Dengue fever physical examination
|
Dengue Fever Microchapters |
|
Diagnosis |
|---|
|
Treatment |
|
Case Studies |
|
Dengue fever physical examination On the Web |
|
American Roentgen Ray Society Images of Dengue fever physical examination |
|
Risk calculators and risk factors for Dengue fever physical examination |
Editor-In-Chief: C. Michael Gibson, M.S., M.D. [1]
Overview
The typical signs of Dengue Fever include a high fever with no localizing source of infection on physical examination. Occasionally petechia are present. The physical examination in Dengue fever should be directed toward identifying warning signs that the patient has or may develop severe disease warranting in-hospital observation and/or intensive treatment. These warning signs include tachycardia, postural hypotension, a narrow pulse pressure (<20 mm Hg) and / or frank hypotension could indicate intravascular volume depletion due to either dehydration or capillary leak; petechia, lethargy, restlessness, mucosal bleeding, pleural effusion, ascites, hepatomegaly, abdominal tenderness and pedal edema.[1]
Vital Signs
Pulse and Blood Pressure
Tachycardia, postural hypotension, a narrow pulse pressure (<20 mm Hg) and / or frank hypotension could indicate intravascular volume depletion due to either dehydration or capillary leak. The presence of any of the above is a warning sign of severe disease, and the patient should be hospitalized for observation.
Urine Output
If the patient is not urinating at least every 6 hours, this may reflect intravascular volume depletion due to capillary leak, and the patient should be observed for the development of severe disease.
Skin
If the patient has poor perfusion, the skin may be cold and clammy.
Erythema of face, maculopapular rash and Petechiae may be present.[2] The tourniquet test can used to elicit petechia. A blood pressure cuff is applied and inflated to a point between the systolic and diastolic blood pressures for five minutes. The test is positive if there are more than 20 petechiae per square inch (a petechia is a small red or purple spot on the body, caused by a minor hemorrhage).
-
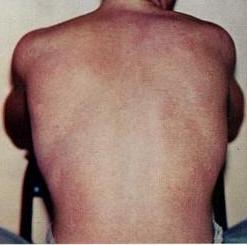
The above picture is a rash typically associated with Dengue fever. Source: CDC
Mental Status
Lethargy and restlessness are warning signs that the patient should be monitored for the development of severe disease.
HEENT
- Mucosal bleeding is a warning sign that the patient may have thrombocytopenia, and should be monitored for the development of severe disease.
- Pharyngeal inflamation
- Retinal hemorrhage may occur.[3]
Lungs
- Pleural effusion is a warning sign the capillary leak may be occurring and that the patient should be monitored for the development of severe disease.
Abdomen
- Abdominal pain or tenderness are warning signs and the patient should be monitored for the development of severe disease.
- Liver enlargment >2 cm is a warning signs and the patient should be monitored for the development of severe disease.
- Ascites is a warning sign and the patient should be monitored for the development of severe disease.
Extremities
- Pedal edema or evidence of fluid accumulation is a warning sign and the patient should be monitored for the development of severe disease.
References
- ↑ "Dengue: guidelines for diagnosis, treatment, prevention and control" (PDF).
- ↑ Thomas EA, John M, Kanish B (2010). "Mucocutaneous manifestations of Dengue fever". Indian J Dermatol. 55 (1): 79–85. doi:10.4103/0019-5154.60359. PMC 2856380. PMID 20418984.
- ↑ Loh BK, Bacsal K, Chee SP, Cheng BC, Wong D (2008). "Foveolitis associated with dengue Fever: a case series". Ophthalmologica. 222 (5): 317–20. doi:10.1159/000144074. PMID 18617754.