|
|
| (19 intermediate revisions by the same user not shown) |
| Line 10: |
Line 10: |
| {{Concussion}} | | {{Concussion}} |
|
| |
|
| ==Background== | | ==[[Concussion overview|Overview]]== |
|
| |
|
| |
|
|
| | ==[[Concussion historical perspective|Historical Perspective]]== |
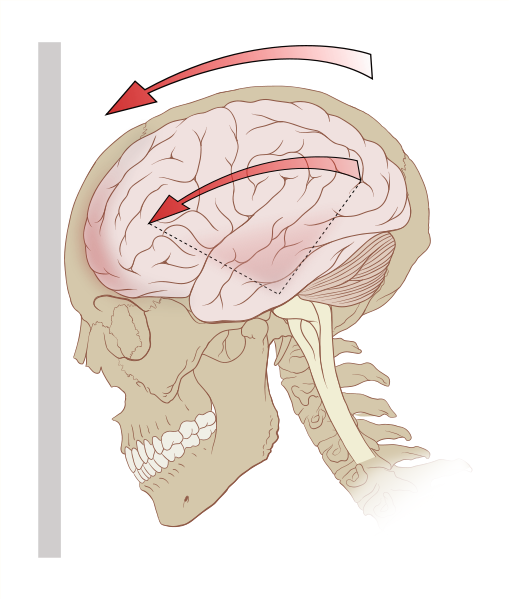
| Due to factors such as widely varying definitions and possible underreporting of concussion, the rate at which it occurs annually is not known; however it may be more than 6 per 1000 people.<ref name="CassidyWHO"/> Common causes include sports injuries, bicycle accidents, auto accidents, and falls; the latter two are the most frequent causes among adults.<ref name="pmid17215534"/> Concussion may be caused by a blow to the head, or by [[acceleration]] or deceleration forces without a direct impact. The forces involved disrupt cellular processes in the [[brain]] for days or weeks.
| |
|
| |
|
| It is not known whether the concussed brain is structurally damaged the way it is in other types of brain injury (albeit to a lesser extent) or whether concussion mainly entails a loss of function with [[physiology|physiological]] but not structural changes.<ref name="Shaw02">
| | ==[[Concussion classification|Classification]]== |
| {{
| |
| cite journal |author=Shaw NA |title=The neurophysiology of concussion |journal=Progress in Neurobiology |volume=67 |issue=4 |pages=281–344 |year=2002 |pmid=12207973 |doi=10.1016/S0301-0082(02)00018-7
| |
| }}
| |
| </ref> Cellular damage has reportedly been found in concussed brains, but it may have been due to artifacts from the studies.<ref name="Rees03"/> A debate about whether structural damage exists in concussion has raged for centuries and is ongoing.
| |
|
| |
|
| ==Definitions== | | ==[[Concussion pathophysiology|Pathophysiology]]== |
| No single definition of concussion, mild head injury,<ref name="SatzZaucha">
| |
| {{
| |
| cite journal |author=Satz P, Zaucha K, McCleary C, Light R, Asarnow R, Becker D |title=Mild head injury in children and adolescents: A review of studies (1970–1995) |journal=Psychological Bulletin |volume=122 |issue=2 |pages=107–131 |year=1997 |pmid=9283296 |doi=
| |
| }}</ref> or mild traumatic brain injury is universally accepted, though a variety of definitions have been offered.<ref name="ComperBisschop">
| |
| {{
| |
| cite journal |author=Comper P, Bisschop SM, Carnide N, Tricco A |title=A systematic review of treatments for mild traumatic brain injury |journal=Brain Injury |volume=19 |issue=11 |pages=863–880 |year=2005 |pmid=16296570 |doi=10.1080-0269050400025042 |issn=0269-9052
| |
| }}
| |
| </ref> In 2001, the first International Symposium on Concussion in Sport was organized by the International Olympic Committee Medical Commission and other sports federations.<ref name="aubry"/> A group of experts called the Concussion in Sport Group met there and defined concussion as "a complex pathophysiological process affecting the brain, induced by traumatic biomechanical forces."<ref name="canturc06">
| |
| {{
| |
| cite journal |author=Cantu RC |date=2006 |url=http://www.aans.org/education/journal/neurosurgical/Oct06/21-4-3-1067.pdf |format=PDF |title=An overview of concussion consensus statements since 2000 |journal=Neurosurgical Focus |volume=21 |issue=4:E3 |pages=1–6
| |
| }}<!-- No PMID found -->
| |
| </ref> They agreed that concussion typically involves temporary impairment of neurological function which quickly resolves by itself, and that [[neuroimaging]] normally shows no gross structural changes to the brain as the result of the condition.<ref name="AndersonT"/>
| |
|
| |
|
| According to the classic definition, no structural brain damage occurs in concussion;<ref>
