Drug-Eluting Stent Thrombosis More Than Seven Years After Implantation: Pathophysiology of “Very” Very Late Stent Thrombosis Elucidated by Optical Coherence Tomography and Histological Analysis: Difference between revisions
Tarek Nafee (talk | contribs) |
Tarek Nafee (talk | contribs) |
||
| Line 15: | Line 15: | ||
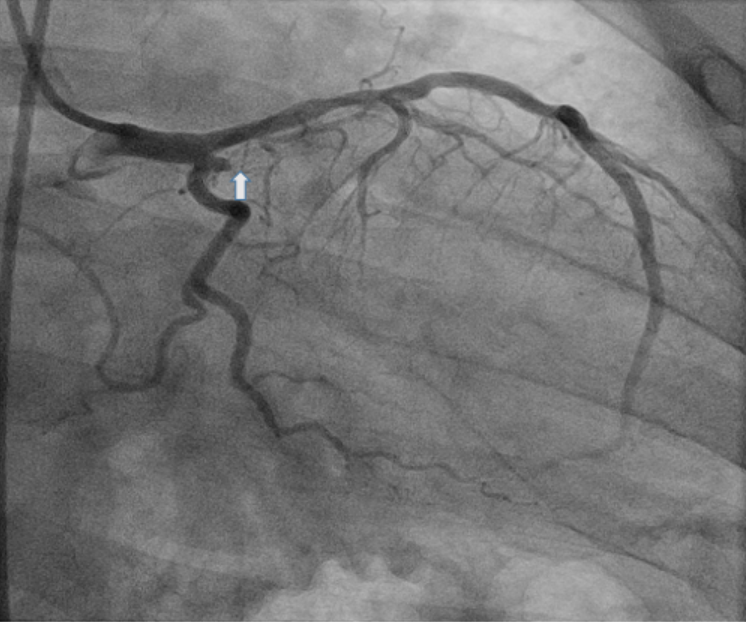
File:10003_1.png|'''Figure 1.''' Coronary angiography demonstrates the total occlusion (arrow) of the first obtuse marginal branch 86 months after placement of a Sirolimus eluting-stent. | File:10003_1.png|'''Figure 1.''' Coronary angiography demonstrates the total occlusion (arrow) of the first obtuse marginal branch 86 months after placement of a Sirolimus eluting-stent. | ||
File:10003_2.png|'''Figure 2.''' OCT demonstrating large white thrombus (blue arrows) and focal areas of stent malposition (green arrows) | File:10003_2.png|'''Figure 2.''' OCT demonstrating large white thrombus (blue arrows) and focal areas of stent malposition (green arrows) | ||
File:10003_3.png|'''Figure 3 | File:10003_3.png|'''Figure 3. A-D''' Platelet-rich thrombus. A) Thrombus Aspirate B) Low power H & E (10X) photomicrograph showing red blood cells and finely granular eosinphilic platelets. C) Higher power H &E (40X) photomicrograph D) Immunohistochemical stain for CD61, documenting the abundance of platelets. | ||
File:10003_4.png|'''Figure 4.''' Final angiographic result after thrombectomy and balloon angioplasty. | |||
</gallery> | </gallery> | ||
Revision as of 14:45, 19 September 2018
Click here to go back to the Tweetbook
Click here to read more about stent thrombosis
Authors
Alec Vishnevsky, MD (@AVishnevsky_MD)1; Antony Kaliyadan, MD1; David L. Fischman, MD (@fischman_david)1; Nicholas J. Reuggiero II, MD (@DrNickTJU)1; John Farber, MD1; Michael P. Savage, MD1
1From the Department of Medicine, Division of Cardiology, Sidney Kimmel Medical College at Thomas Jefferson University, Thomas Jefferson University Hospital, Philadelphia, PA
Case
Stent thrombosis remains a serious complication of percutaneous coronary intervention (PCI) resulting in myocardial infarction (MI) or death in up to 80% of patients.1–3 Thrombosis occurring more than one year after PCI is classified as very late stent thrombosis (VLST). It remains unknown whether the risk of DES thrombosis eventually abates over time or persists indefinitely. Recently a series of patients with “very” very late stent thrombosis occurring more than 5 years after implantation has been reported4. In this imaging case report, we present a case of VLST occurring more than 7 years after stent implantation; optical coherence tomography (OCT) and histopathological analysis was performed to elucidate the pathophysiology of this event. A 58-year-old male presented to our emergency department with five hours of chest pain. The patient had a history of non-ST elevation myocardial infarction with placement of a Sirolimus-eluting stent seven years and two months previously. The patient admitted to self-discontinuation of his medications, including a baby aspirin, and had resumed smoking. ECG revealed acute postero-lateral ST elevation MI. Emergent coronary angiography revealed a 100% thrombotic occlusion in the first obtuse marginal branch at the site of the previous SES (Figure 1). After flow was re-established with aspiration thrombectomy, OCT was performed (Figure 2). Histologic analysis of the aspirated material demonstrated a large thrombus characterized by dense platelet aggregates (Figure 3). Noteable was the absence of neoatherosclerosis. Following additional thrombectomy and balloon angioplasty, there was an excellent angiographic appearance (Figure 4).
Figures
-
Figure 1. Coronary angiography demonstrates the total occlusion (arrow) of the first obtuse marginal branch 86 months after placement of a Sirolimus eluting-stent.
-
Figure 2. OCT demonstrating large white thrombus (blue arrows) and focal areas of stent malposition (green arrows)
-
Figure 3. A-D Platelet-rich thrombus. A) Thrombus Aspirate B) Low power H & E (10X) photomicrograph showing red blood cells and finely granular eosinphilic platelets. C) Higher power H &E (40X) photomicrograph D) Immunohistochemical stain for CD61, documenting the abundance of platelets.
-
Figure 4. Final angiographic result after thrombectomy and balloon angioplasty.
Comments
We demonstrate a case of “very” very late stent thrombosis 7 years after initial implantation due to non-compliance with aspirin and smoking cessation. OCT proved critical for elucidating the pathophysiology of this thrombotic event, demonstrating massive white thrombus and focal areas of stent strut malposition.