Dabrafenib mesylate
Editor-In-Chief: C. Michael Gibson, M.S., M.D. [1]; Associate Editor(s)-in-Chief: Kiran Singh, M.D. [2]
Disclaimer
WikiDoc MAKES NO GUARANTEE OF VALIDITY. WikiDoc is not a professional health care provider, nor is it a suitable replacement for a licensed healthcare provider. WikiDoc is intended to be an educational tool, not a tool for any form of healthcare delivery. The educational content on WikiDoc drug pages is based upon the FDA package insert, National Library of Medicine content and practice guidelines / consensus statements. WikiDoc does not promote the administration of any medication or device that is not consistent with its labeling. Please read our full disclaimer here.
Overview
Dabrafenib mesylate is a BRAF Inhibitor that is FDA approved for the treatment of malignant melanoma. Common adverse reactions include peripheral edema, alopecia, hyperkeratosis, abdominal pain, constipation, anemia, arthralgia, cough.
Adult Indications and Dosage
FDA-Labeled Indications and Dosage (Adult)
Indications
BRAF V600E Mutation-Positive Unresectable or Metastatic Melanoma
- Dabrafenib mesylate as a single agent is indicated for the treatment of patients with unresectable or metastatic melanoma with BRAF V600E mutation as detected by an FDA-approved test.
BRAF V600E or V600K Mutation-Positive Unresectable or Metastatic Melanoma
- Dabrafenib mesylate, in combination with trametinib, is indicated for the treatment of patients with unresectable or metastatic melanoma with BRAF V600E or V600K mutations, as detected by an FDA-approved test. This indication is based on the demonstration of durable response rate. Improvement in disease-related symptoms or overall survival has not been demonstrated for dabrafenib mesylate in combination with trametinib.
Limitation of Use
- Dabrafenib mesylate is not indicated for treatment of patients with wild-type BRAF melanoma.
Dosing
Recommended Dosing
- The recommended dosage regimens of Dabrafenib mesylate are:
- 150 mg orally taken twice daily, approximately 12 hours apart, as a single agent
- 150 mg orally taken twice daily, approximately 12 hours apart, in combination with trametinib 2 mg orally taken once daily
- Continue treatment until disease progression or unacceptable toxicity occurs. Take dabrafenib mesylate as a single agent, or dabrafenib mesylate in combination with trametinib, at least 1 hour before or 2 hours after a meal. Do not take a missed dose of dabrafenib mesylate within 6 hours of the next dose of dabrafenib mesylate. Do not open, crush, or break dabrafenib mesylate capsule.
- When administered in combination with trametinib, take the once-daily dose of trametinib at the same time each day with either the morning dose or the evening dose of dabrafenib mesylate.
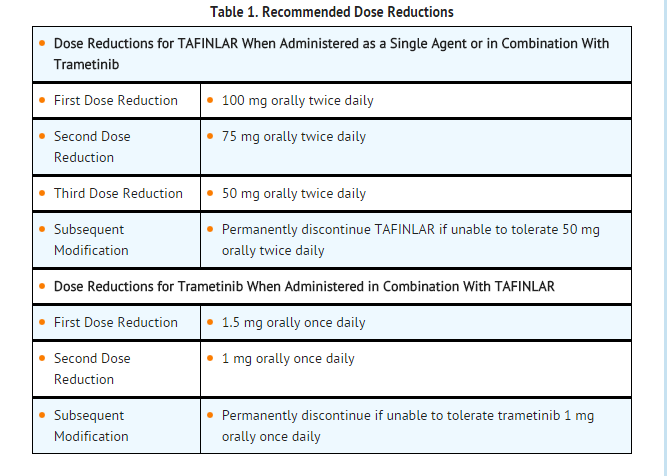
Dose Modifications
- For New Primary Cutaneous Malignancies: No dose modifications are required.
- For New Primary Non-Cutaneous Malignancies: Permanently discontinue dabrafenib mesylate in patients who develop RAS mutation-positive non-cutaneous malignancies. If used in combination with trametinib, no dose modifications are required for trametinib in patients who develop non-cutaneous malignancies.

DOSAGE FORMS AND STRENGTHS
- 50 mg Capsules: Dark red capsule imprinted with ‘GS TEW’ and ‘50 mg’.
- 75 mg Capsules: Dark pink capsule imprinted with ‘GS LHF’ and ‘75 mg’.
Off-Label Use and Dosage (Adult)
Guideline-Supported Use
There is limited information regarding Off-Label Guideline-Supported Use of Dabrafenib mesylate in adult patients.
Non–Guideline-Supported Use
There is limited information regarding Off-Label Non–Guideline-Supported Use of Dabrafenib mesylate in adult patients.
Pediatric Indications and Dosage
FDA-Labeled Indications and Dosage (Pediatric)
There is limited information regarding FDA-Labeled Use of Dabrafenib mesylate in pediatric patients.
Off-Label Use and Dosage (Pediatric)
Guideline-Supported Use
There is limited information regarding Off-Label Guideline-Supported Use of Dabrafenib mesylate in pediatric patients.
Non–Guideline-Supported Use
There is limited information regarding Off-Label Non–Guideline-Supported Use of Dabrafenib mesylate in pediatric patients.
Contraindications
- None
Warnings
- Review the Full Prescribing Information for trametinib prior to initiation of dabrafenib mesylate in combination with trametinib. The following serious adverse reactions of trametinib as a single agent, which may occur when dabrafenib mesylate is used in combination with trametinib, are not described in the Full Prescribing Information for dabrafenib mesylate:
New Primary Malignancies
- New primary malignancies, cutaneous and non-cutaneous, can occur when dabrafenib mesylate is administered as a single agent or when used in combination with trametinib.
Cutaneous Malignancies:
- Dabrafenib mesylate results in an increased incidence of cutaneous squamous cell carcinoma, keratoacanthoma, and melanoma. Dabrafenib mesylate when used in combination with trametinib results in an increased incidence of basal cell carcinoma.
- In Trial 1, cutaneous squamous cell carcinomas and keratoacanthomas (cuSCC) occurred in 7% (14/187) of patients treated with dabrafenib mesylate and in none of the patients treated with dacarbazine.
- Across clinical trials of dabrafenib mesylate (N = 586), the incidence of cuSCC was 11%. The median time to first cuSCC was 9 weeks (range: 1 to 53 weeks). Of those patients who developed new cuSCC, approximately 33% developed one or more cuSCC with continued administration of dabrafenib mesylate. The median time between diagnosis of the first cuSCC and the second cuSCC was 6 weeks.
- In Trial 1, the incidence of new primary malignant melanomas was 2% (3/187) for patients receiving dabrafenib mesylate while no dacarbazine-treated patient was diagnosed with new primary malignant melanoma.
- In Trial 2, the incidence of basal cell carcinoma was increased in patients receiving dabrafenib mesylate in combination with trametinib: 9% (5/55) of patients receiving dabrafenib mesylate in combination with trametinib compared with 2% (1/53) of patients receiving dabrafenib mesylate as a single agent. The range of time to diagnosis of basal cell carcinoma was 28 to 249 days in patients receiving dabrafenib mesylate in combination with trametinib and was 197 days for the patient receiving dabrafenib mesylate as a single agent.
- Cutaneous squamous cell carcinoma (SCC), including keratoacanthoma, occurred in 7% of patients receiving dabrafenib mesylate in combination with trametinib and 19% of patients receiving dabrafenib mesylate as a single agent. The range of time to diagnosis of cuSCC was 136 to197 days in the combination arm and was 9 to 197 days in the arm receiving dabrafenib mesylate as a single agent.
- New primary melanoma occurred in 2% (1/53) of patients receiving dabrafenib mesylate as a single agent and in none of the 55 patients receiving dabrafenib mesylate in combination with trametinib.
- Perform dermatologic evaluations prior to initiation of dabrafenib mesylate as a single agent or in combination with trametinib, every 2 months while on therapy, and for up to 6 months following discontinuation of dabrafenib mesylate. No dose modifications of dabrafenib mesylate or trametinib are required in patients who develop new primary cutaneous malignancies.
Non-cutaneous Malignancies:
- Based on its mechanism of action, dabrafenib mesylate may promote the growth and development of malignancies with activation of RAS through mutation or other mechanisms. In patients receiving dabrafenib mesylate in combination with trametinib four cases of non-cutaneous malignancies were identified: KRAS mutation-positive pancreatic adenocarcinoma (n = 1), recurrent NRAS mutation-positive colorectal carcinoma (n = 1), head and neck carcinoma (n = 1), and glioblastoma (n = 1). Monitor patients receiving the combination closely for signs or symptoms of non-cutaneous malignancies. Permanently discontinue dabrafenib mesylate for RAS mutation-positive non-cutaneous malignancies. If used in combination with trametinib, no dose modification of trametinib is required for patients who develop non-cutaneous malignancies.