| | ==[[Concussion causes|Causes]]== |
| {{
| |
| cite journal |author=Parkinson D |year=1999 |title=Concussion confusion |journal=Critical Reviews in Neurosurgery |volume=9 |issue=6 |pages=335–339 |issn=1433-0377 |doi=10.1007/s003290050153
| |
| }}<!--Not indexed on Pubmed--></ref> it is a functional state, meaning that symptoms are caused primarily by temporary [[biochemistry|biochemical]] changes in [[neuron]]s, taking place for example at their [[cell membrane]]s and [[synapse]]s.<ref name="AndersonT"/> However, in recent years researchers have included [[injury|injuries]] in which structural damage does occur under the rubric of concussion. According to the [[National Institute for Health and Clinical Excellence]] definition, concussion may involve a physiological or physical disruption in the brain's [[chemical synapse|synapse]]s.<ref name="NICE">
| |
| {{
| |
| cite web|url=http://www.nice.org.uk/nicemedia/pdf/CG56guidance.pdf|format=PDF |publisher=National Institute for Health and Clinical Excellence |title=Head Injury: Triage, Assessment, Investigation and Early Management of Head Injury in Infants, Children and Adults |isbn=0-9549760-5-3 |date=September 2007 |accessdate=2008-01-26
| |
| }}</ref>
| |
|
| |
|
| Definitions of mild traumatic brain injury (MTBI) have been inconsistent since the 1970s, but the [[World Health Organization]]'s [[ICD-10|International Statistical Classification of Diseases and Related Health Problems]] (ICD-10) described MTBI-related conditions in 1992, providing a consistent, authoritative definition across specialties.<ref name="Petchprapai07"/> In 1993, the American Congress of Rehabilitation Medicine defined MTBI as 30 minutes or fewer of [[loss of consciousness]] (LOC), 24 hours or fewer of [[post-traumatic amnesia]] (PTA), and a [[Glasgow Coma Scale]] (GCS) score of at least 13.<ref name="Kushner98">
| | ==[[Concussion differential diagnosis|Differentiating Concussion from other Diseases]]== |
| {{
| |
| cite journal |author=Kushner D |title=Mild Traumatic brain injury: Toward understanding manifestations and treatment |journal=Archives of Internal Medicine |volume=158 |issue=15 |pages=1617–1624 |year=1998 |pmid=9701095 |doi= |url=http://archinte.highwire.org/cgi/content/full/158/15/1617
| |
| }}</ref> In 1994, the [[American Psychiatric Association]]'s ''[[Diagnostic and Statistical Manual of Mental Disorders]]'' defined MTBI using PTA and LOC.<ref name="Petchprapai07"/> Other definitions of MTBI incorporate focal neurological deficit and altered mental status, in addition to PTA and GCS.<ref name="ComperBisschop"/>
| |
|
| |
|
| Concussion falls under the classification of mild TBI.<ref name="LeeLK07">
| | ==[[Concussion epidemiology and demographics|Epidemiology and Demographics]]== |
| {{
| |
| cite journal |author=Lee LK |title=Controversies in the sequelae of pediatric mild traumatic brain injury |journal=Pediatric Emergency Care |volume=23 |issue=8 |pages=580–583 |year=2007 |pmid=17726422 |doi=10.1097/PEC.0b013e31813444ea
| |
| }}</ref> It is not clear whether concussion is implied in mild brain injury or mild head injury.<ref name=LevinHS>
| |
| {{
| |
| cite book |author=Benton AL, Levin HS, Eisenberg HM |title=Mild Head Injury |publisher=Oxford University Press |location=Oxford [Oxfordshire] |year=1989 |pages=v |isbn=0-19-505301-X |oclc= |doi=
| |
| }}</ref> "MTBI" and "concussion" are often treated as synonyms in medical literature.<ref name="Kushner98"/> However, other injuries such as [[intracranial hemorrhage]]s (e.g. [[intra-axial hematoma]], [[epidural hematoma]], and [[subdural hematoma]]) are not necessarily precluded in MTBI<ref name="AndersonT"/> or mild head injury,<ref name="vanderNaalt">
