Congestive heart failure
| Heart failure | |
| ICD-10 | I50.0 |
|---|---|
| ICD-9 | 428.0 |
| DiseasesDB | 16209 |
| MedlinePlus | 000158 |
| eMedicine | med/3552 |
| MeSH | D006333 |
| Cardiology Network |
 Discuss Congestive heart failure further in the WikiDoc Cardiology Network |
| Adult Congenital |
|---|
| Biomarkers |
| Cardiac Rehabilitation |
| Congestive Heart Failure |
| CT Angiography |
| Echocardiography |
| Electrophysiology |
| Cardiology General |
| Genetics |
| Health Economics |
| Hypertension |
| Interventional Cardiology |
| MRI |
| Nuclear Cardiology |
| Peripheral Arterial Disease |
| Prevention |
| Public Policy |
| Pulmonary Embolism |
| Stable Angina |
| Valvular Heart Disease |
| Vascular Medicine |
Template:WikiDoc Cardiology News Editor-In-Chief: C. Michael Gibson, M.S., M.D. [1]
Associate Editor-In-Chief: Cafer Zorkun, M.D., Ph.D. [2]
Please Join in Editing This Page and Apply to be an Editor-In-Chief for this topic: There can be one or more than one Editor-In-Chief. You may also apply to be an Associate Editor-In-Chief of one of the subtopics below. Please mail us [3] to indicate your interest in serving either as an Editor-In-Chief of the entire topic or as an Associate Editor-In-Chief for a subtopic. Please be sure to attach your CV and or biographical sketch.
Synonyms and Related Key Words: CHF, pump failure, left heart failure, right heart failure, chronic heart failure, acute heart failure, flash pulmonary edema, congestion, systolic dysfunction, LV dysfunction, LV failure, impaired filling, reduced cardiac output, pulmonary edema
Overview
- Clinical syndrome resulting from inadequate systemic perfusion from any structural or functional disorder that impairs the ability of the ventricle to fill with or eject blood.
- The classic syndrome of heart failure is dyspnea, fatigue, and fluid retention.
- There are two broad categories of heart failure:
- Systolic Heart Failure and
- Diastolic Heart Failure.
Differential Diagnosis of Causes of Heart Failure
A. Left Ventricular Failure
Most Common Causes:
Expanded List of Causes:
- Atrial fibrillation
- Alcoholism
- Anemia
- Angina
- Aortic regurgitation
- Aortic Stenosis
- Arteriovenous fistula
- Beriberi
- Cardiac aneurysm
- Cardiomyopathy
- Constrictive pericarditis
- Drugs, toxins
- Hypertension
- Hyperthyroidism
- Hypovolemia
- Hypoxia
- Mediastinal tumors
- Mitral Regurgitation
- Myocardial Infarction
- Paget's Disease
- Pancoast's Tumor
- Pericardial effusion
- Pericardial tamponade
- Perimyocarditis
- Protein deficiency
- Restrictive cardiomyopathy
- Rupture of the papillary muscles
- Sepsis
- Vena Cava Superior Thrombosis
B. Right Ventricular Failure
Most Common Causes:
- Cardiomyopathy
- Cor pulmonale
- Diffuse myocarditis
- Left heart failure
Other Causes:
- After left ventricular failure
- After pulmonary resection
- Allergic alveolitis
- Bronchial asthma
- Chronic bronchitis
- Honeycomb lung
- Hyperglobulia
- Emphysema
- Mitral Stenosis
- Right ventricular myocardial infarction
- Pickwickian Syndrome
- Pleural fibrosis
- Pneumoconiosis
- Pulmonary fibrosis
- Pulmonic regurgitation
- Pulmonic stenosis
- Sarcoidosis
- Severe relapsing pulmonary emboli
- Silicosis
- Tachycardia
- Tricuspid insufficiency
C. Others
- Ascorbic acid deficiency
- Cardiac amyloidosis
- Carnitine deficiency
- Cervical vein stasis of non-cardiac genesis
- Congenital heart disease
- Cyanosis of non-cardiac genesis
- Diabetes Mellitus
- Dyspnea of non-cardiac genesis
- Edema of non-cardiac genesis
- Hemochromatosis
- Pleural effusion of non-cardiac genesis
- Pulmonary edema of non-cardiac genesis
- Thiamine deficiency
- Thyroid disease
Pathophysiology & Etiology
- There are several general causes of heart failure. Heart failure may be of pericardial origin such as tamponade and pericardial constriction, valvular such as aortic or mitral regurgitation; myocardial such as idiopathic dilated cardiomyopathy, familial dilated cardiomyopathy, ischemic cardiomyopathy, and valvular cardiomyopathy; coronary vascular such as acute ischemic episodes, and rhythm disturbances such as tachycardia-induced heart failure.
- Cardiac output can be maintained if LV dilation occurs and stroke volume is preserved even though the LVEF is low.
- As LV dilation occurs, functional mitral regurgitation (MR) may develop despite an anatomically normal mitral valve.
- The ejection fraction is usually below 35% in symptomatic patients.
- Rales usually develop if the pulmonary capillary wedge pressure is >25 mm Hg. Rales may not be present in the patient with chronic heart failure. Rales may develop at even lower pressures if LV function deteriorates suddenly.
- Dyspnea and orthopnea occur due to interstitial edema at lower pressures.
- Hypoperfusion at rest is suggested by cool extremities, altered mentation, and declining renal function.
- EKG often shows low voltage. The differential diagnosis of low voltage on the EKG includes amyloid.
- Poor R wave progression in the precordial leads and LBBB are both common with both ischemic and non-ischemic causes.
- Since the LV often dilates in the anteroposterior direction, the cardiac silhouette may appear deceptively normal. Once the heart failure is advanced, the enlarged right ventricle forms the left border of the cardiac silhouette.
- The presence of enlargement of vessels to the upper lobes, per bronchial cuffing, and pulmonary interstitial and alveolar edema are all indicative of pulmonary venous hypertension.
- As part of the diagnostic maneuvers check the serum TSH and iron levels. Check TSH particularly in those e patients treated with amiodarone.
- Decompensation; most often is non compliance with therapeutic regimens.