Tumor Promotion in BRAF Wild-Type Melanoma
- In vitro experiments have demonstrated paradoxical activation of MAP-kinase signaling and increased cell proliferation in BRAF wild-type cells which are exposed to BRAF inhibitors. Confirm evidence of BRAF V600E or V600K mutation status prior to initiation of dabrafenib mesylate as a single agent or combination therapy.
Hemorrhage
- Hemorrhages, including major hemorrhages defined as symptomatic bleeding in a critical area or organ, can occur when dabrafenib mesylate is used in combination with trametinib.
- In Trial 2, treatment with dabrafenib mesylate in combination with trametinib resulted in an increased incidence and severity of any hemorrhagic event: 16% (9/55) of patients treated with dabrafenib mesylate in combination with trametinib compared with 2% (1/53) of patients treated with dabrafenib mesylate as a single agent. The major hemorrhagic events of intracranial or gastric hemorrhage occurred in 5% (3/55) of patients treated with dabrafenib mesylate in combination with trametinib compared with none of the 53 patients treated with dabrafenib mesylate as a single agent. Intracranial hemorrhage was fatal in 4% (2/55) of patients receiving dabrafenib mesylate in combination with trametinib.
- Permanently discontinue dabrafenib mesylate and trametinib for all Grade 4 hemorrhagic events and for any Grade 3 hemorrhagic events that do not improve. Withhold dabrafenib mesylate for Grade 3 hemorrhagic events; if improved resume at a lower dose level. Withhold trametinib for up to 3 weeks for Grade 3 hemorrhagic events; if improved, resume at a lower dose level.
Venous Thromboembolism
- Venous thromboembolism can occur when dabrafenib mesylate is used in combination with trametinib.
- In Trial 2, treatment with dabrafenib mesylate in combination with trametinib resulted in an increased incidence of deep venous thrombosis (DVT) and pulmonary embolism (PE): 7% (4/55) of patients treated with dabrafenib mesylate in combination with trametinib compared with none of the 53 patients treated with dabrafenib mesylate as a single agent. Pulmonary embolism was fatal in 2% (1/55) of patients receiving dabrafenib mesylate in combination with trametinib.
- Advise patients to immediately seek medical care if they develop symptoms of DVT or PE, such as shortness of breath, chest pain, or arm or leg swelling. Permanently discontinue dabrafenib mesylate and trametinib for life-threatening PE. Withhold trametinib and continue dabrafenib mesylate at the same dose for uncomplicated DVT or PE; if improved within 3 weeks, trametinib may be resumed at a lower dose level.
Cardiomyopathy
- Cardiomyopathy can occur when dabrafenib mesylate is used in combination with trametinib and with trametinib as a single agent.
- In Trial 2, cardiomyopathy occurred in 9% (5/55) of patients treated with dabrafenib mesylate in combination with trametinib and in none of patients treated with dabrafenib mesylate as a single agent. The median time to onset of cardiomyopathy in patients treated with dabrafenib mesylate in combination with trametinib was 86 days (range: 27 to 253 days). Cardiomyopathy was identified within the first month of treatment with dabrafenib mesylate in combination with trametinib in two of five patients. Development of cardiomyopathy resolved in all five patients following dose reduction (4/55) and/or dose interruption (1/55).
- Across clinical trials of dabrafenib mesylate administered in combination with trametinib (N = 202), 8% of patients developed evidence of cardiomyopathy (decrease in LVEF below institutional lower limits of normal with an absolute decrease in LVEF ≥10% below baseline). Two percent demonstrated a decrease in LVEF below institutional lower limits of normal with an absolute decrease in LVEF of ≥20% below baseline.
- Assess LVEF by echocardiogram or multigated acquisition (MUGA) scan before initiation of dabrafenib mesylate in combination with trametinib, one month after initiation, and then at 2- to 3-month intervals while on treatment with the combination. Withhold treatment with trametinib and continue dabrafenib mesylate at the same dose if absolute LVEF value decreases by 10% from pretreatment values and is less than the lower limit of normal. For symptomatic cardiomyopathy or persistent, asymptomatic LV dysfunction that does not resolve within 4 weeks, permanently discontinue trametinib and withhold dabrafenib mesylate. Resume dabrafenib mesylate at the same dose level upon recovery of cardiac function.
Ocular Toxicities
Retinal Pigment Epithelial Detachment (RPED):
- Retinal pigment epithelial detachments (RPED) can occur when dabrafenib mesylate is used in combination with trametinib and with trametinib as a single agent [refer to Full Prescribing Information for trametinib]. Retinal detachments resulting from trametinib are often bilateral and multifocal, occurring in the macular region of the retina.
- In Trial 2, ophthalmologic examinations including retinal evaluation were performed pretreatment and at regular intervals during treatment. RPED occurred in 2% (1/55) of patients receiving dabrafenib mesylate in combination with trametinib. Across clinical trials of dabrafenib mesylate administered in combination with trametinib (N = 202), the incidence of RPED was 1% (2/202).
- Perform ophthalmological evaluation at any time a patient reports visual disturbances and compare with baseline, if available. If dabrafenib mesylate is used in combination with trametinib, do not modify the dose of dabrafenib mesylate. Withhold trametinib if RPED is diagnosed. If resolution of the RPED is documented on repeat ophthalmological evaluation within 3 weeks, resume trametinib at a lower dose level. Discontinue trametinib if no improvement after 3 weeks.
Uveitis and Iritis:
- Uveitis and iritis can occur when dabrafenib mesylate is administered as a single agent or when used in combination with trametinib.
- Uveitis (including iritis) occurred in 1% (6/586) of patients treated with dabrafenib mesylate as a single agent and uveitis occurred in 1% (2/202) of patients treated with dabrafenib mesylate in combination with trametinib. Symptomatic treatment employed in clinical trials included steroid and mydriatic ophthalmic drops. Monitor patients for visual signs and symptoms of uveitis (e.g., change in vision, photophobia, eye pain). If diagnosed, withhold dabrafenib mesylate for up to 6 weeks until uveitis/iritis resolves to Grade 0-1. If dabrafenib mesylate is used in combination with trametinib, do not modify the dose of trametinib.
Serious Febrile Reactions
- Serious febrile reactions and fever of any severity complicated by hypotension, rigors or chills, dehydration, or renal failure, can occur when dabrafenib mesylate is administered as a single agent or when used in combination with trametinib. The incidence and severity of pyrexia are increased when dabrafenib mesylate is used in combination with trametinib compared with dabrafenib mesylate as a single agent.
- In Trial 1, the incidence of fever (serious and non-serious) was 28% in patients treated with dabrafenib mesylate and 10% in patients treated with dacarbazine. In patients treated with dabrafenib mesylate, the median time to initial onset of fever (any severity) was 11 days (range: 1 to 202 days) and the median duration of fever was 3 days (range: 1 to 129 days). Serious febrile reactions and fever of any severity complicated by hypotension, rigors or chills occurred in 3.7% (7/187) of patients treated with dabrafenib mesylate and in none of the 59 patients treated with dacarbazine.
- In Trial 2, the incidence of fever (serious and non-serious) was 71% (39/55) in patients treated with dabrafenib mesylate in combination with trametinib and 26% (14/53) in patients treated with dabrafenib mesylate as a single agent. Serious febrile reactions and fever of any severity complicated by hypotension, rigors or chills occurred in 25% (14/55) of patients treated with dabrafenib mesylate in combination with trametinib compared with 2% (1/53) of patients treated with dabrafenib mesylate as a single agent. Fever was complicated with chills/rigors in 51% (28/55), dehydration in 9% (5/55), renal failure in 4% (2/55), and syncope in 4% (2/55) of patients in Trial 2.
- In patients treated with dabrafenib mesylate in combination with trametinib, the median time to initial onset of fever was 30 days compared with 19 days in patients treated with dabrafenib mesylate as a single agent; the median duration of fever was 6 days with the combination compared with 4 days with dabrafenib mesylate as a single agent.
- Across clinical trials of dabrafenib mesylate administered in combination with trametinib (N = 202), the incidence of pyrexia was 57% (116/202).
- Withhold dabrafenib mesylate for fever of 101.3ºF or higher. Withhold trametinib for any fever higher than 104ºF. Withhold dabrafenib mesylate, and trametinib if used in combination, for any serious febrile reaction or fever complicated by hypotension, rigors or chills, dehydration, or renal failure and evaluate for signs and symptoms of infection. Refer to Table 2 for recommended dose modifications for adverse reactions. Prophylaxis with antipyretics may be required when resuming dabrafenib mesylate or trametinib.
Serious Skin Toxicity
- Serious skin toxicity can occur when dabrafenib mesylate is used in combination with trametinib and with trametinib as a single agent [refer to Full Prescribing Information for trametinib].