| |
| {{
| |
| cite journal |author=van der Naalt J |title=Prediction of outcome in mild to moderate head injury: A review |journal=Journal of Clinical and Experimental Neuropsychology |volume=23 |issue=6 |pages=837–851 |year=2001 |pmid=11910548 |doi=10.1076/jcen.23.6.837.1018
| |
| }}</ref><ref name="Savitsky00">
| |
| {{
| |
| cite journal |author=Savitsky EA, Votey SR |title=Current controversies in the management of minor pediatric head injuries |journal=American Journal of Emergency Medicine |volume=18 |issue=1 |pages=96–101 |year=2000 |pmid=10674544 |doi=10.1016/S0735-6757(00)90060-3 |url=
| |
| }}</ref> but they are in concussion.<ref name="ParikhKoch">
| |
| {{
| |
| cite journal |author=Parikh S, Koch M, Narayan RK |title=Traumatic brain injury |journal=International Anesthesiology Clinics |volume=45 |issue=3 |pages=119–135 |year=2007 |pmid=17622833 |doi=10.1097/AIA.0b013e318078cfe7
| |
| }}</ref> MTBI associated with abnormal neuroimaging may be considered "complicated MTBI".<ref name="Iverson2005"/> "Concussion" can be considered to imply a state in which brain function is temporarily impaired and "MTBI" to imply a [[pathophysiology|pathophysiological]] state, but in practice few researchers and clinicians distinguish between the terms.<ref name="AndersonT"/> Descriptions of the condition, including the severity and the area of the brain affected, are now used more often than "concussion" in clinical neurology.<ref name="LarnerAJ">
| |
| {{
| |
| cite book |author=Larner AJ, Barker RJ, Scolding N, Rowe D |title=The A-Z of Neurological Practice: a Guide to Clinical Neurology |publisher=Cambridge University Press |location=Cambridge, UK |year=2005 |pages=199 |isbn=0521629608 |oclc= |doi=
| |
| }}</ref>
| |
|
| |
|
| Although the term "concussion" is still used in sports literature as interchangeable with "MHI" or "MTBI", the general clinical medical literature now uses "MTBI" instead.<ref name="BarthVarney99">
| | ==[[Concussion risk factors|Risk Factors]]== |
| {{
| |
| cite book |author=Barth JT, Varney NR, Ruchinskas RA, Francis JP |chapter=Mild head injury: The new frontier in sports medicine |editor=Varney NR, Roberts RJ |title=The Evaluation and Treatment of Mild Traumatic Brain Injury |publisher=Lawrence Erlbaum Associates |location=Hillsdale, New Jersey |year=1999 |pages=85-86 |isbn=0-8058-2394-8 |oclc= |doi= |accessdate=2008-03-06 |url= http://books.google.com/books?id=i4Tpx6wHvJ4C&pg=PA21&vq=concussion&source=gbs_search_s&sig=t8NaFBJM5afqp0fXKb3Ou8yBjMo#PPA357,M1
| |
| }}</ref>
| |
|
| |
|
| Controversy exists about whether the definition of concussion should include only those injuries in which [[unconsciousness|loss of consciousness]] occurs.<ref name="Pearce"/> Historically, concussion by definition involved a loss of consciousness, but the definition has changed over time to include a change in consciousness, such as amnesia.<ref name="RuffGrant">
| | ==[[Concussion natural history, complications and prognosis|Natural History, Complications and Prognosis]]== |
| {{
| |
| cite book |author=Ruff RM, Grant I |chapter=Postconcussional disorder: Background to DSM-IV and future considerations |editor=Varney NR, Roberts RJ |title=The Evaluation and Treatment of Mild Traumatic Brain Injury |publisher=Lawrence Erlbaum Associates |location=Hillsdale, New Jersey |year=1999 |pages=320 |isbn=0-8058-2394-8 |oclc= |doi= |url=http://books.google.com/books?id=i4Tpx6wHvJ4C&pg=PA21&vq=concussion&source=gbs_search_s&sig=t8NaFBJM5afqp0fXKb3Ou8yBjMo#PPA357,M1
| |
| }}</ref> The best-known concussion grading scales count head injuries in which loss of consciousness does not occur to be mild concussions and those in which it does to be more severe.<ref name=cobb/>
