Chronic cholecystitis: Difference between revisions
| Line 42: | Line 42: | ||
==Treatment== | ==Treatment== | ||
[[Cholecystitis medical therapy|Medical therapy]] | [[Cholecystitis surgery|Surgical options]] | [[Cholecystitis primary prevention|Primary prevention]] | [[Cholecystitis secondary prevention|Secondary prevention]] | [[Cholecystitis cost-effectiveness of therapy|Financial costs]] | [[Cholecystitis future or investigational therapies|Future therapies]] | [[Cholecystitis medical therapy|Medical therapy]] | [[Cholecystitis surgery|Surgical options]] | [[Cholecystitis primary prevention|Primary prevention]] | [[Cholecystitis secondary prevention|Secondary prevention]] | [[Cholecystitis cost-effectiveness of therapy|Financial costs]] | [[Cholecystitis future or investigational therapies|Future therapies]] | ||
== Differential Diagnosis of Causes of Cholecystitis by Presence of a Stone== | == Differential Diagnosis of Causes of Cholecystitis by Presence of a Stone== | ||
Revision as of 16:54, 27 January 2012
Template:DiseaseDisorder infobox
|
Chronic cholecystitis Microchapters |
|
Diagnosis |
|---|
|
Treatment |
|
Case Studies |
|
Chronic cholecystitis On the Web |
|
American Roentgen Ray Society Images of Chronic cholecystitis |
For patient information click here
Editor-In-Chief: C. Michael Gibson, M.S., M.D. [1]
Please Take Over This Page and Apply to be Editor-In-Chief for this topic: There can be one or more than one Editor-In-Chief. You may also apply to be an Associate Editor-In-Chief of one of the subtopics below. Please mail us [2] to indicate your interest in serving either as an Editor-In-Chief of the entire topic or as an Associate Editor-In-Chief for a subtopic. Please be sure to attach your CV and or biographical sketch.
Overview
Historical Perspective
Pathophysiology
Epidemiology & Demographics
Risk Factors
Screening
Causes
Differentiating Cholecystitis
Complications & Prognosis
Diagnosis
History and Symptoms | Physical Examination | Staging | Laboratory tests | Electrocardiogram | X Rays | CT | MRI Echocardiography or Ultrasound | Other images | Alternative diagnostics
Treatment
Medical therapy | Surgical options | Primary prevention | Secondary prevention | Financial costs | Future therapies
Differential Diagnosis of Causes of Cholecystitis by Presence of a Stone
Acalculous Cholecystitis
- AIDS with cryptosporidiosis
- AIDS with Cytomegalovirus
- AIDS with microsporidiosis
- Burns
- Diabetes Mellitus
- Idiopathic
- Long-term total parenteral nutrition (TPN)
- Major surgery
- Myocardial infarction
- Other cardiac disease
- Prolonged fasting
- Salmonella
- Sepsis
- Seriously ill patients
- Severe trauma
- Sickle Cell Disease
Calculous Cholecystitis (Cholelithiasis)
- Female gender
- Hormonal therapy in women
- Idiopathic
- Increasing age
- Obesity
- Pregnancy
- Race: Scandinavians > African-Americans
- Rapid weight loss
Investigations
Blood
Laboratory values may be notable for an elevated alkaline phosphatase, possibly an elevated bilirubin (although this may indicate choledocholithiasis), and possibly an elevation of the WBC. CRP (C-reactive protein) is often elevated. The degree of elevation of these laboratory values may depend on the degree of inflammation of the gallbladder. Patients with acute cholecystitis are much more likely to manifest abnormal laboratory values, while in chronic cholecystitis the laboratory values are frequently normal.
Radiology
Sonography is a sensitive and specific modality for diagnosis of acute cholecystitis; adjusted sensitivity and specificity for diagnosis of acute cholecystitis are 88% and 80%, respectively. The 2 major diagnostic criteria are cholelithiasis and sonographic Murphy's sign. Minor criteria include gallbladder wall thickening greater than 3mm, pericholecystic fluid, and gallbladder dilatation. [1] [2]
The reported sensitivity and specificity of CT scan findings are in the range of 90-95%. CT is more sensitive than ultrasonography in the depiction of pericholecystic inflammatory response and in localizing pericholecystic abscesses, pericholecystic gas, and calculi outside the lumen of the gallbladder. CT cannot see noncalcified gallbladder calculi, and cannot assess for a Murphy's sign. [1] [2]
Hepatobiliary scintigraphy with technetium-99m DISIDA (bilirubin) analog is also sensitive and accurate for diagnosis of chronic and acute cholecystitis. It can also assess the ability of the gall bladder to expel bile (gall bladder ejection fraction), and low gall bladder ejection fraction has been linked to chronic cholecystitis. However, since most patients with right upper quadrant pain do not have cholecystitis, primary evaluation is usually accomplished with a modality that can diagnose other causes, as well. [1] [2]
Therapy
For most patients, in most centres, the definitive treatment is surgical removal of the gallbladder. Supportive measures are instituted in the meantime and to prepare the patient for surgery. These measures include fluid resuscitation and antibiotics. Antibiotic regimens usually consist of a broad spectrum cephalosporin such as ceftriaxone and an antibacterial with good cover against anaerobic bacteria, such as metronidazole.
