22)19(24)25/h4-6,8-9,14,16-17,21H,3,7,10-13H2,1-2H3,(H,24,25)/t14-,16-,17-/m0/s1
| StdInChIKey_Ref =
| StdInChIKey = GBXSMTUPTTWBMN-XIRDDKMYSA-N
}}
|mechAction=* Enalapril, after hydrolysis to enalaprilat, inhibits angiotensin-converting enzyme (ACE) in human subjects and animals. ACE is a peptidyl dipeptidase that catalyzes the conversion of angiotensin I to the vasoconstrictor substance, angiotensin II. Angiotensin II also stimulates aldosterone secretion by the adrenal cortex. The beneficial effects of enalapril in hypertension and heart failure appear to result primarily from suppression of the renin-angiotensin-aldosterone system. Inhibition of ACE results in decreased plasma angiotensin II, which leads to decreased vasopressor activity and to decreased aldosterone secretion. Although the latter decrease is small, it results in small increases of serum potassium. In hypertensive patients treated with enalaprilat alone for up to 48 weeks, mean increases in serum potassium of approximately 0.2 mEq/L were observed. In patients treated with enalaprilat plus a thiazide diuretic, there was essentially no change in serum potassium . Removal of angiotensin II negative feedback on renin secretion leads to increased plasma renin activity.
- ACE is identical to kininase, an enzyme that degrades bradykinin. Whether increased levels of bradykinin, a potent vasodepressor peptide, play a role in the therapeutic effects of enalaprilat remains to be elucidated.
- While the mechanism through which enalaprilat lowers blood pressure is believed to be primarily suppression of the renin-angiotensin-aldosterone system, enalaprilat is antihypertensive even in patients with low-renin hypertension. Although enalaprilat was antihypertensive in all races studied, black hypertensive patients (usually a low-renin hypertensive population) had a smaller average response to enalapril monotherapy than non-black patients.
|structure=* Enalapril® (Enalapril Maleate) is the maleate salt of enalapril, the ethyl ester of a long-acting angiotensin converting enzyme inhibitor, enalaprilat. Enalapril maleate is chemically described as (S)-1-[N-[1-(ethoxycarbonyl)-3-phenylpropyl]-L-alanyl]-L-proline, (Z)-2-butenedioate salt (1:1). Its empirical formula is C20H28N2O5•C4H4O4, and its structural formula is:

- Enalapril maleate is a white to off-white, crystalline powder with a molecular weight of 492.53. It is sparingly soluble in water, soluble in ethanol, and freely soluble in methanol.
- Enalapril is a pro-drug; following oral administration, it is bioactivated by hydrolysis of the ethyl ester to enalaprilat, which is the active angiotensin converting enzyme inhibitor.
- Enalapril maleate is supplied as 2.5 mg, 5 mg, 10 mg, and 20 mg tablets for oral administration. In addition to the active ingredient enalapril maleate, each tablet contains the following inactive ingredients: lactose, magnesium stearate, sodium bicarbonate, and starch. The 10 mg and 20 mg tablets also contain iron oxides.
|PD=* Administration of enalaprilat to patients with hypertension of severity ranging from mild to severe results in a reduction of both supine and standing blood pressure usually with no orthostatic component. Symptomatic postural hypotension is therefore infrequent, although it might be anticipated in volume-depleted patients.
- In most patients studied, after oral administration of a single dose of enalapril, onset of antihypertensive activity was seen at one hour with peak reduction of blood pressure achieved by four to six hours.
- At recommended doses, antihypertensive effects have been maintained for at least 24 hours. In some patients the effects may diminish toward the end of the dosing interval.
- In some patients achievement of optimal blood pressure reduction may require several weeks of therapy.
- The antihypertensive effects of enalaprilat have continued during long term therapy. Abrupt withdrawal of enalaprilat has not been associated with a rapid increase in blood pressure.
- In hemodynamic studies in patients with essential hypertension, blood pressure reduction was accompanied by a reduction in peripheral arterial resistance with an increase in cardiac output and little or no change in heart rate. Following administration of enalaprilat, there is an increase in renal blood flow; glomerular filtration rate is usually unchanged. The effects appear to be similar in patients with renovascular hypertension.