| |
|
| |
|
| ==Diagnosis== | | ==Diagnosis== |
| Diagnosis of MTBI is based on physical and neurological exams, duration of unconsciousness (usually less than 30 minutes) and post-traumatic amnesia (PTA; usually less than 24 hours), and the Glasgow Coma Scale (MTBI sufferers have scores of 13 to 15).<ref name="BorgHolm04"/> [[Neuropsychological test]]s exist to measure cognitive function.<ref name="Rees03"/> The tests may be administered hours, days, or weeks after the injury, or at different times to determine whether there is a trend in the patient's condition.<ref name=moser>
| | [[Concussion diagnostic criteria|Diagnostic Criteria]] | [[Concussion history and symptoms|History and Symptoms]] | [[Concussion physical examination|Physical Examination]] | [[Concussion CT|CT]] | [[Concussion MRI|MRI]] | [[Concussion other imaging findings|Other Imaging Findings]] | [[Concussion other diagnostic studies|Other Diagnostic Studies]] |
| {{
| |
| cite journal|author=Moser RS, Iverson GL, Echemendia RJ, Lovell MR, Schatz P, Webbe FM ''et al.'' |date=2007 |title=Neuropsychological evaluation in the diagnosis and management of sports-related concussion |journal=Archives of Clinical Neuropsychology |volume=22 |issue=8 |pages=909–916 |pmid=17988831
| |
| }}
| |
| </ref> Athletes may be tested before a sports season begins to provide a baseline comparison in the event of an injury.<ref name="pmid10981754">
| |
| {{
| |
| cite journal |author=Maroon JC, Lovell MR, Norwig J, Podell K, Powell JW, Hartl R |title=Cerebral concussion in athletes: Evaluation and neuropsychological testing |journal=Neurosurgery |volume=47 |issue=3 |pages=659–669; discussion 669–672 |year=2000 |pmid=10981754 |doi= |url=
| |
| }}
| |
| </ref>
| |
|
| |
|
| [[Image:Anizokoria.JPG|left|thumb|230px|Unequal pupil size is a sign of a brain injury more serious than concussion.]] | | ==Treatment== |
| Health care providers examine head trauma survivors to ensure that the injury is not a more severe [[medical emergency]] such as an intracranial hemorrhage. Indications that screening for more serious injury is needed include worsening of symptoms such as headache, persistent vomiting,<ref name="CookSchweer">
| | [[Concussion medical therapy|Medical Therapy]] | [[Concussion primary prevention|Primary Prevention]] | [[Concussion secondary prevention|Secondary Prevention]] | [[Concussion cost-effectiveness of therapy|Cost-Effectiveness of Therapy]] | [[Concussion future or investigational therapies|Future or Investigational Therapies]] |
| {{
| |
| cite journal |author=Cook RS, Schweer L, Shebesta KF, Hartjes K, Falcone RA |title=Mild traumatic brain injury in children: Just another bump on the head? |journal=Journal of Trauma Nursing |volume=13 |issue=2 |pages=58–65 |year=2006 |pmid=16884134 |doi=
| |
| }}
| |
| </ref> increasing disorientation or a deteriorating level of consciousness,<ref name="Kayteasdale">
| |
| {{
| |
| cite journal |author=Kay A, Teasdale G |title=Head injury in the United Kingdom |journal=World Journal of Surgery |volume=25 |issue=9 |pages=1210–1220 |year=2001 |pmid=11571960 |doi=10.1007/s00268-001-0084-6 |url=
| |
| }}
| |
| </ref> [[post-traumatic seizure|seizure]]s, and [[anisocoria|unequal pupil size]].<ref name="cdcfacts">
| |
| {{
| |
| cite web|publisher=Centers for Disease Control and Prevention |date=2006 |url=http://www.cdc.gov/ncipc/tbi/contents.htm |title=Facts About Concussion and Brain Injury |accessdate=2008-01-13
| |
| }}
| |
| </ref> Patients with such symptoms, or who are at higher risk for a more serious brain injury, are given [[Magnetic resonance imaging|MRI]]s or [[CT scan]]s to detect brain lesions and are observed by medical staff.
