Concussion: Difference between revisions
| Line 12: | Line 12: | ||
==Diagnosis== | ==Diagnosis== | ||
Concussion may be under-diagnosed. The lack of the highly noticeable signs and symptoms that are frequently present in other forms of head injury could lead [[clinician]]s to miss the injury, and athletes may cover up their injuries in order to be allowed to remain in the competition.<ref name="BarthVarney99"/> A retrospective survey in 2005 found that more than 88% of concussions go unrecognized.<ref name="Delaney"> | Concussion may be under-diagnosed. The lack of the highly noticeable signs and symptoms that are frequently present in other forms of head injury could lead [[clinician]]s to miss the injury, and athletes may cover up their injuries in order to be allowed to remain in the competition.<ref name="BarthVarney99"/> A retrospective survey in 2005 found that more than 88% of concussions go unrecognized.<ref name="Delaney"> | ||
Revision as of 15:13, 27 February 2013
For patient information, click here
| Concussion | |
 | |
|---|---|
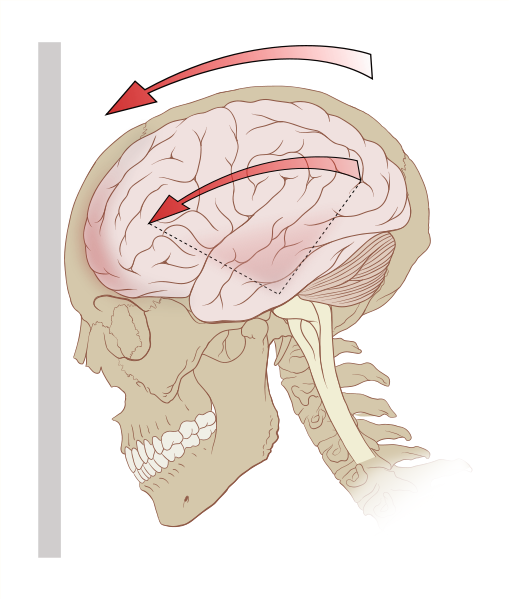
| Deceleration can exert rotational forces in the brain, especially the midbrain and diencephalon. |
Editor-In-Chief: C. Michael Gibson, M.S., M.D. [1]
|
Concussion Microchapters |
|
Diagnosis |
|---|
|
Treatment |
|
Case Studies |
|
Concussion On the Web |
|
American Roentgen Ray Society Images of Concussion |
Diagnosis
Concussion may be under-diagnosed. The lack of the highly noticeable signs and symptoms that are frequently present in other forms of head injury could lead clinicians to miss the injury, and athletes may cover up their injuries in order to be allowed to remain in the competition.[1] A retrospective survey in 2005 found that more than 88% of concussions go unrecognized.[2]
Dementia pugilistica
Chronic encephalopathy is an example of the cumulative damage that can occur as the result of multiple concussions or less severe blows to the head. The condition called dementia pugilistica, or "punch drunk" syndrome, which is associated with boxers, can result in cognitive and physical deficits such as parkinsonism, speech and memory problems, slowed mental processing, tremor, and inappropriate behavior.[3] It shares features with Alzheimer's disease.[4]
Second-impact syndrome
Second-impact syndrome, in which the brain swells dangerously after a minor blow, may occur in very rare cases. The condition may develop in people who receive a second blow days or weeks after an initial concussion, before its symptoms have gone away.[5] No one is certain of the cause of this often fatal complication, but it is commonly thought that the swelling occurs because the brain's arterioles lose the ability to regulate their diameter, causing a loss of control over cerebral blood flow.[6] As the brain swells, intracranial pressure rapidly rises.[7] The brain can herniate, and the brain stem can fail within five minutes.[5] Except in boxing, all cases have occurred in athletes under age 20.[8] Due to the very small number of documented cases, the diagnosis is controversial, and doubt exists about its validity.[9]
Related Chapters
References
- ↑
- ↑ Delaney JS, Abuzeyad F, Correa JA, Foxford R (2005). "Recognition and characteristics of concussions in the emergency department population". Journal of Emergency Medicine. 29 (2): 189–197. doi:10.1016/j.jemermed.2005.01.020. PMID 16029831.
- ↑ Mendez MF (1995). "The neuropsychiatric aspects of boxing". International Journal of Psychiatry in Medicine. 25 (3): 249–262. PMID 8567192.
- ↑ Jordan BD (2000). "Chronic traumatic brain injury associated with boxing". Seminars in Neurology. 20 (2): 179–85. doi:10.1055/s-2000-9826. PMID 10946737.
- ↑ 5.0 5.1
- ↑
- ↑
- ↑
- ↑ McCrory P (2001). "Does second impact syndrome exist?". Clinical Journal of Sport Medicine. 11 (3): 144–149. PMID 11495318.
Template:Injuries, other than fractures, dislocations, sprains and strains
da:Hjernerystelse
de:Gehirnerschütterung
el:Εγκεφαλική διάσειση
it:Commozione cerebrale
he:זעזוע מוח
nl:Hersenschudding
no:Hjernerystelse
fi:Aivotärähdys
sv:Hjärnskakning