- When given together with thiazide-type diuretics, the blood pressure lowering effects of enalaprilat are approximately additive.
|PK=* Following oral administration of vasotc, peak serum concentrations of enalapril occur within about one hour. Based on urinary recovery, the extent of absorption of enalapril is approximately 60 percent. Enalapril absorption is not influenced by the presence of food in the gastrointestinal tract. Following absorption, enalapril is hydrolyzed to enalaprilat, which is a more potent angiotensin converting enzyme inhibitor than enalapril; enalaprilat is poorly absorbed when administered orally. Peak serum concentrations of enalaprilat occur three to four hours after an oral dose of enalapril maleate. Excretion of Enalapril is primarily renal. Approximately 94 percent of the dose is recovered in the urine and feces as enalaprilat or enalapril. The principal components in urine are enalaprilat, accounting for about 40 percent of the dose, and intact enalapril. There is no evidence of metabolites of enalapril, other than enalaprilat.
- The serum concentration profile of enalaprilat exhibits a prolonged terminal phase, apparently representing a small fraction of the administered dose that has been bound to ACE. The amount bound does not increase with dose, indicating a saturable site of binding. The effective half-life for accumulation of enalaprilat following multiple doses of enalapril maleate is 11 hours.
- The disposition of enalapril and enalaprilat in patients with renal insufficiency is similar to that in patients with normal renal function until the glomerular filtration rate is 30 mL/min or less. With glomerular filtration rate ≤30 mL/min, peak and trough enalaprilat levels increase, time to peak concentration increases and time to steady state may be delayed. The effective half-life of enalaprilat following multiple doses of enalapril maleate is prolonged at this level of renal insufficiency. Enalaprilat is dialyzable at the rate of 62 mL/min.
- Studies in dogs indicate that enalapril crosses the blood-brain barrier poorly, if at all; enalaprilat does not enter the brain. Multiple doses of enalapril maleate in rats do not result in accumulation in any tissues. Milk of lactating rats contains radioactivity following administration of 14C-enalapril maleate. Radioactivity was found to cross the placenta following administration of labeled drug to pregnant hamsters.
|nonClinToxic=There was no evidence of a tumorigenic effect when enalapril was administered for 106 weeks to male and female rats at doses up to 90 mg/kg/day or for 94 weeks to male and female mice at doses up to 90 and 180 mg/kg/day, respectively. These doses are 26 times (in rats and female mice) and 13 times (in male mice) the maximum recommended human daily dose (MRHDD) when compared on a body surface area basis. Neither enalapril maleate nor the active diacid was mutagenic in the Ames microbial mutagen test with or without metabolic activation. Enalapril was also negative in the following genotoxicity studies: rec-assay, reverse mutation assay with E. coli, sister chromatid exchange with cultured mammalian cells, and the micronucleus test with mice, as well as in an in vivo cytogenic study using mouse bone marrow. There were no adverse effects on reproductive performance of male and female rats treated with up to 90 mg/kg/day of enalapril (26 times the MRHDD when compared on a body surface area basis). |clinicalStudies======heart failure=====
- In trials in patients treated with digitalis and diuretics, treatment with enalapril resulted in decreased systemic vascular resistance, blood pressure, pulmonary capillary wedge pressure and heart size, and increased cardiac output and exercise tolerance. Heart rate was unchanged or slightly reduced, and mean ejection fraction was unchanged or increased. There was a beneficial effect on severity of heart failure as measured by the New York Heart Association (NYHA) classification and on symptoms of dyspnea and fatigue. Hemodynamic effects were observed after the first dose, and appeared to be maintained in uncontrolled studies lasting as long as four months. Effects on exercise tolerance, heart size, and severity and symptoms of heart failure were observed in placebo-controlled studies lasting from eight weeks to over one year.
- Enalapril is indicated for the treatment of symptomatic heart failure, usually in combination with diuretics and digitalis. In the placebo-controlled studies that demonstrated improved survival, patients were titrated as tolerated up to 40 mg, administered in two divided doses.
- The recommended initial dose is 2.5 mg. The recommended dosing range is 2.5 to 20 mg given twice a day. Doses should be titrated upward, as tolerated, over a period of a few days or weeks. The maximum daily dose administered in clinical trials was 40 mg in divided doses.