- Atrial fibrillation is a major target of therapy. It occurs in 20% of patients with congestive heart failure.
- Other secondary causes include anemia, obesity, drugs [(such as first generation calcium channel blockers, disopyramide, and sotalol, NSAIDs (may cause fluid retention), beta blockers (may cause heart failure with their negative inotropic effects)].
Epidemiology of Heart Failure
Prevalance
- Estimated 2005 prevalence in adults age 20 and older: 5,300,000 (about 2,650,000 males, and 2,650,000 females).
Incidence [1]
- Data from the NHLBI’s Framingham Heart Study indicate that;[2]
- Heart failure (HF) incidence approaches 10 per 1,000 population after age 65.
- 75% of heart failure cases have antecedent hypertension. About 22% of male and 46% of female myocardial infarction (MI) victims will be disabled with heart failure within following 6 years.
- At age 40, the lifetime risk of developing heart failure for both men and women is 1 in 5.
- At age 40, the lifetime risk of heart failure occurring without antecedent myocardial infarction is 1 in 9 for men and 1 in 6 for women.
- The lifetime risk doubles for people with blood pressure >160/90 mm Hg compared to those with blood pressure <140/90 mm Hg.
- A study conducted in Olmsted County, Minnesota, showed that the incidence of heart failure (ICD9/428) has not declined during two decades, but survival after onset has increased overall, with less improvement among women and elderly persons. [3]
Classification Schemes of Heart Failure
Framingham Criteria
Major Criteria
- Paroxysmal nocturnal dyspnea
- Jugular vein distention
- Rales
- Radiographic cardiomegaly
- Acute pulmonary edema
- S3
- Central venous pressure > 16 cmH2O
- Circulation time ≥ 25 sec
- Hepatojugular reflux
- Pulmonary edema
- Visceral congestion
- Cardiomegaly at autopsy
- Weight loss ≥ 4.5 kg in 5 days in response to treatment of heart failure
Minor Criteria
- Bilateral ankle edema
- Nocturnal cough
- Dyspnea on ordinary exertion
- Hepatomegaly
- Pleural effusion
- 30% decrease in baseline vital capacity
- Tachycardia
Boston Criteria of Congestive Heart Failure
- Category I: History
- Rest dyspnea 4 points
- Orthopnea 4 points
- Paroxysmal nocturnal dyspnea 3 points
- Dyspnea on walking on level ground 2 points
- Dyspnea on climbing 1 point
- Category II: Physical Examination
- Heart rate abnormality (1 point if 91 to 110 bpm; if >110 bpm, 2 points)
- Jugular venous pressure elevation (2 points if >6 cm H2O; 3 points if >6 cm H2O and hepatomegaly or edema))
- Lung crackles (1 point if basilar; 2 points if more than basilar)
- Wheezing 3 points
- Third heart sound 3 points
- Category III: Chest Radiography
- Alveolar pulmonary edema 4 points
- Interstitial pulmonary edema 3 points
- Bilateral pleural effusion 3 points
- Cardiothoracic ratio >0.50 (posteroanterior projection) 3 points
- Upper zone flow redistribution 2 points
No more than 4 points are allowed from each of three categories; hence the composite score (the sum of the subtotal from each category) has a possible maximum of 12 points.
The diagnosis of heart failure is classified as "definite" at a score of 8 to 12 points, "possible" at a score of 5 to 7 points, and "unlikely" at a score of 4 points or less.
New York Heart Association Criteria (NYHA)
- NYHA I: No symptoms with ordinary activity.
- NYHA II: Slight limitation of physical activity. Comfortable at rest, but ordinary physical activity results in fatigue, palpitation, dyspnea, or angina.
- NYHA III: Marked limitation of physical activity. Comfortable at rest, but less than ordinary physical activity results in fatigue, palpitation, dyspnea, or anginal pain.
- NYHA IV: Unable to carry out any physical activity without discomfort. Symptoms of cardiac insufficiency present at rest.
ACC/AHA Classification of Chronic Heart Failure
Classification System based on structural and symptomatic stages of the syndrome.
Stage 1: patients at risk of developing heart failure but who have no structural heart disease at present. Stage 2: patients with structural heart disease but no symptoms. Stage 3: patients with structural heart disease and symptomatic heart failure. Stage 4: patients with severe refractory heart failure.
Stage 1
Patients “at Risk”
- Hypertension
- Diabetes mellitus
- Coronary artery disease
- Exposure history to cardiac toxins:
- History of cardiotoxic drug therapy.
- History of alcohol abuse.
- Familial history of cardiomyopathy
Stage 2
Patients with structural heart disease, but no history of signs or symptoms of heart failure.
- Left ventricular hypertrophy (LVH)
- Myocardial fibrosis
- Left ventricular dilatation or dysfunction
- Asymptomatic valvular heart disease
- Previous myocardial infarction
Stage 3
Underlying structural heart disease and symptoms of heart failure.
- Dyspnea or fatigue due to left ventricular systolic dysfunction.
- Asymptomatic patients receiving treatment for prior symptoms of heart failure.
Stage 4
Despite of maximal medical therapy, symptoms of heart failure at rest and advanced structural heart disease.
- Awaiting for heart transplantation
- Requiring continuous inotropic or mechanical support
- Hospital management of heart failure
Risk Factors for the Development of Heart Failure
- Demographic factors
- Age
- Gender
- Low socioeconomic status
- Lifestyle-related factors
- Tobacco and coffee consumption
- Alcohol consumption
- Dietary sodium intake
- Recreational drug use: Cocaine, methamphetamines.
- Comorbidities
- Echocardiographic factors
- Ventricular dimension
- Ventricular mass
- Diastolic filling impairment
- Pharmacological factors
- Chemotherapeutic agents
- Non-steroidal anti-inflammatory drugs
- Thiazolidinediones?
- Doxazosin
- Biochemical
- Albuminuria
- Homocysteine: Elevated plasma homocysteine levels are associated with almost a 75% increase in risk for heart failure development.