| |
|
| |
|
| Health care providers make the decision about whether to give a CT scan using the Glasgow Coma Scale.<ref name="pmid17215534">
| | ==Case Studies== |
| {{
| | [[Concussion case study one|Case #1]] |
| cite journal |author=Ropper AH, Gorson KC |title=Clinical practice. Concussion |journal=New England Journal of Medicine |volume=356 |issue=2 |pages=166–172 |year=2007|url=http://content.nejm.org/cgi/content/full/356/2/166 |pmid=17215534 |doi=10.1056/NEJMcp064645 |pmid=17215534
| |
| }}
| |
| </ref> In addition, they may be more likely to perform a CT scan on people who would be difficult to observe after discharge or those who are [[intoxication|intoxicated]], at risk for bleeding, older than 60,<ref name="pmid17215534"/> or younger than 16. Most concussions cannot be detected with MRI or CT scans.<ref name="Poirier">
| |
| {{
| |
| cite journal |author=Poirier MP |year=2003 |url= |title=Concussions: Assessment, management, and recommendations for return to activity ([http://www.sciencedirect.com/science?_ob=ArticleURL&_udi=B75BD-49H1C2F-7&_user=3356446&_origUdi=B6VDJ-44KHFBN-8&_fmt=high&_coverDate=09%2F30%2F2003&_rdoc=1&_orig=article&_acct=C000060332&_version=1&_urlVersion=0&_userid=3356446&md5=9c2a61c0c62684c26cf317a8ea637458 abstract]) |journal=Clinical Pediatric Emergency Medicine |volume=4 |issue=3 |pages=179–185 |doi=10.1016/S1522-8401(03)00061-2
| |
| }}
| |
| <!--abstract linked with url because doi doesn't take you right to it. no PMID found--></ref> However, changes have been reported to show up on MRI and SPECT imaging in concussed people with normal CT scans, and [[post-concussion syndrome]] may be associated with abnormalities visible on [[single photon emission computed tomography|SPECT]] and [[Positron emission tomography|PET scan]]s.<ref name="Iverson2005"/> Mild head injury may or may not produce abnormal [[Electroencephalography|EEG]] readings.<ref name="Binder86">
| |
| {{
| |
| cite journal |author=Binder LM |title=Persisting symptoms after mild head injury: A review of the postconcussive syndrome |journal=Journal of Clinical and Experimental Neuropsychology|volume=8 |issue=4 |pages=323–346 |year=1986 |pmid=3091631 |doi=10.1080/01688638608401325
| |
| }}
| |
| </ref>
| |
|
| |
|
| Concussion may be under-diagnosed. The lack of the highly noticeable signs and symptoms that are frequently present in other forms of head injury could lead [[clinician]]s to miss the injury, and athletes may cover up their injuries in order to be allowed to remain in the competition.<ref name="BarthVarney99"/> A retrospective survey in 2005 found that more than 88% of concussions go unrecognized.<ref name="Delaney">
| | ==Related Chapters== |
| {{
| | *[[Post-concussion syndrome]] |
| cite journal |author=Delaney JS, Abuzeyad F, Correa JA, Foxford R |title=Recognition and characteristics of concussions in the emergency department population |journal=Journal of Emergency Medicine |volume=29 |issue=2 |pages=189–197 |year=2005 |pmid=16029831 |doi=10.1016/j.jemermed.2005.01.020
| | *[[Second-impact syndrome]] |
| }}
| | *[[Dementia pugilistica]] |
| </ref>
| |
|
| |
|
| Diagnosis of concussion can be complicated because it shares symptoms with other conditions. For example, post-concussion symptoms such as cognitive problems may be misattributed to brain injury when they are in fact due to [[post-traumatic stress disorder]] (PTSD).<ref name="Bryant08"/>
| |
|
| |
|
| ==Prognosis and lasting effects==
| |
| MTBI has a mortality rate of almost zero.<ref name="BorgHolm04"/> The symptoms of most concussions resolve within weeks, but problems may persist.<ref name="AndersonT"/> It is not common for problems to be permanent, and outcome is usually excellent.<ref name="Iverson2005"/> People over age 55 may take longer to heal from MTBI or may heal incompletely.<ref name="AlexanderMP95">
| |
| {{
| |