- After the initial dose of Enalapril, the patient should be observed under medical supervision for at least two hours and until blood pressure has stabilized for at least an additional hour. If possible, the dose of any concomitant diuretic should be reduced which may diminish the likelihood of hypotension. The appearance of hypotension after the initial dose of Enalapril does not preclude subsequent careful dose titration with the drug, following effective management of the hypotension.
heart failure, Mortality Trials
- In a multicenter, placebo-controlled clinical trial, 2,569 patients with all degrees of symptomatic heart failure and ejection fraction ≤35 percent were randomized to placebo or enalapril and followed for up to 55 months (SOLVD-Treatment). Use of enalapril was associated with an 11 percent reduction in all-cause mortality and a 30 percent reduction in hospitalization for heart failure. Diseases that excluded patients from enrollment in the study included severe stable angina (>2 attacks/day), hemodynamically significant valvular or outflow tract obstruction, renal failure (creatinine >2.5 mg/dL), cerebral vascular disease (e.g., significant carotid artery disease), advanced pulmonary disease, malignancies, active myocarditis and constrictive pericarditis. The mortality benefit associated with enalapril does not appear to depend upon digitalis being present.
- A second multicenter trial used the SOLVD protocol for study of asymptomatic or minimally symptomatic patients. SOLVD-Prevention patients, who had left ventricular ejection fraction ≤35% and no history of symptomatic heart failure, were randomized to placebo (n=2117) or enalapril (n=2111) and followed for up to 5 years. The majority of patients in the SOLVD-Prevention trial had a history of ischemic heart disease. A history of myocardial infarction was present in 80 percent of patients, current angina pectoris in 34 percent, and a history of hypertension in 37 percent. No statistically significant mortality effect was demonstrated in this population. Enalapril-treated subjects had 32% fewer first hospitalizations for heart failure, and 32% fewer total heart failure hospitalizations. Compared to placebo, 32 percent fewer patients receiving enalapril developed symptoms of overt heart failure. Hospitalizations for cardiovascular reasons were also reduced. There was an insignificant reduction in hospitalizations for any cause in the enalapril treatment group (for enalapril vs. placebo, respectively, 1166 vs. 1201 first hospitalizations, 2649 vs. 2840 total hospitalizations), although the study was not powered to look for such an effect.
- The SOLVD-Prevention trial was not designed to determine whether treatment of asymptomatic patients with low ejection fraction would be superior, with respect to preventing hospitalization, to closer follow-up and use of enalapril at the earliest sign of heart failure. However, under the conditions of follow-up in the SOLVD-Prevention trial (every 4 months at the study clinic; personal physician as needed), 68% of patients on placebo who were hospitalized for heart failure had no prior symptoms recorded which would have signaled initiation of treatment.
- The SOLVD-Prevention trial was also not designed to show whether enalapril modified the progression of underlying heart disease.
- In another multicenter, placebo-controlled trial (CONSENSUS) limited to patients with NYHA Class IV congestive heart failure and radiographic evidence of cardiomegaly, use of enalapril was associated with improved survival. The results are shown in the following table.
Hypertension
- In clinical studies in hypertensive patients with unilateral or bilateral renal artery stenosis, increases in blood urea nitrogen and serum creatinine were observed in 20 percent of patients. These increases were almost always reversible upon discontinuation of enalapril and/or diuretic therapy. In such patients renal function should be monitored during the first few weeks of therapy.
Clinical Pharmacology in Pediatric Patients
- A multiple dose pharmacokinetic study was conducted in 40 hypertensive male and female pediatric patients aged 2 months to ≤16 years following daily oral administration of 0.07 to 0.14 mg/kg enalapril maleate. At steady state, the mean effective half-life for accumulation of enalaprilat was 14 hours and the mean urinary recovery of total enalapril and enalaprilat in 24 hours was 68% of the administered dose. Conversion of enalapril to enalaprilat was in the range of 63-76%. The overall results of this study indicate that the pharmacokinetics of enalapril in hypertensive children aged 2 months to ≤16 years are consistent across the studied age groups and consistent with pharmacokinetic historic data in healthy adults.
- In a clinical study involving 110 hypertensive pediatric patients 6 to 16 years of age, patients who weighed <50 kg received either 0.625, 2.5 or 20 mg of enalapril daily and patients who weighed ≥50 kg received either 1.25, 5, or 40 mg of enalapril daily. Enalapril administration once daily lowered trough blood pressure in a dose-dependent manner. The dose-dependent antihypertensive efficacy of enalapril was consistent across all subgroups (age, Tanner stage, gender, race). However, the lowest doses studied, 0.625 mg and 1.25 mg, corresponding to an average of 0.02 mg/kg once daily, did not appear to offer consistent antihypertensive efficacy. In this study, Enalapril was generally well tolerated.