- Tumor necrosis factor-alpha (TNF-alpha): After adjustment for other risk factors, every tertile increment in tumor necrosis factor-alpha (TNF-alpha) levels was associated with a 60% increase in risk of heart failure. TNF-alpha has several negative pleiotropic effects and also negative inotropic properties that may be responsible for excessive heart failure risk. TNF-alpha is also associated with progression of heart failure.
- Interleukin-6: IL-6 is a pro-inflammatory cytokine which associated with an excessive risk of development of heart failure.
- C-reactive protein
- Insulin-like growth factor-I (IGF-I)
- Natriuretic peptides
- Genetic risk factors
Risk Factors Associated with Heart Failure Progression and Outcomes
- Clinical
- Etiology
- Age
- Gender
- Symptom duration
- NYHA class
- Weight
- Heart rate
- Mean arterial pressure
- S3 gallop
- Jugular venous pressure
- Cardiothoracic ratio
- Renal function
- Serum sodium
- Troponin T
- History of diabetes
- Anemia
- Echocardiographic
- Ejection fraction
- Exercise ejection fraction
- Ventricular dimensions
- Sphericity index
- Prolonged isovolumic relaxation
- Restrictive mitral filling
- Changes in E/A ratio
- Mitral regurgitation
- Contractile reserve
- Left ventricular mass
- Exercise Tolerance
- Exercise duration
- Peak O2 consumption
- VE/VCO2
- Anaerobic threshold 6-minute walk test
- Hemodynamics
- Cardiac index
- Pulmonary artery pressure
- Pulmonary artery wedge pressure
- Pulmonary vascular resistance
- Stroke work index
- Right atrial pressure
- A-V oxygen difference
- Coronary sinus O2 content
- Electrophysiological
- Conduction delay
- Atrial arrhythmia
- Family history of sudden death
- Presence of late potentials
- QT dispersion
- T wave alternans
- Neurohormonal
- Renin-angiotensin system
- Angiotensin II
- Aldosterone
- Plasma renin activity
- Sympathetic nervous system
- Norepinephrine
- Epinephrine
- Heart rate variability
- Norepinephrine spillover
- Natriuretic factors
- Atrial natriuretic peptide
- B-type natriuretic peptide
- N-terminal-pro-ANP
- Cytokines and others
Differential Diagnosis of Heart Failure
Heart Failure Secondary to Coronary Artery Disease
A. Underlying Mechanisms
- Ischemic Preconditioning
- Reductions in ischemia-related apoptosis
- Increases in endogenous adenosine
- Activation of potassium-adenosine triphosphate (K+-ATP) channels
- Electrical Dysfunction
- QT prolongation
- Increased susceptibility to arrhythmia
- QT dispersion
- Mechanical Dysfunction
- Systolic dysfunction
- Diastolic dysfunction
- Biochemical Dysfunction
- Increases in beta-adrenergic receptor density
- Changes in structural and regulatory proteins
- Shift to FFA as a proffered metabolic substrate
- Lactate production
- Elevated BNP concentration
B. Utilisation of Clinical Data
Management of heart failure due to coronary artery disease are primarily influenced by following parameters:
- An estimate of the relative proportions of:
- Viable but ischemic myocardium
- Nonviable myocardium
- Viable non-ischemic myocardium
- The technical feasibility of successful mechanical revascularization
- The extent and severity of comorbidities in the individual patient
Cardiomyopathies and Inflammatory Diseases
Restrictive Cardiomyopathies
- Primary (idiopathic)
- Tumor infiltration
- Amyloidosis
- Storage diseases
- Endocardial fibrosis
- Anthracyclines
- Eosinophilic heart disease
- Radiation
- Hemochromatosis
- Cardiac transplant
- Sarcoidosis
Dilated Cardiomyopathies
- Duchenne muscular dystrophy
- Becker's muscular dystrophy
- Limb-girdle muscular dystrophy
- Mitochondrial myopathy
- Arrhythmogenic right ventricular dysplasia
- Alcohol-Induced cardiomyopathy
- Cocaine related cardiomyopathy
- Diabetic cardiomyopathy
- Peripartum cardiomyopathy
- Anthracycline induced cardiomyopathy
- Trastuzumab Herceptin-lnduced Cardiomyopathy
Inflammations
- Viral Myocarditis
- Rickettsial Myocarditis
- Bacterial Myocarditis
- Spirochetal Infections
- Protozoal Myocarditis: Trypanosomiasis (Chagas Disease)
- Fungal myocarditis
- Giant Cell Myocarditis
- Sarcoidosis
Congestive Heart Failure as a Consequence of Valvular Heart Disease
- Aortic stenosis with Left Ventricular Systolic Dysfunction
- Chronic aortic regurgitation
- Mitral Stenosis
- Chronic mitral regurgitation
- Acute aortic regurgitation
- Acute mitral regurgitation
Congestive Hert Failure Secondary to Congenital Heart Disease
A. Causes of Congestive Heart Failure in Adults with Unoperated Congenital Heart Diseases
- Eisenmenger's syndrome
- Fibrocalcific degeneration of abnormal aortic valve
- Systemic ventricular dysfunction and/or tricuspid regurgitation in congenitally corrected transposition of the great arteries
- Atrial septal defect with mitral regurgitation] secondary to myxomatous mitral valve
- Congenital mitral regurgitation
- Arrhythmia
- Endocarditis
- Other degenerative diseases (coronary artery disease, hypertension)
- Drug abuse, alcohol abuse
- Pregnancy
B. Causes of Congestive Heart Failure in Adults with Operated Congenital Heart Diseases
- Myocardial dysfunction
- Valvular regurgitation
- Persistent left-to-right shunt
- Pulmonary vascular disease
- Prosthetic valve dysfunction
- Status post Fontan operation
- Arrhythmia
- Endocarditis
- Other degenerative diseases (coronary artery disease, hypertension)
Right Ventricular Failure
Factors affected right ventricle and to be eliminated during management of congestive heart failure. A. Right ventricular myocardial dysfunction
B. Primary right ventricular pressure overload
- Left ventricular failure
- Mitral valve disease
- Atrial myxoma
- Pulmonary veno-occlusive disease
- Cor pulmonale
- Pulmonic stenosis
- Ventricular septal defect
- Aortopulmonary communication
C. Primary right ventricular volume overload
- Pulmonic regurgitation
- Tricuspid regurgitation
- Atrial septal defect
- Partial anomalous pulmonary venous return
D. Impediment to right ventricular inflow
Heart Failure in Cardiac Tamponade, Constrictive Pericarditis, and Restrictive Cardiomyopathy
Electrocardiography
- Electrocardiograms have no definitive but only suggestive findings.