- In Trial 2, the incidence of any skin toxicity was similar for patients receiving dabrafenib mesylate in combination with trametinib (65% [36/55]) compared with patients receiving dabrafenib mesylate as a single agent (68% [36/53]). The median time to onset of skin toxicity in patients treated with dabrafenib mesylate in combination with trametinib was 37 days (range: 1 to 225 days) and median time to resolution of skin toxicity was 33 days (range: 3 to 421 days). No patient required dose reduction or permanent discontinuation of dabrafenib mesylate or trametinib for skin toxicity.
- Across clinical trials of dabrafenib mesylate in combination with trametinib (N = 202), severe skin toxicity and secondary infections of the skin requiring hospitalization occurred in 2.5% (5/202) of patients treated with dabrafenib mesylate in combination with trametinib.
- Withhold dabrafenib mesylate, and trametinib if used in combination, for intolerable or severe skin toxicity. dabrafenib mesylate and trametinib may be resumed at lower dose levels in patients with improvement or recovery from skin toxicity within 3 weeks.
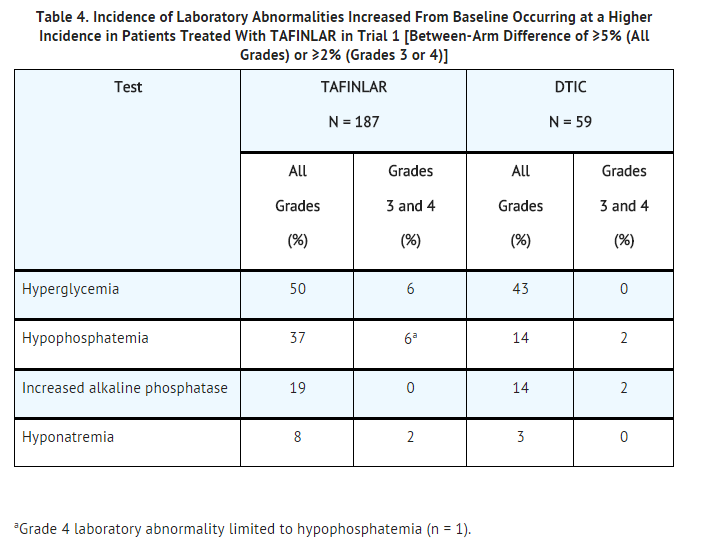
Hyperglycemia
- Hyperglycemia can occur when dabrafenib mesylate is administered as a single agent or when used in combination with trametinib.
- In Trial 1, 5 of 12 patients with a history of diabetes required more intensive hypoglycemic therapy while taking dabrafenib mesylate. The incidence of Grade 3 hyperglycemia based on laboratory values was 6% (12/187) in patients treated with dabrafenib mesylate compared with none of the dacarbazine-treated patients.
- In Trial 2, the incidence of Grade 3 hyperglycemia based on laboratory values was 5% (3/55) in patients treated with dabrafenib mesylate in combination with trametinib compared with 2% (1/53) in patients treated with dabrafenib mesylate as a single agent.
- Monitor serum glucose levels as clinically appropriate when dabrafenib mesylate is administered as a single agent or when used in combination with trametinib in patients with pre-existing diabetes or hyperglycemia. Advise patients to report symptoms of severe hyperglycemia such as excessive thirst or any increase in the volume or frequency of urination.
Glucose-6-Phosphate Dehydrogenase Deficiency
- Dabrafenib mesylate, which contains a sulfonamide moiety, confers a potential risk of hemolytic anemia in patients with glucose-6-phosphate dehydrogenase (G6PD) deficiency. Closely observe patients with G6PD deficiency for signs of hemolytic anemia.
Embryofetal Toxicity
- Based on its mechanism of action, dabrafenib mesylate can cause fetal harm when administered to a pregnant woman. Dabrafenib was teratogenic and embryotoxic in rats at doses three times greater than the human exposure at the recommended clinical dose. If this drug is used during pregnancy or if the patient becomes pregnant while taking this drug, the patient should be apprised of the potential hazard to a fetus.
- Advise female patients of reproductive potential to use a highly effective non-hormonal method of contraception since dabrafenib mesylate can render hormonal contraceptives ineffective, during treatment and for at least 2 weeks after treatment with dabrafenib mesylate or for 4 months after treatment with dabrafenib mesylate in combination with trametinib. Advise patients to contact their healthcare provider if they become pregnant, or if pregnancy is suspected, while taking dabrafenib mesylate.
Adverse Reactions
Clinical Trials Experience
- The following adverse reactions are discussed in greater detail in another section of the label:
- New Primary Malignancies
- Tumor Promotion in BRAF Wild-Type Melanoma
- Hemorrhage
- Venous Thromboembolism
- Cardiomyopathy
- Ocular Toxicities
- Serious Febrile Reactions
- Serious Skin Toxicity
- Hyperglycemia
- Glucose-6-Phosphate Dehydrogenase Deficiency
Clinical Trials Experience
- Because clinical trials are conducted under widely varying conditions, adverse reaction rates observed in the clinical trials of a drug cannot be directly compared to rates in the clinical trials of another drug and may not reflect the rates observed in practice.
- The data described in the Warnings and Precautions section and below reflect exposure to dabrafenib mesylate as a single agent and in combination with trametinib.
BRAF V600E Unresectable or Metastatic Melanoma:
- The safety of dabrafenib mesylate as a single agent was evaluated in 586 patients with BRAF V600 mutation-positive unresectable or metastatic melanoma, previously treated or untreated, who received dabrafenib mesylate 150 mg orally twice daily until disease progression or unacceptable toxicity, including 181 patients treated for at least 6 months and 86 additional patients treated for more than 12 months. Dabrafenib mesylate was studied in open-label, single-arm trials and in an open-label, randomized, active-controlled trial. The median daily dose of dabrafenib mesylate was 300 mg (range: 118 to 300 mg).
- Table 3 and Table 4 present adverse drug reactions and laboratory abnormalities identified from analyses of Trial 1. Trial 1, a multicenter, international, open-label, randomized (3:1), controlled trial allocated 250 patients with unresectable or metastatic BRAF V600E mutation-positive melanoma to receive dabrafenib mesylate 150 mg orally twice daily (n = 187) or dacarbazine 1,000 mg/m2 intravenously every 3 weeks (n = 63). The trial excluded patients with abnormal left ventricular ejection fraction or cardiac valve morphology (≥Grade 2), corrected QT interval ≥480 milliseconds on electrocardiogram, or a known history of glucose-6-phosphate dehydrogenase deficiency. The median duration on treatment was 4.9 months for patients treated with dabrafenib mesylate and 2.8 months for dacarbazine-treated patients. The population exposed to dabrafenib mesylate was 60% male, 99% white, and had a median age of 53 years.
- The most commonly occurring adverse reactions (≥20%) in patients treated with dabrafenib mesylate were, in order of decreasing frequency: hyperkeratosis, headache, pyrexia, arthralgia, papilloma, alopecia, and palmar-plantar erythrodysesthesia syndrome (PPES).
- The incidence of adverse events resulting in permanent discontinuation of study medication in Trial 1 was 3% for patients treated with dabrafenib mesylate and 3% for patients treated with dacarbazine. The most frequent (≥2%) adverse reactions leading to dose reduction of dabrafenib mesylate were pyrexia (9%), PPES (3%), chills (3%), fatigue (2%), and headache (2%).