- In the above pediatric studies, enalapril maleate was given as tablets of Enalapril and for those children and infants who were unable to swallow tablets or who required a lower dose than is available in tablet form, enalapril was administered in a suspension formulation
|howSupplied=* VASOTEC Tablets, 2.5 mg, are white, oval shaped tablet imprinted with "VASO 2.5" and scored on one side and scored on the other.
- They are supplied as follows:
- NDC 0187-0140-30 bottles of 30 (with desiccant)
- NDC 0187-0140-90 unit of use bottles of 90 (with desiccant)
- VASOTEC Tablets, 5 mg, are white, rounded triangle shaped tablet imprinted with "VASO 5" on one side and scored on the other.
- They are supplied as follows:
- NDC 0187-0141-30 bottles of 30 (with desiccant)
- NDC 0187-0141-90 unit of use bottles of 90 (with desiccant)
- NDC 0187-0141-10 bottles of 1,000 (with desiccant)
- VASOTEC Tablets, 10 mg, are rust red, rounded triangle shaped tablet imprinted with "VASO 10" on one side and scored on the other.
- They are supplied as follows:
- NDC 0187-0142-30 bottles of 30 (with desiccant)
- NDC 0187-0142-90 unit of use bottles of 90 (with desiccant)
- NDC 0187-0142-10 bottles of 1,000 (with desiccant)
- VASOTEC Tablets, 20 mg, are peach, rounded triangle shaped tablet imprinted with "VASO 20" on one side and scored on the other.
- They are supplied as follows:
- NDC 0187-0143-30 bottles of 30 (with desiccant)
- NDC 0187-0143-90 unit of use bottles of 90 (with desiccant)
- NDC 0187-0143-10 bottles of 1,000 (with desiccant)
|storage=* Store at 25°C (77°F); excursions permitted to 15-30°C (59-86°F) [see USP Controlled Room Temperature].
- Keep container tightly closed.
- Protect from moisture.
- Dispense in a tight container as per USP, if product package is subdivided.
|fdaPatientInfo=* Angioedema:
- Angioedema, including laryngeal edema, may occur at any time during treatment with angiotensin converting enzyme inhibitors, including enalapril. Patients should be so advised and told to report immediately any signs or symptoms suggesting angioedema (swelling of face, extremities, eyes, lips, tongue, difficulty in swallowing or breathing) and to take no more drug until they have consulted with the prescribing physician.
- Hypotension:
- Patients should be cautioned to report lightheadedness, especially during the first few days of therapy. If actual syncope occurs, the patients should be told to discontinue the drug until they have consulted with the prescribing physician. All patients should be cautioned that excessive perspiration and dehydration may lead to an excessive fall in blood pressure because of reduction in fluid volume. Other causes of volume depletion such as vomiting or diarrhea may also lead to a fall in blood pressure; patients should be advised to consult with the physician.
- Hyperkalemia:
- Patients should be told not to use salt substitutes containing potassium without consulting their physician.
- Neutropenia:
- Patients should be told to report promptly any indication of infection (e.g., sore throat, fever) which may be a sign of neutropenia.
- Pregnancy:
- Female patients of childbearing age should be told about the consequences of exposure to Enalapril during pregnancy. Discuss treatment options with women planning to become pregnant. Patients should be asked to report pregnancies to their physicians as soon as possible.
- NOTE: As with many other drugs, certain advice to patients being treated with enalapril is warranted. This information is intended to aid in the safe and effective use of this medication. It is not a disclosure of all possible adverse or intended effects.