- Left ventricular hypertrophy, left bundle branch block, intraventricular conduction delay, chamber enlargement, non-specific ST segment and T wave changes.
Chest X-ray
- Cardiac enlargement
- Pulmonary congestion (Kerley B lines, and pleural effusion)
Echocardiography
- Evaluation of left ventricular function and ejection fraction
- Wall motion abnormalities
- Detection of mitral regurgitation
- Detection of aortic stenosis
- Measurement of pulmonary artery pressure
- Detection and evaluation of aneurysms
Exercise Stress Tests
Exercise Stress Tests is useful in measuring the "functional capacity" of patients. It is also helpful in follow up period for evaluation of congestive heart failure treatment.
Myocardial Viability Studies
- Dobutamine echocardiography
- Nuclear tests (SPECT or PET)
- Cardiac MRI
Cardiac Catheterization
Coronary angiography for evaluation of coronary arteries and right heart catheterization for assessment of pulmonary artery resistance.
Management of Heart Failure
Pharmacotherapy
A. Acute Pharmacotherapy
B. Chronic Pharmacotherapy
Antiarrhythmic Drugs
Antiarrhythmic therapy should be considered as a therapy to prevent sudden death. There are multiple causes of the for sudden death including ventricular tachycardia, ventricular fibrillation as low as pulmonary emboli, hyperkalemia, and primary bradyarrhythmias.
Over 50% of patients will have asymptomatic non-sustained ventricular tachycardia and there is no general indication for treatment of this arrhythmia.
Metabolisms of following anti-arrhythmic drugs are significantly affected in patients with congestive heart failure;
- Quinidine
- Procainamide
- Disopyramide: Contraindicated in patients with heart failure.
- Moricizine
- Lidocaine
- Mexiletine
- Tocainide
- Flecainide
- Propafenone
- Amiodarone
Renin-Angiotensin-Aldosteron System Related Drugs
- ACE Inhibitors
- ACE Inhibitors (ACEI) should be considered as first-line therapy for the treatment of patients with clinical heart failure due to reduced LVSD, patients with asymptomatic LV dysfunction, and for patients who are at high risk for the development of heart failure due to the presence of coronary, cerebrovascular, or peripheral vascular disease.
- Treatment should not be deferred in patients with few or no symptoms because of the significant mortality benefit derived from ACEI therapy.
- Initial therapy usually consist of 12.5 mg tid of captopril, 2.5 mg bid of enalapril, or 2.5 mg daily lisinopril. The optimal dose is usually established by change 4 to 6 weeks. ACE inhibitors are rarely adequate for the treatment of congestion without the use of diuretics.
- 5-10 % patients cannot tolerate ACE inhibitors because of cough. Cough can be a sign of elevated left-sided filling pressures. Sometimes cough will diminish with the treatment of heart failure. Angiotensin 2 receptor blockers are now being studied as a substitute for ACE inhibitors. Renal artery stenosis should be considered if there's a decline in renal function with the initiation of ACE inhibitors.
- Angiotensin receptor blockers (ARB)
- Aldosterone Antagonists
Anticoagulants
The annual incidence of systemic and pulmonary embolism in patients with heart failure is 2-5%. This is not that is similar from the risk of severe bleeding among patients to its anticoagulants which is 0.8-2.5% per year.
As a result anticoagulation is not routinely recommended in the current guidelines for the treatment of heart failure. However among those patients with a atrial fibrillation, a history of emboli, or multiple intracardiac thrombi, or akinesis or dyskinesis detected on echo should be anticoagulated.
Beta Blockers
- Metoprolol, Carvedilol and Bisoprolol have FDA approval.
- Blockade of compensatory sympathetic stimulation creates an arrhythmic, ischemic, remodeling, and apoptotic benefit.
- Used as monotherapy or combined with conventional heart failure management, beta-blockers reduce the combined risk of morbidity and mortality.
- Initiate low starting dosing and titrate up to tolerated target doses.
- Bisoprolol
- Bucindolol
- Carvedilol
- Metoprolol
- Nevibolol
Ca Channel Blockers
Although calcium channel blockers cause vasodilation their overall benefit is minimized by the fact that they have a negative inotropic effect and by the reflex activation of the sympathetic nervous system.
These agents are not recommended as vasodilators in patients with congestive heart failure, however they may be useful as antihypertensive agents in patients with diastolic dysfunction.
Diuretics
- Provide symptomatic relief.
- Slows the progression of ventricular remodeling by reducing ventricular filling pressure and wall stress.
- No survival benefit and may cause azotemia, hypokalemia, metabolic alkalosis and elevation of neurohormones.
- Although thiazide diuretics are effective in mild heart failure they are usually inadequate for the treatment of severe heart failure.
- Thiazide diuretics have also been associative with hyponatremia.
- Fluid retention usually responds best to furosemide (Lasix) and at doses of 10 to 20 mg per day. The patient should be told to return to their position in the next three to seven days for further assessment including assessment of their potassium concentration. Weight loss should not exceed 1 to 2 pounds/day.
- If there is no response to the initial dose then it can be increased by at least 50%. The maintenance dose of the diuretics lower than that required to initiate diuresis.
- If the patient gains more than two pounds and they are instructed to double the dose of their loop diuretic.
- Once the baseline weight has been re-established than they can resume their previous status.
- Intermittent use of metolazone into dose of 2.5 or 5 mg can be given if the patient is refractory to furosemide Lasix. Metolazone should be given in the inpatient setting.
- The role of potassium sparing diuretics such as spironolactone (Aldactone), amiloride, or triamterene remains the subject of controversy.
- Extreme caution is necessary when adding a potassium sparing agent to the regiment that includes ACE inhibitors particularly when diabetes or renal disease is present because the patient can become hyperkalemic.