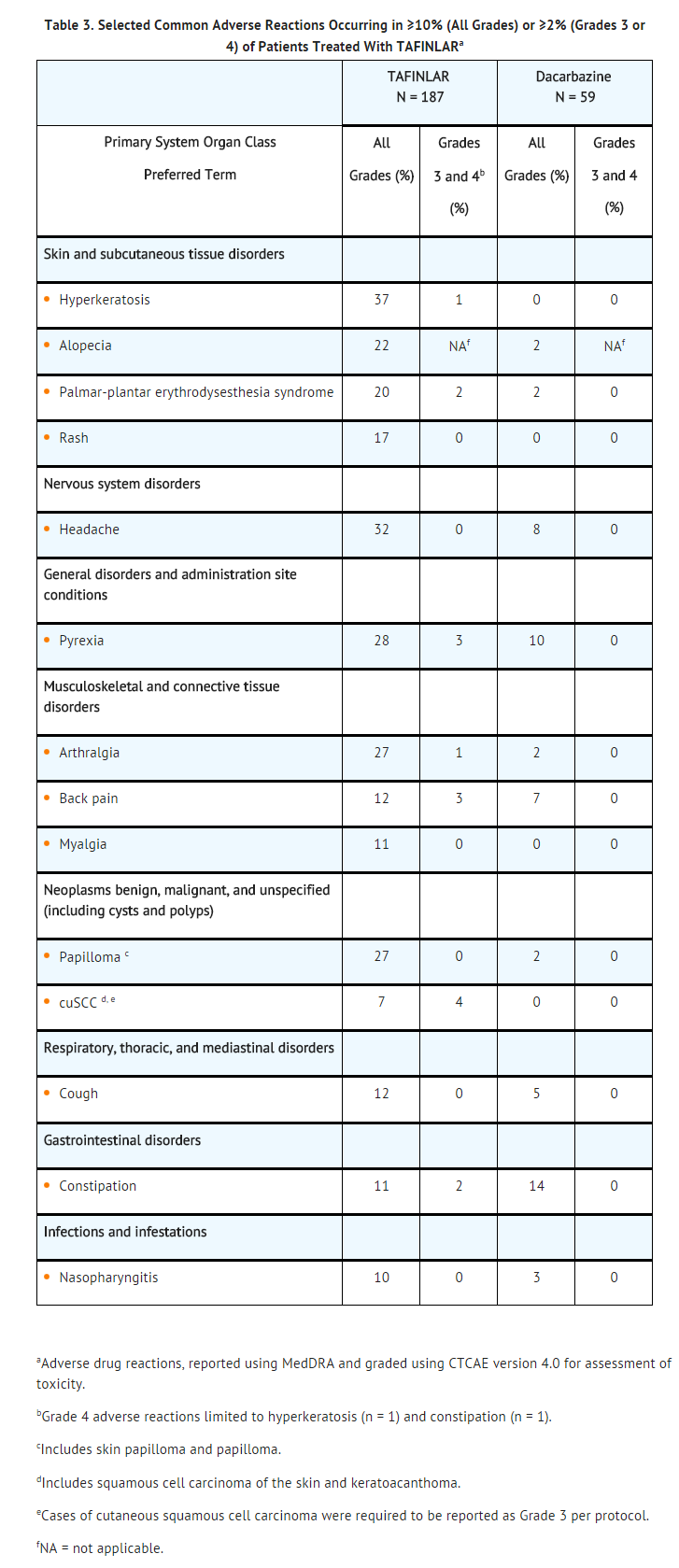
- Other clinically important adverse reactions observed in <10% of patients (N = 586) treated with dabrafenib mesylate were:
- Gastrointestinal Disorders: Pancreatitis.
- Immune System Disorders: Hypersensitivity manifesting as bullous rash.
- Renal and Urinary Disorders: Interstitial nephritis.
BRAF V600E or V600K Unresectable or Metastatic Melanoma:
- The safety of dabrafenib mesylate in combination with trametinib was evaluated in Trial 2 and other trials consisting of a total of 202 patients with BRAF V600 mutation-positive unresectable or metastatic melanoma who received dabrafenib mesylate 150 mg orally twice daily in combination with trametinib 2 mg orally once daily until disease progression or unacceptable toxicity. Among these 202 patients, 66 (33%) were exposed to dabrafenib mesylate and 68 (34%) were exposed to trametinib for greater than 6 to 12 months while 40 (20%) were exposed to dabrafenib mesylate and 36 (18%) were exposed to trametinib for greater than one year. The median age was 54 years, 57% were male, and >99% were white.
- Table 5 presents adverse reactions from Trial 2, a multicenter, open-label, randomized trial of 162 patients with BRAF V600E or V600K mutation-positive melanoma receiving dabrafenib mesylate 150 mg twice daily in combination with trametinib 2 mg orally once daily (n = 55), dabrafenib mesylate 150 mg orally twice daily in combination with trametinib 1 mg once daily (n = 54), and dabrafenib mesylate as a single agent 150 mg orally twice daily (n = 53). Patients with abnormal LVEF, history of acute coronary syndrome within 6 months, current evidence of Class II or greater congestive heart failure (New York Heart Association), history RVO or RPED, QTc interval ≥480 msec, treatment refractory hypertension, uncontrolled arrhythmias, history of pneumonitis or interstitial lung disease, or a known history of G6PD deficiency were excluded. The median duration of treatment was 10.9 months for both dabrafenib mesylate and trametinib (2-mg orally once-daily treatment group) when used in combination, 10.6 months for both dabrafenib mesylate and trametinib (1-mg orally once-daily treatment group) when used in combination, and 6.1 months for dabrafenib mesylate as a single agent.
- In Trial 2, 13% of patients receiving dabrafenib mesylate in combination with trametinib experienced adverse reactions resulting in permanent discontinuation of trial medication(s). The most common adverse reaction resulting in permanent discontinuation was pyrexia (4%). Adverse reactions led to dose reductions in 49% and dose interruptions in 67% of patients treated with dabrafenib mesylate in combination with trametinib. Pyrexia, chills, and nausea were the most common reasons cited for dose reductions and pyrexia, chills, and decreased ejection fraction were the most common reasons cited for dose interruptions of dabrafenib mesylate and trametinib when used in combination.

- Other clinically important adverse reactions (N = 202) observed in <10% of patients treated with dabrafenib mesylate in combination with trametinib were:
- Eye Disorders: Vision blurred, transient blindness.
- Gastrointestinal Disorders: Stomatitis, pancreatitis.
- General Disorders and Administration Site Conditions: Asthenia.
- Infections and Infestations: Cellulitis, folliculitis, paronychia, rash pustular.
- Neoplasms Benign, Malignant, and Unspecified (including cysts and polyps): Skin papilloma.
- Skin and Subcutaneous Tissue Disorders: Palmar-plantar erythrodysesthesia syndrome, hyperkeratosis, hyperhidrosis.
- Vascular Disorders: Hypertension.
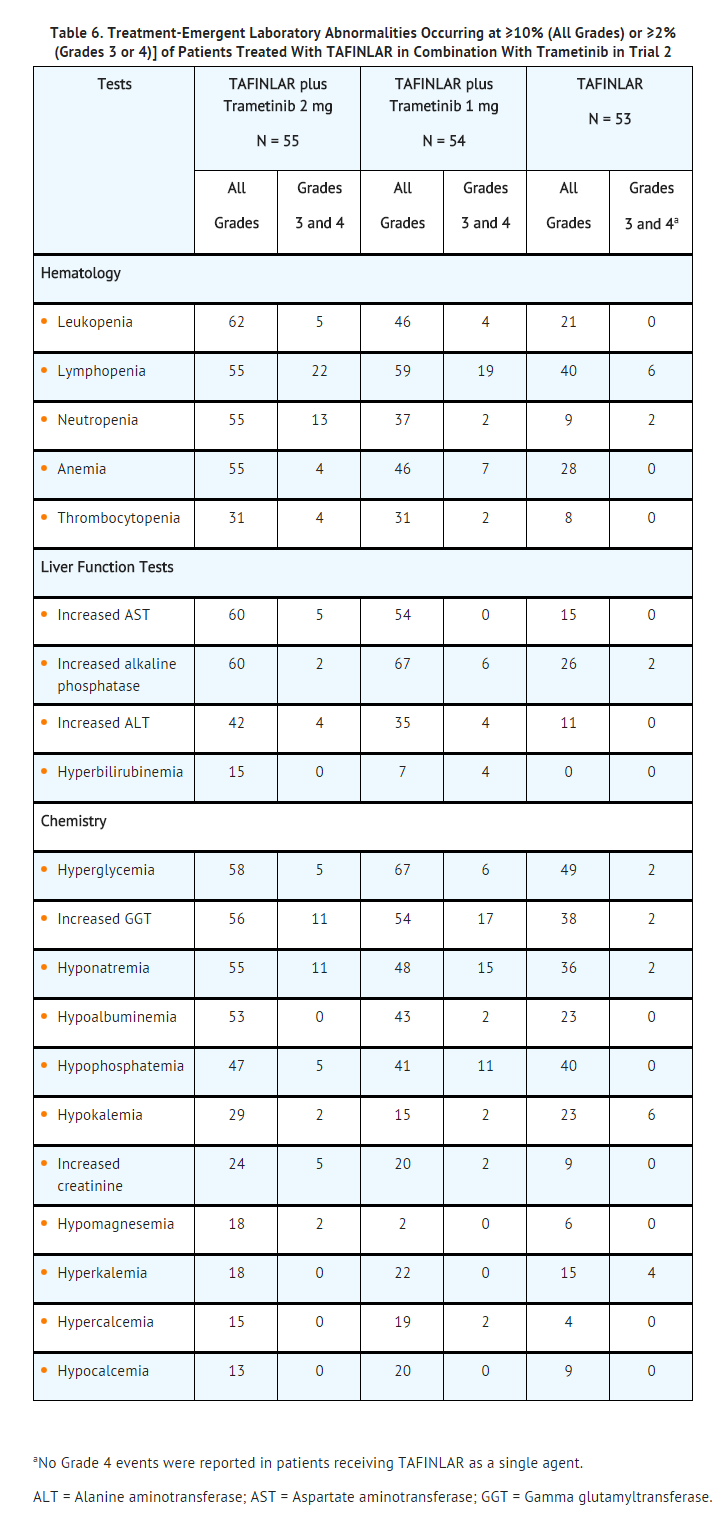
QT Prolongation: In Trial 2, QTcF prolongation to >500 msec occurred in 4% (2/55) of patients treated with dabrafenib mesylate in combination with trametinib and in 2% (1/53) of patients treated with dabrafenib mesylate as a single agent. The QTcF was increased more than 60 msec from baseline in 13% (7/55) of patients treated withdabrafenib mesylate in combination with trametinib and 2% (1/53) of patients treated with dabrafenib mesylate as a single agent.