| cite journal |author=Alexander MP |title=Mild traumatic brain injury: Pathophysiology, natural history, and clinical management |journal=Neurology |volume=45 |issue=7 |pages=1253–1260 |year=1995 |pmid=7617178 |doi=
| |
| }}
| |
| </ref> Similarly, factors such as a previous head injury or a coexisting medical condition have been found to predict longer-lasting post-concussion symptoms.<ref name="Hall05"/> Other factors that may lengthen recovery time after MTBI include psychological problems such as [[substance abuse]] or [[clinical depression]], poor health before the injury or additional injuries sustained during it, and life stress.<ref name="Iverson2005">
| |
| {{
| |
| cite journal |author=Iverson GL |title=Outcome from mild traumatic brain injury |journal=Current Opinion in Psychiatry |volume=18 |issue=3 |pages=301–317 |year=2005 |pmid=16639155 |doi=10.1097/01.yco.0000165601.29047.ae
| |
| }}
| |
| </ref> Longer periods of amnesia or loss of consciousness immediately after the injury may indicate longer recovery times from residual symptoms.<ref name="Masferrer"/> For unknown reasons, having had one concussion significantly increases a person's risk of having another.<ref name=moser/> The prognosis may differ between concussed adults and children.<ref name=moser/> Little research has been done on concussion in the [[pediatric]] population, but concern exists that severe concussions could interfere with [[neural development|brain development]] in children.<ref name=moser/>
| |
|
| |
| ===Post-concussion syndrome===
| |
| {{main|Post-concussion syndrome}}
| |
| In post-concussion syndrome, symptoms do not resolve for weeks, months, or years after a concussion, and may occasionally be permanent.<ref name="Ryan03">
| |
| {{
| |
| cite journal |author=Ryan LM, Warden DL |title=Post concussion syndrome |journal=International Review of Psychiatry |volume=15 |issue=4 |pages=310–316 |year=2003 |pmid=15276952 |doi=10.1080/09540260310001606692
| |
| }}
| |
| </ref> Symptoms may include headaches, dizziness, fatigue, [[anxiety]], memory and attention problems, sleep problems, and irritability.<ref name=Boake>
| |
| {{
| |
| cite journal |author=Boake C, McCauley SR, Levin HS, Pedroza C, Contant CF, Song JX, ''et al''. |date=2005 | url=http://neuro.psychiatryonline.org/cgi/content/full/17/3/350 |title=Diagnostic criteria for postconcussional syndrome after mild to moderate traumatic brain injury |journal=Journal of Neuropsychiatry and Clinical Neurosciences |volume=17 |issue=3 |pages=350-356 |pmid=16179657 |doi= doi: 10.1176/appi.neuropsych.17.3.350
| |
| }}
| |
| </ref> There is no scientifically established treatment, and rest, a recommended recovery technique, has limited effectiveness.<ref name="Willer06"/> Symptoms usually go away on their own within months.<ref name="ParikhKoch"/> The question of whether the syndrome is due to structural damage or other factors such as psychological ones, or a combination of these, has long been the subject of debate.<ref name="Bryant08">
| |
| {{
| |
| cite journal |author=Bryant RA |title=Disentangling mild traumatic brain injury and stress reactions |journal=New England Journal of Medicine |volume=358 |issue=5 |pages=525–527 |year=2008 |pmid=18234757 |doi=10.1056/NEJMe078235
| |
| }}
| |
| </ref>
| |
|
| |
| ===Cumulative effects===
| |
| Cumulative effects of concussions are poorly understood. The severity of concussions and their symptoms may worsen with successive injuries, even if a subsequent injury occurs months or years after an initial one.<ref name=harmon>
| |
| {{
| |
| cite journal|author=Harmon KG |year=1999 |url=http://www.aafp.org/afp/990901ap/887.html |title=Assessment and management of concussion in sports |journal=American Family Physician |volume=60 |issue=3 |pages=887–892, 894 |pmid=10498114
| |
| }}
| |
| </ref> Symptoms may be more severe and changes in [[neurophysiology]] can occur with the third and subsequent concussions.<ref name=moser/> Studies have had conflicting findings on whether athletes have longer recovery times after repeat concussions and whether cumulative effects such as impairment in cognition and memory occur.<ref name="Pellman">