- Electrolyte replacement:
ACE inhibitors reduce potassium excretion, but most patients with good renal function require potassium supplementation during daily therapy with the diuretics such as furosemide (Lasix) despite of ACE inhibitors therapy.
- Dietary supplementation is rarely adequate.
- Hypokalemia can aggravate arrhythmia is precipitate muscle cramps.
- Potassium levels >6 (particularly when occurs rapidly) can be associated with reduction in myocardial contractility.
- Patients are actually at higher risk of hyperkalemia and hypokalemia. The goal is to maintain a potassium between 3.8 and 4.5 mEq.
- Unless the hypokalemia is very severe and at life-threatening level, potassium should be replaced by oral administration.
- For IV route, It should not be administered more than 10 mEq per hour.
- Patients who use diuretics usually require approximately 20-60 mEq/day of oral potassium.
- Extra potassium should be given after the patient has noted diuresis or weight change. If patient lost more than two pounds, the electrolyte's level should be checked every three days.
Loop Diuretics
- Furosemide, bumetanide, ethacrynic acid and torsemide.
- Inhibit the Na+/K+/2Cl- symporter.
- Furosemide IV has direct vasodilatory effect.
- Providing additional blood pressure reduction.
- Relaxes pre-contracted pulmonary venules: beneficial for treatment of Pulmonary Edema.
Thiazide Diuretics
- Inhibit the Na+/Cl- co transporter in the distal convoluted tube.
- Recommended for management of chronic heart failure.
Potassium Sparing Diuretics
- Spironolactone, amiloride and triamterene.
- Inhibit principal cells in the distal convoluted tubule and cortical collecting duct.
- Inhibits Na reabsorbtion and Potassium secretion.
- Their significant side effect is hyperkalemia.
Nitrates
- Nitrates can be added to ACE inhibitors to relieve symptoms of congestion.
- The addition of a nitrate and ACE inhibitor may improve exercised tolerance.
- The combination of hydralazine and nitrates is useful when ACE inhibitors are not well tolerated.
- Hydralazine by itself is only an arterial vasodilator and does not reduced ventricular filling pressures to the same extent that nitrates and ACE inhibitors do. In fact when used alone it can stimulate sympathetic tone reflexively. The combination of hydralazine and nitrates has been shown to decrease mortality as well as improve the left ventricular ejection fraction and exercise capacity in patients with heart failure. However the combination of hydralazine and nitrates has been found to be less effective than ACE inhibitors.
- The major uses this combination is in those patients who are intolerant of ACE inhibitors.
Positive Inotropics
- Agents that increase intracellular cAMP
- Alpha-adrenergic agonists
- Phosphodiesterase inhibitors
- Agents that affect sarcolemmal ion pumps/channels
- Agents that modulate intracellular calcium mechanisms by either:
- Release of sarcoplasmic reticulum calcium (IP3)
- Increased sensitization of the contractile proteins to calcium
- Drugs having multiple mechanisms of action
- Pimobendan
- Vesnarinone
Digoxin
- Inhibits Na,K+-ATPase resulting in an increase in intracellular Na+, extracellular Ca2+ exchange increasing the velocity and extent of sarcomere shortening.
- ACC/AHA recommend digoxin for symptomatic patients with left ventricular systolic dysfunction.
- Commonly used in patients with heart failure and atrial fibrillation to reduce the ventricular response rate.
- Mortality has not been shown to be improved with use of digoxin, but the use of digoxin has been associated with a reduction in hospitalization.
- There is no need to load a patient with digoxin for most patients with normal renal function 0.25 mg of digoxin daily is usually adequate. In the only patient or in those patients with renal impairment a dose of 0.125 mg per day may be adequate.
- Drugs increase the same concentration of digoxin include antibiotics and anticholinergic agents as well as amiodarone, quinidine and verapamil.
Dobutamine
- Activates beta-1 receptors resulting in enhanced cardiac contractility.
- Long-term dobutamine infusions are arrhythmogenic and increase mortality.
Dopamine
- Unique dose dependent mechanism of action.
- At low doses: (≤2 µg/kg/min), selective dilation of splanchnic and renal arterial beds. assists in increasing renal perfusion.
- At intermediate doses: (2 to 10 µg/kg/min), increased norepinephrine secretion results in increased cardiac contractility, heart rate and peripheral vascular resistance.
- At higher doses: (5 to 20 µg/kg/min), direct alpha-adrenergic receptor stimulation increases systemic vascular resistance.
Milrinone
- Phosphodiesterase-III inhibitor that enhances contractility by increasing intracellular cyclic adenosine monophosphate (cAMP).
- Potent pulmonary vasodilatation that benefits pts with pulmonary hypertension.
- Unlike dobutamine: milrinone is beneficial to decompensated heart failure patients on beta-blocker therapy.
- Long term milrinone infusions are arrhythmogenic, and increase mortality.
Biventricular Pacing
Biventricular pacing or cardiac resynchronization therapy is;
- Indicated for symptomatic patients with NYHA III-IV heart failure and wide QRS complex (>120ms).
- 70% of patients receiving synchronous ventricular contraction report significant symptomatic improvements.
Implantation of Intracardiac Defibrillator
- 50% of heart failure patients die of sudden cardiac death.
- ICDs are indicated for patients with previous myocardial infarction and LVEF <30%, sustained ventricular tachycardia, inducible ventricular tachycardia.
- Morbidity/mortality benefit of ICD placement vs. anti-arrhythmic drug therapy is controversial.
Ultrafiltration
The process of ultrafiltration consists of the production of plasma water from whole blood across a semipermeable membrane (hemofilter) in response to a transmembrane pressure gradient. Possible benefits of ultrafiltration as follow;
- Provides fluid regulation
- Relieve pulmonary edema
- Reduce ascites and/or peripheral edema
- Hemodynamic stabilization
- Improve oxygenation
- Facilitate blood product replacement without excess volume
- Enable parenteral nutritional support without excess volume
- Improves solute regulation
- Correct acid-base balance
- Correct serum sodium content
- Eliminate myocardial depressant factors or known toxins
- Correct uremia
- Correct hyperkalemia
- Correct other electrolyte disturbances
- Helps to establish homeostasis
- Reset water omostat
- Restore diuretic responsiveness
- Reduce neurohormonal activation
Cardiac Surgery
- Resection of non-viable myocardium
- Revascularization without resection of non-viable myocardium
- Dor procedure: Surgical resection of infarcted myocardium and left ventricular reconstruction.