Postmarketing Experience
There is limited information regarding Postmarketing Experience of Dabrafenib mesylate in the drug label.
Drug Interactions
Effects of Other Drugs on Dabrafenib
Dabrafenib is primarily metabolized by CYP2C8 and CYP3A4. Strong inhibitors of CYP3A4 or CYP2C8 may increase concentrations of dabrafenib and strong inducers of CYP3A4 or CYP2C8 may decrease concentrations of dabrafenib. Substitution of strong inhibitors or strong inducers of CYP3A4 or CYP2C8 is recommended during treatment with dabrafenib mesylate. If concomitant use of strong inhibitors (e.g., ketoconazole, nefazodone, clarithromycin, gemfibrozil) or strong inducers (e.g., rifampin, phenytoin, carbamazepine, phenobarbital, St John’s wort) of CYP3A4 or CYP2C8 is unavoidable, monitor patients closely for adverse reactions when taking strong inhibitors or loss of efficacy when taking strong inducers.
Effects of Dabrafenib on Other Drugs
Dabrafenib induces CYP3A4 and CYP2C9. Dabrafenib decreased the systemic exposures of midazolam (a CYP3A4 substrate), S-warfarin (a CYP2C9 substrate), and R-warfarin (a CYP3A4/CYP1A2 substrate). Monitor international normalized ratio (INR) levels more frequently in patients receiving warfarin during initiation or discontinuation of dabrafenib. Coadministration of dabrafenib mesylate with other substrates of these enzymes, including dexamethasone or hormonal contraceptives, can result in decreased concentrations and loss of efficacy. Substitute for these medications or monitor patients for loss of efficacy if use of these medications is unavoidable.
Trametinib
- Coadministration of dabrafenib mesylate 150 mg twice daily and trametinib 2 mg once daily resulted in no clinically relevant pharmacokinetic drug interactions.
Use in Specific Populations
Pregnancy
Pregnancy Category (FDA): Pregnancy Category D
Risk Summary: Based on its mechanism of action, dabrafenib mesylate can cause fetal harm when administered to a pregnant woman. Dabrafenib was teratogenic and embryotoxic in rats at doses three times greater than the human exposure at the recommended clinical dose of 150 mg twice daily based on AUC. If this drug is used during pregnancy or if the patient becomes pregnant while taking this drug, the patient should be apprised of the potential hazard to a fetus.
Animal Data: In a combined female fertility and embryo fetal development study in rats, developmental toxicity consisted of embryo-lethality, ventricular septal defects, and variation in thymic shape at a dabrafenib dose of 300 mg/kg/day (approximately three times the human exposure at the recommended dose based on AUC). At doses of 20 mg/kg/day or greater (equivalent to the human exposure at the recommended dose based on AUC), rats demonstrated delays in skeletal development and reduced fetal body weight.
Pregnancy Category (AUS):
- Australian Drug Evaluation Committee (ADEC) Pregnancy Category
There is no Australian Drug Evaluation Committee (ADEC) guidance on usage of Dabrafenib mesylate in women who are pregnant.
Labor and Delivery
There is no FDA guidance on use of Dabrafenib mesylate during labor and delivery.
Nursing Mothers
- It is not known whether this drug is present in human milk. Because many drugs are present in human milk and because of the potential for serious adverse reactions from dabrafenib mesylate in nursing infants, a decision should be made whether to discontinue nursing or discontinue the drug, taking into account the importance of the drug to the mother.
Pediatric Use
- The safety and effectiveness of dabrafenib mesylate have not been established in pediatric patients.
- In a repeat-dose toxicity study in juvenile rats, an increased incidence of kidney cysts and tubular deposits were noted at doses as low as 0.2 times the human exposure at the recommended adult dose based on AUC. Additionally, forestomach hyperplasia, decreased bone length and early vaginal opening were noted at doses as low as 0.8 times the human exposure at the recommended adult dose based on AUC.
Geriatic Use
- One hundred and twenty-six (22%) of 586 patients in clinical trials of dabrafenib mesylate administered as a single agent and 40 (21%) of the 187 patients receiving dabrafenib mesylate in Trial 1 were ≥65 years of age. No overall differences in the effectiveness or safety of dabrafenib mesylate were observed in the elderly in Trial 1.
- Across all clinical trials of dabrafenib mesylate administered in combination with trametinib, there was an insufficient number of patients aged 65 years and over to determine whether they respond differently from younger patients. In Trial 2, 11 patients (20%) were 65 years of age and older, and 2 patients (4%) were 75 years of age and older.
Gender
Contraception:Females: Advise female patients of reproductive potential to use highly effective contraception during treatment and for at least 2 weeks after the last dose of dabrafenib mesylate or at least 4 months after the last dose of dabrafenib mesylate taken in combination with trametinib. Counsel patients to use a non-hormonal method of contraception since dabrafenib mesylate can render hormonal contraceptives ineffective. Advise patients to contact their healthcare provider if they become pregnant, or if pregnancy is suspected, while taking dabrafenib mesylate.
Infertility:
- Females: Increased follicular cysts and decreased corpora lutea were observed in female rats treated with trametinib. Advise female patients of reproductive potential that dabrafenib mesylate taken in combination with trametinib may impair fertility in female patients.
- Males: Effects on spermatogenesis have been observed in animals. Advise male patients of the potential risk for impaired spermatogenesis, and to seek counseling on fertility and family planning options prior to starting treatment with dabrafenib mesylate.
Race
There is no FDA guidance on the use of Dabrafenib mesylate with respect to specific racial populations.
Renal Impairment
- No formal pharmacokinetic trial in patients with renal impairment has been conducted. Dose adjustment is not recommended for patients with mild or moderate renal impairment based on the results of the population pharmacokinetic analysis. An appropriate dose has not been established for patients with severe renal impairment.
Hepatic Impairment
- No formal pharmacokinetic trial in patients with hepatic impairment has been conducted. Dose adjustment is not recommended for patients with mild hepatic impairment based on the results of the population pharmacokinetic analysis. As hepatic metabolism and biliary secretion are the primary routes of elimination of dabrafenib and its metabolites, patients with moderate to severe hepatic impairment may have increased exposure. An appropriate dose has not been established for patients with moderate to severe hepatic impairment.
Females of Reproductive Potential and Males
There is no FDA guidance on the use of Dabrafenib mesylate in women of reproductive potentials and males.
Immunocompromised Patients
There is no FDA guidance one the use of Dabrafenib mesylate in patients who are immunocompromised.
Administration and Monitoring
Administration
- Oral
Monitoring
There is limited information regarding Monitoring of Dabrafenib mesylate in the drug label.
IV Compatibility
There is limited information regarding IV Compatibility of Dabrafenib mesylate in the drug label.
Overdosage
- There is no information on overdosage of dabrafenib mesylate. Since dabrafenib is highly bound to plasma proteins, hemodialysis is likely to be ineffective in the treatment of overdose with dabrafenib mesylate.
Pharmacology
There is limited information regarding Dabrafenib mesylate Pharmacology in the drug label.
Mechanism of Action
- Dabrafenib is an inhibitor of some mutated forms of BRAF kinases with in vitro IC50 values of 0.65, 0.5, and 1.84 nM for BRAF V600E, BRAF V600K, and BRAF V600D enzymes, respectively. Dabrafenib also inhibits wild-type BRAF and CRAF kinases with IC50 values of 3.2 and 5.0 nM, respectively, and other kinases such as SIK1, NEK11, and LIMK1 at higher concentrations. Some mutations in the BRAF gene, including those that result in BRAF V600E, can result in constitutively activated BRAF kinases that may stimulate tumor cell growth [see Indications and Usage (1)]. Dabrafenib inhibits BRAF V600 mutation-positive melanoma cell growth in vitro and in vivo.
- Dabrafenib and trametinib target two different tyrosine kinases in the RAS/RAF/MEK/ERK pathway. Use of dabrafenib and trametinib in combination resulted in greater growth inhibition of BRAF V600 mutation-positive melanoma cell lines in vitro and prolonged inhibition of tumor growth in BRAF V600 mutation positive melanoma xenografts compared with either drug alone.