|alcohol=Alcohol-Enalapril tablet interaction has not been established. Talk to your doctor about the effects of taking alcohol with this medication. |lookAlike=There is limited information about the Look-Alike Drug Names. |price=lactose, magnesium stearate, sodium stearate, sodium bicarbonate, starch, corn }} {{#subobject:
|Page Name=Enalapril maleate |Pill Name=No_image.jpg |Drug Name=Vasotec 2.5 MG Oral Tablet |Pill Ingred=lactose, magnesium stearate, sodium stearate, sodium bicarbonate, starch, corn|+sep=; |Pill Imprint=VASO;2;5 |Pill Dosage=2.5 mg |Pill Color=White|+sep=; |Pill Shape=Oval |Pill Size (mm)=6.00 |Pill Scoring=2 |Pill Image= |Drug Author=Valeant Pharmaceuticals North America LLC |NDC=0187-0140
}}
{{#subobject:
|Label Page=Enalapril maleate |Label Name=Enalapril_label_01.jpg
}}
{{#subobject:
|Label Page=Enalapril maleate |Label Name=Enalapril_label_02.jpg
}}
{{#subobject:
|Label Page=Enalapril maleate |Label Name=Enalapril_label_03.jpg
}}
{{#subobject:
|Label Page=Enalapril maleate |Label Name=Enalapril_label_04.jpg
}}
{{#subobject:
|Label Page=Enalapril maleate |Label Name=Enalapril_panel_01.jpg
}}
{{#subobject:
|Label Page=Enalapril maleate |Label Name=Enalapril_panel_02.jpg
}}
{{#subobject:
|Label Page=Enalapril maleate |Label Name=Enalapril_panel_03.jpg
}}
{{#subobject:
|Label Page=Enalapril maleate |Label Name=Enalapril_panel_04.jpg
}}
- ↑ Cardinale D, Colombo A, Lamantia G, Colombo N, Civelli M, De Giacomi G; et al. (2010). "Anthracycline-induced cardiomyopathy: clinical relevance and response to pharmacologic therapy". J Am Coll Cardiol. 55 (3): 213–20. doi:10.1016/j.jacc.2009.03.095. PMID 20117401.
- ↑ Evangelista A, Tornos P, Sambola A, Permanyer-Miralda G, Soler-Soler J (2005). "Long-term vasodilator therapy in patients with severe aortic regurgitation". N Engl J Med. 353 (13): 1342–9. doi:10.1056/NEJMoa050666. PMID 16192479.
- ↑ Lin M, Chiang HT, Lin SL, Chang MS, Chiang BN, Kuo HW; et al. (1994). "Vasodilator therapy in chronic asymptomatic aortic regurgitation: enalapril versus hydralazine therapy". J Am Coll Cardiol. 24 (4): 1046–53. PMID 7930196.
- ↑ Saleh AE (1993). "Angiotensin-converting-enzyme inhibitors and chyluria". Ann Intern Med. 119 (12): 1223–4. PMID 8239259.
- ↑ Vermes E, Ducharme A, Bourassa MG, Lessard M, White M, Tardif JC; et al. (2003). "Enalapril reduces the incidence of diabetes in patients with chronic heart failure: insight from the Studies Of Left Ventricular Dysfunction (SOLVD)". Circulation. 107 (9): 1291–6. PMID 12628950. Review in: ACP J Club. 2003 Nov-Dec;139(3):68
- ↑ Ravid M, Savin H, Jutrin I, Bental T, Lang R, Lishner M (1994). "Long-term effect of ACE inhibition on development of nephropathy in diabetes mellitus type II". Kidney Int Suppl. 45: S161–4. PMID 8158887.
- ↑ Ravid M, Brosh D, Levi Z, Bar-Dayan Y, Ravid D, Rachmani R (1998). "Use of enalapril to attenuate decline in renal function in normotensive, normoalbuminuric patients with type 2 diabetes mellitus. A randomized, controlled trial". Ann Intern Med. 128 (12 Pt 1): 982–8. PMID 9625684.
- ↑ Ahmad J, Siddiqui MA, Ahmad H (1997). "Effective postponement of diabetic nephropathy with enalapril in normotensive type 2 diabetic patients with microalbuminuria". Diabetes Care. 20 (10): 1576–81. PMID 9314638.
- ↑ Capes SE, Gerstein HC, Negassa A, Yusuf S (2000). "Enalapril prevents clinical proteinuria in diabetic patients with low ejection fraction". Diabetes Care. 23 (3): 377–80. PMID 10868869.
- ↑ Ueng KC, Tsai TP, Yu WC, Tsai CF, Lin MC, Chan KC; et al. (2003). "Use of enalapril to facilitate sinus rhythm maintenance after external cardioversion of long-standing persistent atrial fibrillation. Results of a prospective and controlled study". Eur Heart J. 24 (23): 2090–8. PMID 14643269.
- ↑ Javid R, Ghahramani N, Malek-Hosseini SA, Behzadi S, Rais-Jalali GA (1999). "Management of posttransplant erythrocytosis with enalapril". Transplant Proc. 31 (8): 3226. PMID 10616453.