| |
| {{
| |
| cite journal |author=Pellman EJ, Viano DC |title=Concussion in professional football: Summary of the research conducted by the National Football League’s Committee on Mild Traumatic Brain Injury|journal=Neurosurgical Focus |volume=21 |issue=4 |pages=E12 |year=2006 |pmid=17112190 |doi= |url=http://www.aans.org/education/journal/neurosurgical/Oct06/21-4-12-1028.pdf |format=PDF
| |
| }}
| |
| </ref>
| |
|
| |
| Cumulative effects may include [[mental disorder|psychiatric disorder]]s and loss of [[long-term memory]]. For example, the risk of developing clinical depression has been found to be significantly greater for retired football players with a history of three or more concussions than for those with no concussion history.<ref name="cantuCTE">
| |
| {{
| |
| cite journal |author=Cantu RC |title=Chronic traumatic encephalopathy in the National Football League |journal=Neurosurgery |volume=61 |issue=2 |pages=223–225 |year=2007 |pmid=17762733 |doi=10.1227/01.NEU.0000255514.73967.90
| |
| }}
| |
| </ref> Three or more concussions is also associated with a five-fold greater chance of developing [[Alzheimer's disease]] earlier and a three-fold greater chance of developing [[memory]] deficits.<ref name="cantuCTE"/>
| |
|
| |
| ==Dementia pugilistica==
| |
|
| |
| {{main|Dementia pugilistica}}
| |
| Chronic [[encephalopathy]] is an example of the cumulative damage that can occur as the result of multiple concussions or less severe blows to the head. The condition called [[dementia pugilistica]], or "punch drunk" syndrome, which is associated with boxers, can result in cognitive and physical deficits such as [[parkinsonism]], speech and memory problems, slowed mental processing, tremor, and inappropriate behavior.<ref name="Mendez">
| |
| {{
| |
| cite journal |author=Mendez MF |title=The neuropsychiatric aspects of boxing |journal=International Journal of Psychiatry in Medicine |volume=25 |issue=3 |pages=249–262 |year=1995 |pmid=8567192 |doi=
| |
| }}
| |
| </ref> It shares features with Alzheimer's disease.<ref name="Jordan00">
| |
| {{
| |
| cite journal |author=Jordan BD |title=Chronic traumatic brain injury associated with boxing |journal=Seminars in Neurology |volume=20 |issue=2 |pages=179–85 |year=2000 |pmid=10946737 |doi=10.1055/s-2000-9826
| |
| }}
| |
| </ref>
| |
|
| |
| ===Second-impact syndrome===
| |
| {{main|Second-impact syndrome}}
| |
| Second-impact syndrome, in which the brain swells dangerously after a minor blow, may occur in very rare cases. The condition may develop in people who receive a second blow days or weeks after an initial concussion, before its symptoms have gone away.<ref name="Bowen03"/> No one is certain of the cause of this often fatal complication, but it is commonly thought that the swelling occurs because the brain's [[arteriole]]s lose the ability to regulate their diameter, causing a loss of control over cerebral blood flow.<ref name=moser/> As the brain [[swelling|swells]], intracranial pressure rapidly rises.<ref name="CookSchweer"/> The brain can [[brain herniation|herniate]], and the brain stem can fail within five minutes.<ref name="Bowen03"/> Except in boxing, all cases have occurred in athletes under age 20.<ref name="Team"/> Due to the very small number of documented cases, the diagnosis is controversial, and doubt exists about its validity.<ref name=McCroryP01>
| |
| {{
| |
| cite journal|author=McCrory P |date=2001 |title=Does second impact syndrome exist? |journal=Clinical Journal of Sport Medicine |volume=11 |issue=3 |pages=144–149 |pmid=11495318
| |
| }}
| |
| </ref>
| |
|
| |
| == References ==
| |
| {{Reflist|2}}
| |
|
| |
|
| {{Injuries, other than fractures, dislocations, sprains and strains}} | | {{Injuries, other than fractures, dislocations, sprains and strains}} |