Structure
- Dabrafenib mesylate is a kinase inhibitor. The chemical name for dabrafenib mesylate is N-{3-[5-(2-Amino-4-pyrimidinyl)-2-(1,1-dimethylethyl)-1,3-thiazol-4-yl]-2-fluorophenyl}-2,6-difluorobenzene sulfonamide, methanesulfonate salt. It has the molecular formula C23H20F3N5O2S2•CH4O3S and a molecular weight of 615.68. Dabrafenib mesylate has the following chemical structure.
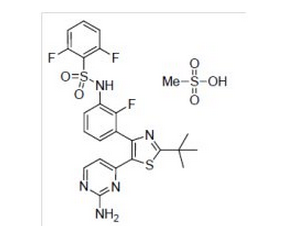
- Dabrafenib mesylate is a white to slightly colored solid with three pKas: 6.6, 2.2, and -1.5. It is very slightly soluble at pH 1 and practically insoluble above pH 4 in aqueous media.
- TAFINLAR (dabrafenib) capsules are supplied as 50-mg and 75-mg capsules for oral administration. Each 50-mg capsule contains 59.25 mg dabrafenib mesylate equivalent to 50 mg of dabrafenib free base. Each 75-mg capsule contains 88.88 mg dabrafenib mesylate equivalent to 75 mg of dabrafenib free base.
- The inactive ingredients of dabrafenib mesylate are colloidal silicon dioxide, magnesium stearate, and microcrystalline cellulose. Capsule shells contain hypromellose, red iron oxide (E172), and titanium dioxide (E171).
Pharmacodynamics
There is limited information regarding Pharmacodynamics of Dabrafenib mesylate in the drug label.
Pharmacokinetics
Absorption: After oral administration, median time to achieve peak plasma concentration (Tmax) is 2 hours. Mean absolute bioavailability of oral dabrafenib is 95%. Following a single dose, dabrafenib exposure (Cmax and AUC) increased in a dose-proportional manner across the dose range of 12 to 300 mg, but the increase was less than dose-proportional after repeat twice-daily dosing. After repeat twice-daily dosing of 150 mg, the mean accumulation ratio was 0.73 and the inter-subject variability (CV%) of AUC at steady-state was 38%.
Administration of dabrafenib with a high-fat meal decreased Cmax by 51%, decreased AUC by 31%, and delayed median Tmax by 3.6 hours as compared with the fasted state.
Distribution: Dabrafenib is 99.7% bound to human plasma proteins. The apparent volume of distribution (Vc/F) is 70.3 L.
Metabolism: The metabolism of dabrafenib is primarily mediated by CYP2C8 and CYP3A4 to form hydroxy-dabrafenib. Hydroxy-dabrafenib is further oxidized via CYP3A4 to form carboxy-dabrafenib and subsequently excreted in bile and urine. Carboxy-dabrafenib is decarboxylated to form desmethyl-dabrafenib; desmethyl-dabrafenib may be reabsorbed from the gut. Desmethyl-dabrafenib is further metabolized by CYP3A4 to oxidative metabolites. Hydroxy-dabrafenib terminal half-life (10 hours) parallels that of dabrafenib while the carboxy- and desmethyl-dabrafenib metabolites exhibited longer half-lives (21 to 22 hours). Mean metabolite-to-parent AUC ratios following repeat-dose administration are 0.9, 11, and 0.7 for hydroxy-, carboxy-, and desmethyl-dabrafenib, respectively. Based on systemic exposure, relative potency, and pharmacokinetic properties, both hydroxy- and desmethyl-dabrafenib are likely to contribute to the clinical activity of dabrafenib.
Elimination: The mean terminal half-life of dabrafenib is 8 hours after oral administration. The apparent clearance of dabrafenib is 17.0 L/h after single dosing and 34.4 L/h after 2 weeks of twice-daily dosing.
Fecal excretion is the major route of elimination accounting for 71% of radioactive dose while urinary excretion accounted for 23% of total radioactivity as metabolites only.
Specific Populations:
Age, Body Weight, and Gender: Based on the population pharmacokinetics analysis, age has no effect on dabrafenib pharmacokinetics. Pharmacokinetic differences based on gender and on weight are not clinically relevant.
Pediatric: Pharmacokinetics of dabrafenib has not been studied in pediatric patients.
Renal: No formal pharmacokinetic trial in patients with renal impairment has been conducted. The pharmacokinetics of dabrafenib were evaluated using a population analysis in 233 patients with mild renal impairment (GFR 60 to 89 mL/min/1.73 m2) and 30 patients with moderate renal impairment (GFR 30 to 59 mL/min/1.73 m2) enrolled in clinical trials. Mild or moderate renal impairment has no effect on systemic exposure to dabrafenib and its metabolites. No data are available in patients with severe renal impairment.
Hepatic: No formal pharmacokinetic trial in patients with hepatic impairment has been conducted. The pharmacokinetics of dabrafenib was evaluated using a population analysis in 65 patients with mild hepatic impairment enrolled in clinical trials. Mild hepatic impairment has no effect on systemic exposure to dabrafenib and its metabolites. No data are available in patients with moderate to severe hepatic impairment.
Drug Interactions:
- In vitro studies show that dabrafenib is a substrate of CYP3A4 and CYP2C8 while hydroxy-dabrafenib and desmethyl-dabrafenib are CYP3A4 substrates. Coadministration of dabrafenib 75 mg twice daily and ketoconazole 400 mg once daily (a strong CYP3A4 inhibitor) for 4 days increased dabrafenib AUC by 71%, hydroxy-dabrafenib AUC by 82%, and desmethyl-dabrafenib AUC by 68%. Coadministration of dabrafenib 75 mg twice daily and gemfibrozil 600 mg twice daily (a strong CYP2C8 inhibitor) for 4 days increased dabrafenib AUC by 47%, with no change in the AUC of dabrafenib metabolites. Dabrafenib is a substrate of human P-glycoprotein (P-gp) and breast cancer resistance protein (BCRP) in vitro.
- In vitro data demonstrate that dabrafenib is an inducer of CYP3A4 and CYP2B6 via activation of the pregnane X receptor (PXR) and constitutive androstane receptor (CAR) nuclear receptors. Dabrafenib may also induce CYP2C enzymes via the same mechanism. Coadministration of dabrafenib 150 mg twice daily for 15 days and a single dose of midazolam 3 mg (a CYP3A4 substrate) decreased midazolam AUC by 74%. Coadministration of dabrafenib 150 mg twice daily for 15 days and a single dose of warfarin 15 mg decreased the AUC of S-warfarin (a CYP2C9 substrate) by 37% and the AUC of R-warfarin (a CYP3A4/CYP1A2 substrate) by 33% [see Drug Interactions (7.2)].
- Dabrafenib and its metabolites, hydroxy-dabrafenib, carboxy-dabrafenib, and desmethyl-dabrafenib, are inhibitors of human organic anion transporting polypeptide OATP1B1, OATP1B3 and organic anion transporter OAT1 and OAT3 in vitro. Dabrafenib and desmethyl-dabrafenib are inhibitors of BCRP in vitro.
- Coadministration of trametinib 2 mg daily with dabrafenib 150 mg twice daily resulted in a 23% increase in AUC of dabrafenib, a 33% increase in AUC of desmethyl-dabrafenib, and no change in AUC of trametinib or hydroxy-dabrafenib as compared with administration of either drug alone.
- Drugs that alter the pH of the upper GI tract (e.g., proton pump inhibitors, H2-receptor antagonists, antacids) may alter the solubility of dabrafenib and reduce its bioavailability. However, no formal clinical trial has been conducted to evaluate the effect of gastric pH-altering agents on the systemic exposure of dabrafenib. When dabrafenib mesylate is coadministered with a proton pump inhibitor, H2-receptor antagonist, or antacid, systemic exposure of dabrafenib may be decreased and the effect on efficacy of dabrafenib mesylate is unknown.
Nonclinical Toxicology
Carcinogenesis, Mutagenesis, Impairment of Fertility
- Carcinogenicity studies with dabrafenib have not been conducted. Dabrafenib mesylate increased the risk of cutaneous squamous cell carcinomas in patients in clinical trials.
- Dabrafenib was not mutagenic in vitro in the bacterial reverse mutation assay (Ames test) or the mouse lymphoma assay, and was not clastogenic in an in vivo rat bone marrow micronucleus test.
- In a combined female fertility and embryofetal development study in rats, a reduction in fertility was noted at doses greater than or equal to 20 mg/kg/day (equivalent to the human exposure at the recommended dose based on AUC). A reduction in the number of ovarian corpora lutea was noted in pregnant females at 300 mg/kg/day (which is approximately three times the human exposure at the recommended dose based on AUC).
- Male fertility studies with dabrafenib have not been conducted; however, in repeat-dose studies, testicular degeneration/depletion was seen in rats and dogs at doses equivalent to and three times the human exposure at the recommended dose based on AUC, respectively.