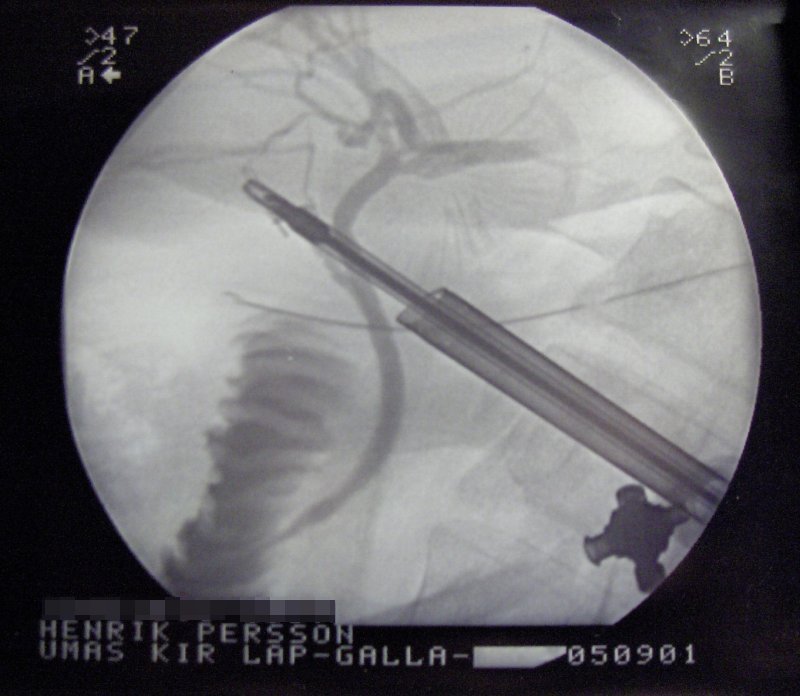
Gallbladder removal, cholecystectomy, can be accomplished via open surgery or a laparoscopic procedure. Laparoscopic procedures can have less morbidity and a shorter recovery stay. Open procedures are usually done if complications have developed or the patient has had prior surgery to the area, making laparoscopic surgery technically difficult. A laparoscopic procedure may also be 'converted' to an open procedure during the operation if the surgeon feels that further attempts at laparoscopic removal might harm the patient. Open procedure may also be done if the surgeon does not know how to perform a laparoscopic cholesystectomy.
In cases of severe inflammation, shock, or if the patient has higher risk for general anesthesia (required for cholecystectomy), the managing physician may elect to have an interventional radiologist insert a percutaneous drainage catheter into the gallbladder ('percutaneous cholecystostomy tube') and treat the patient with antibiotics until the acute inflammation resolves. The patient may later warrant cholecystectomy if their condition improves.
Complications of cholecystitis
Complications of cholecystectomy
- bile leak ("biloma")
- bile duct injury (about 5-7 out of 1000 operations. Open and laparoscopic surgeries have essentially equal injuries, but the recent trend is towards fewer injuries with laparoscopy, probably because the open cases often result because the gallbladder is too difficult or risky to remove with laparoscopy)
- abscess
- wound infection
- bleeding (liver surface and cystic artery most common sites)
- hernia
- organ injury (intestine and liver at highest risk, especially if gallbladder through inflammation has become adherent/scarred to other organs (e.g. transverse colon)
- deep vein thrombosis/pulmonary embolism (unusual- risk can be decreased through use of sequential compression devices on legs during surgery)
Gall bladder perforation
Gall bladder perforation (GBP) is a rare but life-threatening complication of acute cholecystitis. The early diagnosis and treatment of GBP are crucial to patient morbidity and mortality. [3]
Approaches to this complication will vary based on the condition of an individual patient, the evaluation of the treating surgeon or physician, and the facilities' capability. It can happen at the neck from pressure necrosis of an impacted calculus, or at the fundus. It can result in a local abscess, or perforation into the general peritoneal cavity; if the bile, is infected diffuse peritonitis supervenes readily and rapidly. Death can result. [3]
A retrospective study looked at 332 patients who received medical and/or surgical treatment with the diagnosis of acute cholecystitis. Patients were treated with analgesics and antibiotics within the first 36 hours after admission (with a mean of 9 hours), and proceeded to surgery for a cholecystectomy. Two patients died and 6 patients had further complications. The morbidity and mortality rates were 37.5% and 12.5%, respectively in the present study. The authors of this study suggests that early diagnosis and emergency surgical treatment of gallbladder perforation are of crucial importance.[3]
Histopathological Findings: Chronic Cholecystitis
<youtube v=gxGvP3GV_1E/>
See also
References
- ↑ 1.0 1.1 1.2 Shea, JA, Berlin, JA, Escarce, JJ, et al. Revised estimates of diagnostic test sensitivity and specificity in suspected biliary tract disease. Arch Intern Med 1994; 154:2573.
- ↑ 2.0 2.1 2.2 Fink-Bennett, D, Freitas, JE, Ripley, SD, Bree, RL. The sensitivity of hepatobiliary imaging and real time ultrasonography in the detection of acute cholecystitis. Arch Surg 1985; 120:904.
- ↑ 3.0 3.1 3.2 Derici H, Kara C, Bozdag AD, Nazli O, Tansug T, Akca E (2006). "Diagnosis and treatment of gallbladder perforation". World J. Gastroenterol. 12 (48): 7832–6. PMID 17203529.
bs:Holecistitis de:Cholezystitis hr:Kolecistitis it:Colecistite sv:Gallblåseinflammation