- ↑ Usalan C, Erdem Y, Cağlar M, Altun B, Arici M, Bakkaloğlu M; et al. (1998). "Effect of enalapril on exaggerated erythropoietin response to phlebotomy in erythrocytosic renal transplant patients". Nephrol Dial Transplant. 13 (11): 2884–9. PMID 9829495.
- ↑ Montanaro D, Gropuzzo M, Tulissi P, Boscutti G, Risaliti A, Baccarani U; et al. (2001). "Angiotensin-converting enzyme inhibitors reduce hemoglobin concentrations, hematocrit, and serum erythropoietin levels in renal transplant recipients without posttransplant erythrocytosis". Transplant Proc. 33 (1–2): 2038–40. PMID 11267615.
- ↑ Vargas M, Leon-Velarde F, Monge-C C, Orozco E, Rey L (1996). "Enalapril in the treatment of chronic mountain sickness". Wilderness Environ Med. 7 (2): 193–4. PMID 11990112.
- ↑ Esnault VL, Brown EA, Apetrei E, Bagon J, Calvo C, DeChatel R; et al. (2008). "The effects of amlodipine and enalapril on renal function in adults with hypertension and nondiabetic nephropathies: a 3-year, randomized, multicenter, double-blind, placebo-controlled study". Clin Ther. 30 (3): 482–98. doi:10.1016/j.clinthera.2008.03.006. PMID 18405787.
- ↑ van Dijk MA, Breuning MH, Duiser R, van Es LA, Westendorp RG (2003). "No effect of enalapril on progression in autosomal dominant polycystic kidney disease". Nephrol Dial Transplant. 18 (11): 2314–20. PMID 14551359.
- ↑ Midtvedt K, Stokke ES, Hartmann A (1996). "Successful long-term treatment of post-transplant erythrocytosis with losartan". Nephrol Dial Transplant. 11 (12): 2495–7. PMID 9017632.
- ↑ Takahashi F, Ogawa Y, Hasebe N, Natori S, Tokusashi Y, Miyokawa N; et al. (2000). "Successful treatment of a patient with nephrotic syndrome associated with chronic lymphocytic leukemia". Intern Med. 39 (3): 256–9. PMID 10772132.
- ↑ Webb NJ, Shahinfar S, Wells TG, Massaad R, Gleim GW, McCrary Sisk C; et al. (2013). "Losartan and enalapril are comparable in reducing proteinuria in children with Alport syndrome". Pediatr Nephrol. 28 (5): 737–43. doi:10.1007/s00467-012-2372-9. PMID 23207876.
- ↑ Silber JH, Cnaan A, Clark BJ, Paridon SM, Chin AJ, Rychik J; et al. (2004). "Enalapril to prevent cardiac function decline in long-term survivors of pediatric cancer exposed to anthracyclines". J Clin Oncol. 22 (5): 820–8. doi:10.1200/JCO.2004.06.022. PMID 14990637.
- ↑ Yüksel H, Darcan S, Kabasakal C, Cura A, Mir S, Mavi E (1998). "Effect of enalapril on proteinuria, phosphaturia, and calciuria in insulin-dependent diabetes". Pediatr Nephrol. 12 (8): 648–50. PMID 9811387.
- ↑ Proesmans W, Van Dyck M (2004). "Enalapril in children with Alport syndrome". Pediatr Nephrol. 19 (3): 271–5. doi:10.1007/s00467-003-1366-z. PMID 14745635.
- ↑ Bender WI (1995). "ACE inhibitors for prophylaxis of migraine headaches". Headache. 35 (8): 470–1. PMID 7591740.
- ↑ "Effects of enalapril on left ventricular function and exercise performance after a first acute myocardial infarction. The EDEN Study Investigators". Int J Cardiol. 59 (3): 257–65. 1997. PMID 9183041.
- ↑ Zeng C, Zhu Z, Liu G, Hu W, Wang X, Yang C; et al. (1998). "Randomized, double-blind, placebo-controlled trial of oral enalapril in patients with neurally mediated syncope". Am Heart J. 136 (5): 852–8. PMID 9812081.
- ↑ "The Canadian abortion law". Can Med Assoc J. 116 (3): 238, 241, 243–50. 1977. PMC 1878951. PMID 837300.