Animal Toxicology and/or Pharmacology
- Adverse cardiovascular effects were noted in dogs at dabrafenib doses of 50 mg/kg/day (approximately five times the human exposure at the recommended dose based on AUC) or greater, when administered for up to 4 weeks. Adverse effects consisted of coronary arterial degeneration/necrosis and hemorrhage, as well as cardiac atrioventricular valve hypertrophy/hemorrhage.
Clinical Studies
BRAF V600E Mutation-Positive Unresectable or Metastatic Melanoma
- In Trial 1, the safety and efficacy of dabrafenib mesylate as a single agent were demonstrated in an international, multicenter, randomized (3:1), open-label, active-controlled trial conducted in 250 patients with previously untreated BRAF V600E mutation-positive, unresectable or metastatic melanoma. Patients with any prior use of BRAF inhibitors or MEK inhibitors were excluded. Patients were randomized to receive dabrafenib mesylate 150 mg orally twice daily (n = 187) or dacarbazine 1,000 mg/m2 intravenously every 3 weeks (n = 63). Randomization was stratified by disease stage at baseline [unresectable stage III (regional nodal or in-transit metastases), M1a (distant skin, subcutaneous, or nodal metastases), or M1b (lung metastases) versus M1c melanoma (all other visceral metastases or elevated serum LDH)]. The main efficacy outcome measure was progression-free survival (PFS) as assessed by the investigator. In addition, an independent radiology review committee (IRRC) assessed the following efficacy outcome measures in pre-specified supportive analyses: PFS, confirmed objective response rate (ORR), and duration of response.
- The median age of patients in Trial 1 was 52 years. The majority of the trial population was male (60%), white (99%), had an ECOG performance status of 0 (67%), M1c disease (66%), and normal LDH (62%). All patients had tumor tissue with mutations in BRAF V600E as determined by a clinical trial assay at a centralized testing site. Tumor samples from 243 patients (97%) were tested retrospectively, using an FDA-approved companion diagnostic test, THxID™-BRAF assay.
- The median durations of follow-up prior to initiation of alternative treatment in patients randomized to receive dabrafenib mesylate was 5.1 months and in the dacarbazine arm was 3.5 months. Twenty-eight (44%) patients crossed over from the dacarbazine arm at the time of disease progression to receive dabrafenib mesylate.
- Trial 1 demonstrated a statistically significant increase in progression-free survival in the patients treated with TAFINLAR. Table 7 and Figure 1 summarize the PFS results.
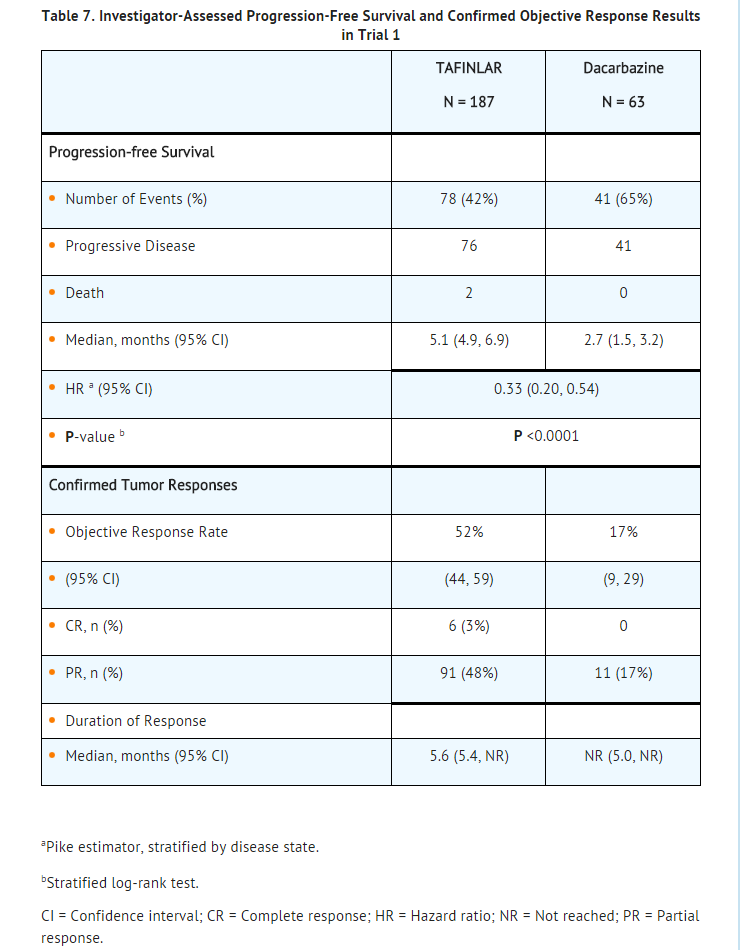
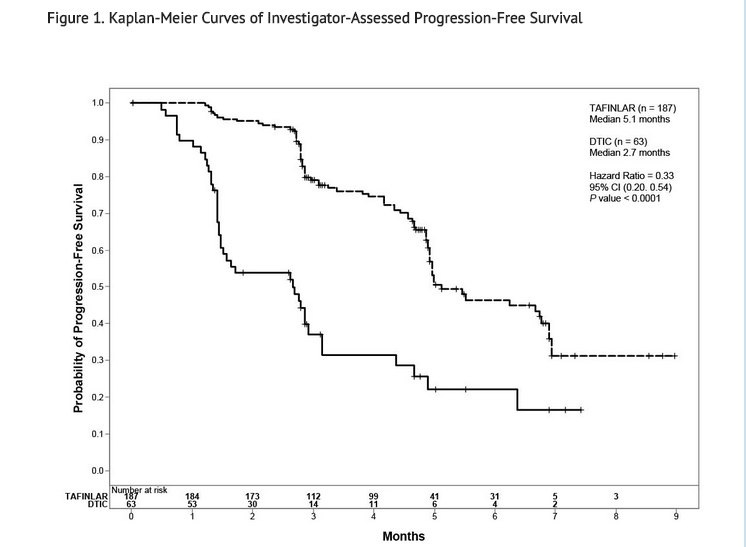
- In supportive analyses based on IRRC assessment and in an exploratory subgroup analysis of patients with retrospectively confirmed V600E mutation-positive melanoma with the THxID™-BRAF assay, the PFS results were consistent with those of the primary efficacy analysis.
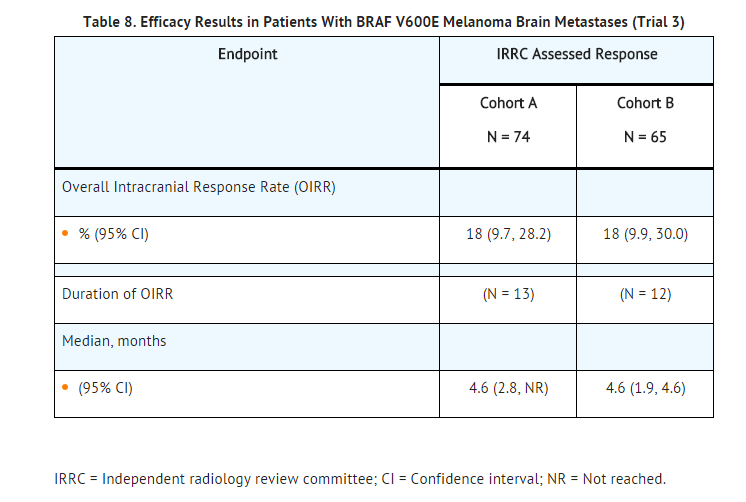
- The activity of dabrafenib mesylate for the treatment of BRAF V600E mutation-positive melanoma, metastatic to the brain was evaluated in a single-arm, open-label, two-cohort multi-center trial (Trial 3). All patients received dabrafenib mesylate 150 mg twice daily. Patients in Cohort A (n = 74) had received no prior local therapy for brain metastases, while patients in Cohort B (n = 65) had received at least one local therapy for brain metastases, including, but not limited to, surgical resection, whole brain radiotherapy, or stereotactic radiosurgery such as gamma knife, linear-accelerated-based radiosurgery, charged particles, or CyberKnife. In addition, patients in Cohort B were required to have evidence of disease progression in a previously treated lesion or an untreated lesion. Additional eligibility criteria were at least one measurable lesion of 0.5 cm or greater in largest diameter on contrast-enhanced MRI, stable or decreasing corticosteroid dose, and no more than two prior systemic regimens for treatment of metastatic disease. The primary outcome measure was estimation of the overall intracranial response rate (OIRR) in each cohort.