- Placement of a passive containment device to prevent progressive cardiac dilation (Under investigation)
Left Ventricular Assist Devices
- LVADs are temporary devices to bridge end stage patients to cardiac transplantation.
- Current clinical research in implementing permanent portable LVADs is underway, and first studies have promising results.
Cardiac Transplantation
- For patients with end-stage congestive heart failure despite all interventions.
- 80% 1 year survival and 60% 5 year survival.
- Lifelong immunosuppressive therapy to prevent (or postpone) rejection, increased risk for opportunistic infections and malignancies.
AHA/ACC Guidelines: Indications for heart transplantation
- Any hemodynamic compromise due to heart failure.
- Requiring IV inotropic support to maintain adequate organ perfusion.
- Peak Vo2 <10 ml/kg/min.
- NYHA Class IV symptoms not amenable to any other intervention.
- Recurrence of symptomatic ventricular arrhythmias refractory to all therapeutic intervention.
Exercise and Daily Activities
- Patient should have uninterrupted exercise at least four days a week including a walking program.
- Rowing machines usually are too vigorous of exercise.
- Patients with heart failure should avoid weightlifting.
- The patient should not routinely lift more than 20 pounds.
- Patients can continue their sexual activity. Some patients take 2.5 or 5.0 mg of sublingual nitroglycerin before sexual activity.
Prognosis
Mortality Associated with Heart Failure
Based on the 44-year follow-up of the NHLBI’s Framingham Heart Study:
- 80% of men and 70% of women under age 65 who have heart failure will die within following 8 years.
- In people diagnosed with heart failure, sudden cardiac death occurs at 6 to 9 times the rate of the general population.
- One in eight deaths has heart failure mentioned on the death certificate.
Hospital Discharges
- Hospital discharges for heart failure rose from 400,000 in 1979 to 1,084,000 in 2005, an increase of 171%. (NHDS / NHLBI and AHA calculations).
Cost
• The estimated direct and indirect cost of heart failure in the United States for 2008 is $34.8 billion.
Pathological Findings
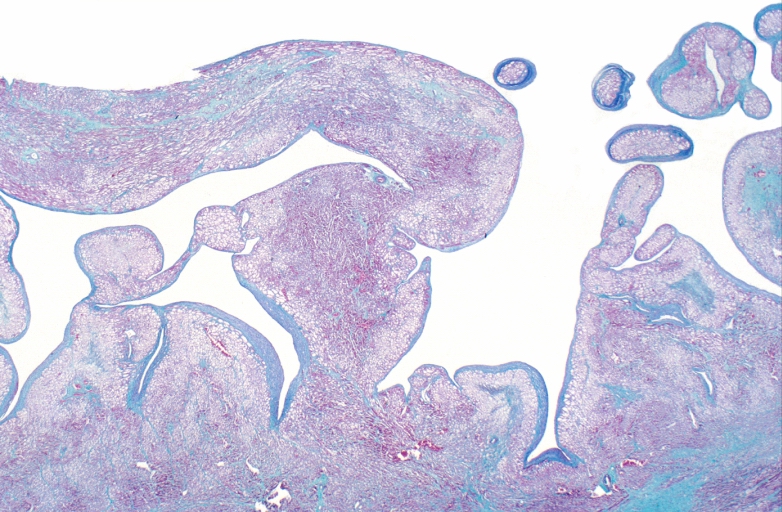
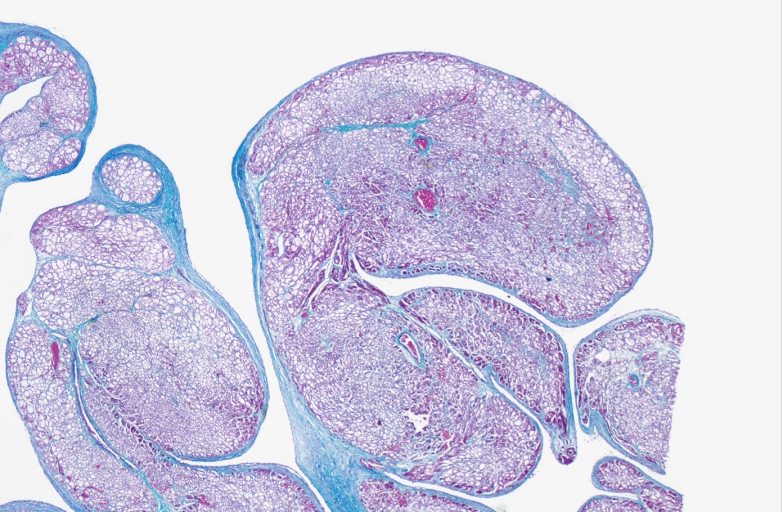
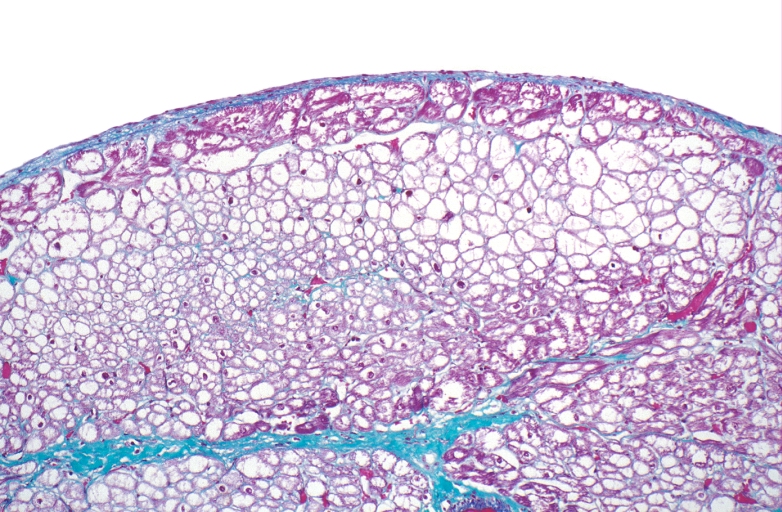
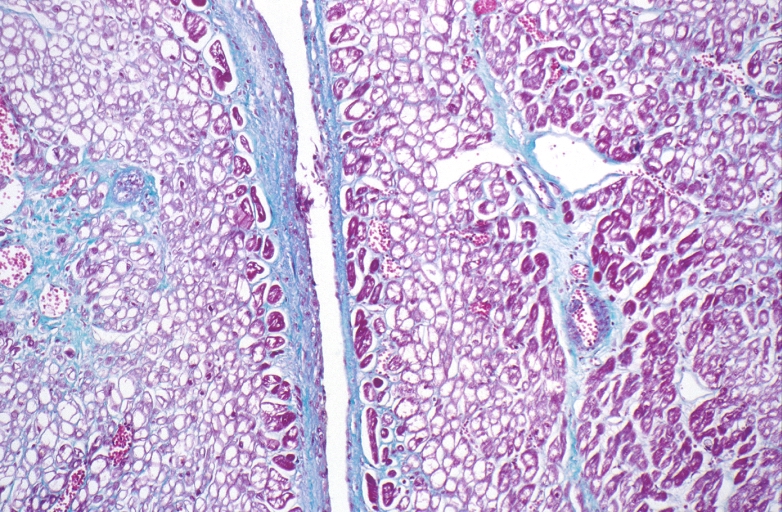
-
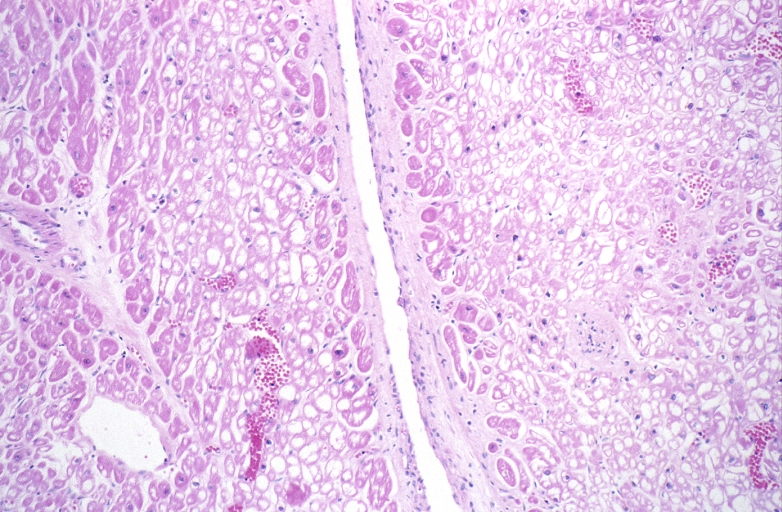
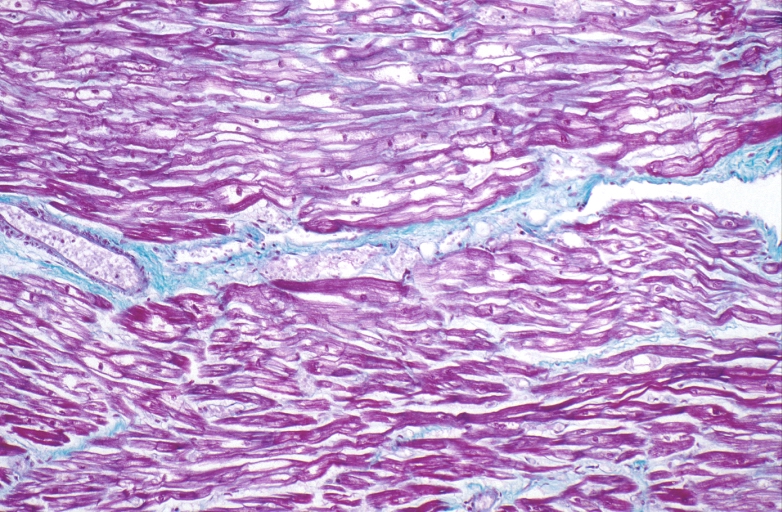
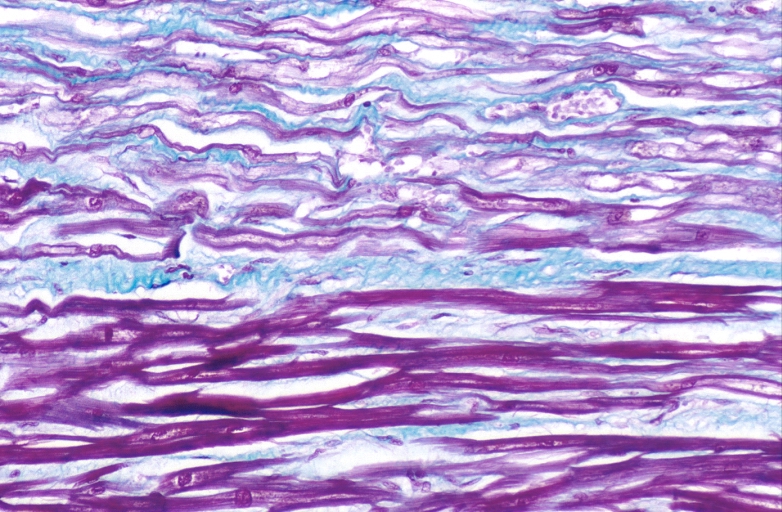
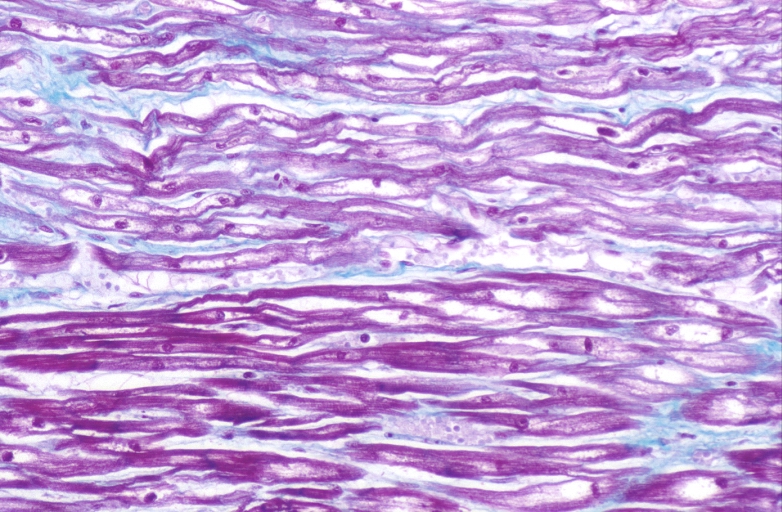
HEART: Congestive heart failure, hydropic change
-
HEART: Congestive heart failure, hydropic change
-