- The median age of patients in Cohort A was 50 years, 72% were male, 100% were white, 59% had a pre-treatment ECOG performance status of 0, and 57% had an elevated LDH value at baseline. The median age of patients in Cohort B was 51 years, 63% were male, 98% were white, 66% had a pre-treatment ECOG performance status of 0, and 54% had an elevated LDH value at baseline. Efficacy results as determined by an independent radiology review committee, masked to investigator response assessments, are provided in Table 8.
BRAF V600E or V600K Unresectable or Metastatic Melanoma
- Trial 2 was a multicenter, open-label, randomized (1:1:1) dose-ranging trial designed to evaluate the clinical activity and safety of dabrafenib mesylate in combination with trametinib (at two different doses) and to compare the safety with dabrafenib mesylate as a single agent in 162 patients with BRAF V600E or V600K mutation-positive, unresectable or metastatic melanoma. Patients were permitted to have had one prior chemotherapy regimen and prior aldesleukin; patients with prior exposure to BRAF or MEK inhibitors were ineligible. Patients were randomized to receive dabrafenib mesylate 150 mg orally twice daily with trametinib 2 mg orally once daily (n = 54), dabrafenib mesylate 150 mg orally twice daily with trametinib 1 mg orally once daily (n = 54), or dabrafenib mesylate 150 mg orally twice daily (n = 54). Treatment continued until disease progression or unacceptable toxicity. Patients randomized to dabrafenib mesylate as a single agent were offered dabrafenib mesylate 150 mg orally twice daily with trametinib 2 mg orally once daily at the time of investigator-assessed disease progression. The major efficacy outcome measure was investigator-assessed overall response rate (ORR). Additional efficacy outcome measures were investigator-assessed duration of response, independent radiology review committee (IRRC)-assessed ORR, and IRRC-assessed duration of response.
- The median age of patients was 53 years, 57% were male, >99% were white, 66% of patients had a pre-treatment ECOG performance status of 0, 67% had M1c disease, 54% had a normal LDH at baseline, and 8% had history of brain metastases. Most patients (81%) had not received prior anti-cancer therapy for unresectable or metastatic disease. Based on local laboratory or centralized testing, 85% of patients’ tumors had BRAF V600E mutations and 15% had BRAF V600K mutations.
- The median duration of follow-up was 14 months. Efficacy outcomes for the trial arms receiving dabrafenib mesylate in combination with trametinib 2 mg orally once daily and TAFINLAR as a single agent are summarized in Table 9.

The ORR results were similar in subgroups defined by BRAF mutation subtype, i.e., in the 85% of patients with V600E mutation-positive melanoma and in the 15% of patients with V600K mutation-positive melanoma. In exploratory subgroup analyses of the patients with retrospectively confirmed BRAF V600E or V600K mutation-positive melanoma using the THxID™-BRAF assay, the ORR results were also similar to the intent-to-treat analysis.
How Supplied
- 50 mg Capsules: Dark red capsule imprinted with ‘GS TEW’ and ‘50 mg’ available in bottles of 120 (NDC 0173-0846-08). Each bottle contains a silica gel desiccant.
- 75 mg Capsules: Dark pink capsule imprinted with ‘GS LHF’ and ‘75 mg’ available in bottles of 120 (NDC 0173-0847-08). Each bottle contains a silica gel desiccant.
Storage
- Store at 25°C (77°F); excursions permitted to 15° to 30°C (59° to 86°F) [see USP Controlled Room Temperature].
Images
Drug Images
{{#ask: Page Name::Dabrafenib mesylate |?Pill Name |?Drug Name |?Pill Ingred |?Pill Imprint |?Pill Dosage |?Pill Color |?Pill Shape |?Pill Size (mm) |?Pill Scoring |?NDC |?Drug Author |format=template |template=DrugPageImages |mainlabel=- |sort=Pill Name }}
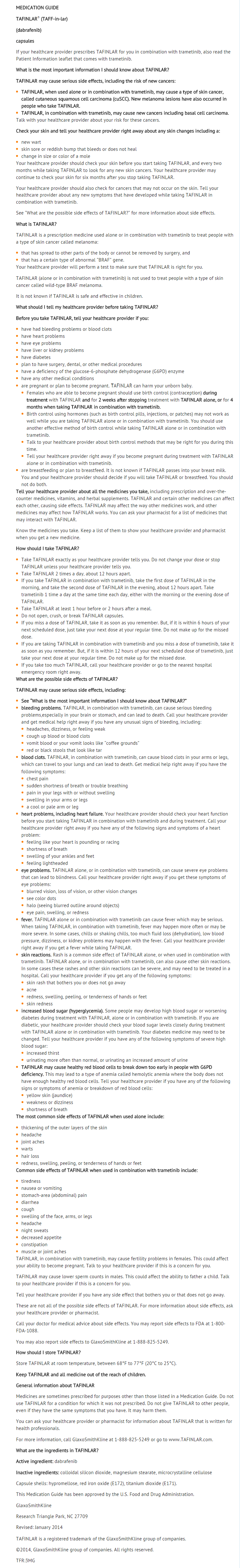
Package and Label Display Panel
{{#ask: Label Page::Dabrafenib mesylate |?Label Name |format=template |template=DrugLabelImages |mainlabel=- |sort=Label Page }}
Patient Counseling Information
Inform patients of the following:
- Evidence of BRAF V600E mutation in the tumor specimen is necessary to identify patients for whom treatment with dabrafenib mesylate as a single agent is indicated and evidence of BRAF V600E or V600K mutation in tumor specimens is necessary to identify patients for whom treatment with dabrafenib mesylate in combination with trametinib is indicated.
- Dabrafenib mesylate increases the risk of developing new primary cutaneous and non-cutaneous malignancies. Advise patients to contact their doctor immediately for any new lesions, changes to existing lesions on their skin, or signs and symptoms of other malignancies.
- Dabrafenib mesylate administered in combination with trametinib increases the risk of intracranial and gastrointestinal hemorrhage. Advise patients to contact their healthcare provider to seek immediate medical attention for signs or symptoms of unusual bleeding or hemorrhage.
- Dabrafenib mesylate administered in combination with trametinib increases the risks of pulmonary embolism and deep venous thrombosis. Advise patients to seek immediate medical attention for sudden onset of difficulty breathing, leg pain, or swelling.
- Dabrafenib mesylate administered in combination with trametinib can cause cardiomyopathy. Advise patients to immediately report any signs or symptoms of heart failure to their healthcare provider.
- Dabrafenib mesylate can cause visual disturbances; dabrafenib mesylate administered in combination with trametinib can lead to blindness. Advise patients to contact their healthcare provider if they experience any changes in their vision.
- Dabrafenib mesylate administered as a single agent and in combination with trametinib, can cause pyrexia including serious febrile reactions. Inform patients that the incidence and severity of pyrexia are increased when dabrafenib mesylate is given in combination with trametinib. Instruct patients to contact their doctor if they develop fever while taking dabrafenib mesylate.
- Dabrafenib mesylate in combination with trametinib can cause serious skin toxicities which may require hospitalization. Advise patients to contact their healthcare provider for progressive or intolerable rash.
- Dabrafenib mesylate can impair glucose control in diabetic patients resulting in the need for more intensive hypoglycemic treatment. Advise patients to contact their doctor to report symptoms of severe hyperglycemia.
- Dabrafenib mesylate may cause hemolytic anemia in patients with glucose-6-phosphate dehydrogenase (G6PD) deficiency. Advise patients with known G6PD deficiency to contact their doctor to report signs or symptoms of anemia or hemolysis.
- Dabrafenib mesylate can cause fetal harm if taken during pregnancy. Instruct female patients to use non-hormonal, highly effective contraception during treatment and for 2 weeks after discontinuation of treatment with dabrafenib mesylate as a single agent, or for 4 months after discontinuation of treatment with dabrafenib mesylate in combination with trametinib. Advise patients to contact their doctor if they become pregnant, or if pregnancy is suspected, while taking dabrafenib mesylate.
- Nursing infants may experience serious adverse reactions if the mother is taking dabrafenib mesylate during breastfeeding. Advise breastfeeding mothers to discontinue nursing while taking dabrafenib mesylate.
- Male patients are at an increased risk for impaired spermatogenesis.
Dabrafenib mesylate should be taken either at least 1 hour before or at least 2 hours after a meal.
Medication Guide
Precautions with Alcohol
- Alcohol-Dabrafenib mesylate interaction has not been established. Talk to your doctor about the effects of taking alcohol with this medication.
Brand Names
- TAFINLAR
Look-Alike Drug Names
- A® — B®[1]
Drug Shortage Status
Price
References
The contents of this FDA label are provided by the National Library of Medicine.
- ↑ "http://www.ismp.org". External link in
|title=(help)
{{#subobject:
|Label Page=Dabrafenib mesylate |Label Name=Tafinlar fig.jpg
}}
{{#subobject:
|Label Page=Dabrafenib mesylate |Label Name=Tafinlar ingredients and appearance.png
}}