HEART: Congestive heart failure, hydropic change
-
HEART: Congestive heart failure, hydropic change
-
HEART: Congestive heart failure, hydropic change
-
HEART: Congestive heart failure, hydropic change
-
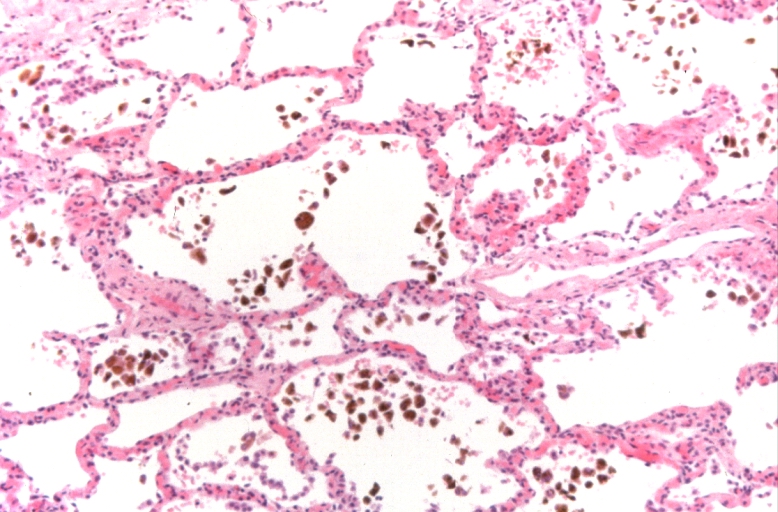
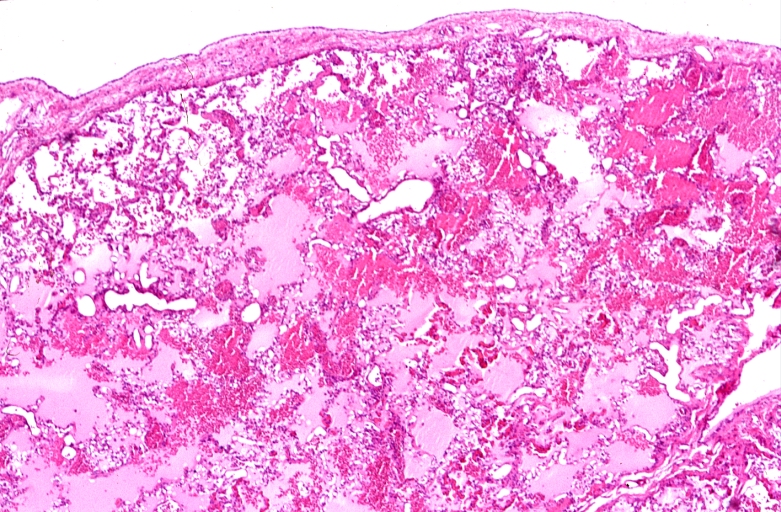
Lung, congestion, heart failure cells (hemosiderin laden macrophages)
-
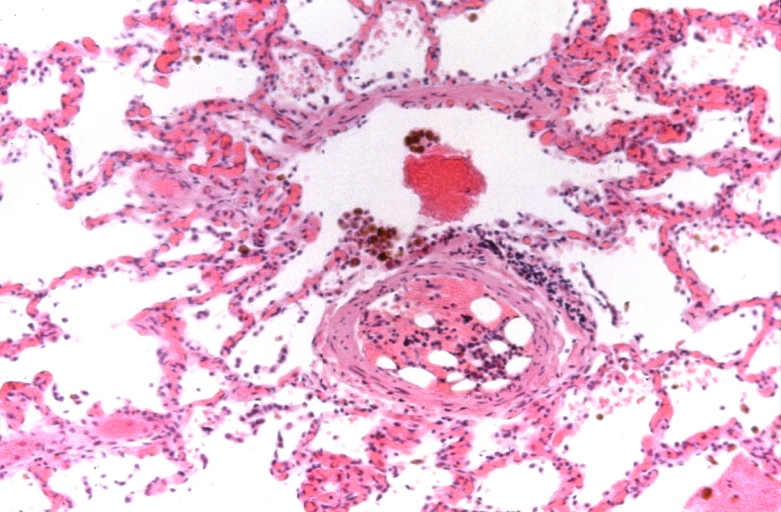
Lung, Congestive Heart Failure, bone marrow embolus
-
Lung, pulmonary edema in patient with congestive heart failure due to heart transplant rejection
-
HEART: Congestive heart failure, hydropic change
-
HEART Congestive heart failure, hydropic change
-
Spleen, congestion, congestive heart failure
References
- ↑ Disease and Stroke Statistics - 2008 Update, American Heart Association. Accessed on 09 March 2008
- ↑ Lloyd-Jones DM, Larson MG, Leip EP, Beiser A, D'Agostino RB, Kannel WB, Murabito JM, Vasan RS, Benjamin EJ, Levy D; Lifetime Risk for Developing Congestive Heart Failure. Framingham Heart Study. Circulation. 2002; 106: 3068–72 PMID 12473553
- ↑ Véronique L. Roger, Susan A. Weston, Margaret M. Redfield, Jens P. Hellermann-Homan, Jill Killian, Barbara P. Yawn, Steven J. Jacobsen Trends in Heart Failure Incidence and Survival in a Community-Based Population JAMA. 2004; 292: 344-50 PMID 15265849