Chickenpox epidemiology and demographics: Difference between revisions
| Line 11: | Line 11: | ||
===Prevalence=== | ===Prevalence=== | ||
*In the early 1990s, an average of 4 million people got varicella, 10,500 to 13,000 were hospitalized (range, 8,000 to 18,000), and 100 to 150 died each year. In the 1990s, the highest rate of varicella was reported in preschool-aged children. | *In the early 1990s, an average of 4 million people got varicella, 10,500 to 13,000 were hospitalized (range, 8,000 to 18,000), and 100 to 150 died each year. In the 1990s, the highest rate of varicella was reported in preschool-aged children. <ref name="urlChickenpox | Monitoring Vaccine Impact | Varicella | CDC">{{cite web |url=https://www.cdc.gov/chickenpox/surveillance/monitoring-varicella.html |title=Chickenpox | Monitoring Vaccine Impact | Varicella | CDC |format= |work= |accessdate=}}</ref> | ||
*Chickenpox vaccine became available in the United States in 1995. In 2014, 91% of children 19 to 35 months old in the United States had received one dose of varicella vaccine, varying from 83% to 95% by state. Among adolescents 13 to 17 years of age without a prior history of disease, 95% had received 1 dose of varicella vaccine, and 81% had received 2 doses of the vaccine. Eighty-five percent of adolescents had either a history of varicella disease or received 2 doses of varicella vaccine. | *Chickenpox vaccine became available in the United States in 1995. In 2014, 91% of children 19 to 35 months old in the United States had received one dose of varicella vaccine, varying from 83% to 95% by state. Among adolescents 13 to 17 years of age without a prior history of disease, 95% had received 1 dose of varicella vaccine, and 81% had received 2 doses of the vaccine. Eighty-five percent of adolescents had either a history of varicella disease or received 2 doses of varicella vaccine. | ||
Revision as of 15:47, 28 June 2017
Editor-In-Chief: C. Michael Gibson, M.S., M.D. [1] Associate Editor(s)-in-Chief:
|
Chickenpox Microchapters |
|
Diagnosis |
|---|
|
Treatment |
|
Case Studies |
|
Chickenpox epidemiology and demographics On the Web |
|
American Roentgen Ray Society Images of Chickenpox epidemiology and demographics |
|
Risk calculators and risk factors for Chickenpox epidemiology and demographics |
Overview
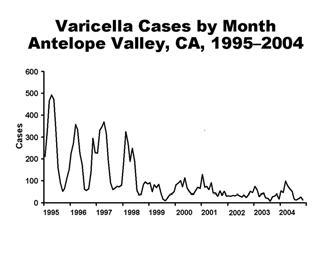
Varicella is an endemic disease spread mainly by the respiratory route. Cases are observed all through the year but most in the winter and early spring. In tropical regions, cases of varicella infection have been reported to be more commonly among adults than children.
Epidemiology and Demographics
Prevalence
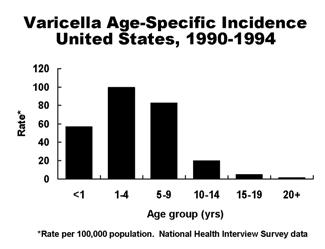
- In the early 1990s, an average of 4 million people got varicella, 10,500 to 13,000 were hospitalized (range, 8,000 to 18,000), and 100 to 150 died each year. In the 1990s, the highest rate of varicella was reported in preschool-aged children. [1]
- Chickenpox vaccine became available in the United States in 1995. In 2014, 91% of children 19 to 35 months old in the United States had received one dose of varicella vaccine, varying from 83% to 95% by state. Among adolescents 13 to 17 years of age without a prior history of disease, 95% had received 1 dose of varicella vaccine, and 81% had received 2 doses of the vaccine. Eighty-five percent of adolescents had either a history of varicella disease or received 2 doses of varicella vaccine.
- Since the chickenpox vaccine was developed in 1995, the major data of chickenpox in the environment is before 1995. In the prevaccine era, varicella was endemic in the United States, and virtually all persons acquired varicella by adulthood. As a result, the number of cases occurring annually was estimated to approximate the birth cohort, or approximately 4 million per year. Varicella was removed from the list of nationally notifiable conditions in 1981, but some states continued to report cases to CDC. The majority of cases (approximately 85%) occurred among children younger than 15 years of age.
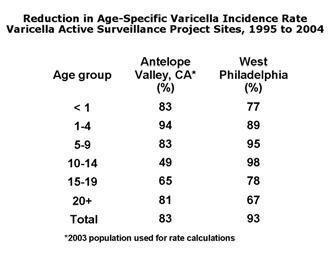
- In 2004, varicella vaccination coverage among children 19–35 months in two of the active surveillance areas was estimated to be 89% and 90%. Compared with 1995, varicella cases declined 83%–93% by 2004. Cases declined most among children aged 1–4 and 5–9 years, but a decline occurred in all age groups including infants and adults, indicating reduced transmission of the virus in 308 Varicella 21 these groups. The reduction of varicella cases is the result of the increasing use of varicella vaccine. Varicella vaccine coverage among 19–35-month-old children was estimated by the National Immunization Survey to be 90% in 2007.
- Despite high one-dose vaccination coverage and success of the vaccination program in reducing varicella morbidity and mortality, varicella surveillance indicates that the number of reported varicella cases appears to have plateaued. An increasing proportion of cases represent breakthrough infection (chickenpox occurring in a previously vaccinated person). In 2001–2005, outbreaks were reported in schools with high varicella vaccination coverage (96%–100%). These outbreaks had many similarities: all occurred in elementary schools; vaccine effectiveness was within the expected range (72%–85%); the highest attack rates occurred among the younger students; each outbreak lasted about 2 months; and persons with breakthrough infection transmitted the virus although the breakthrough disease was mild.Overall attack rates among vaccinated children were 11%–17%, with attack rates in some classrooms as high as 40%. These data indicate that even in settings where almost everyone was vaccinated and vaccine performed as expected, varicella outbreaks could not be prevented with the current one-dose vaccination policy.
- These observations led to the recommendation in 2006 for a second routine dose of varicella vaccine. Chickenpox used to be very common in the United States. In the early 1990s, an average of 4 million people got varicella, 10,500 to 13,000 were hospitalized (range, 8,000 to 18,000), and 100 to 150 died each year. In the 1990s, the highest rate of varicella was reported in preschool-aged children.
- Chickenpox vaccine became available in the United States in 1995. In 2014, 91% of children 19 to 35 months old in the United States had received one dose of varicella vaccine, varying from 83% to 95% by state. Among adolescents 13 to 17 years of age without a prior history of disease, 95% had received 1 dose of varicella vaccine, and 81% had received 2 doses of the vaccine. Eighty-five percent of adolescents had either a history of varicella disease or received 2 doses of varicella vaccine. Each year, more than 3.5 million cases of varicella, 9,000 hospitalizations, and 100 deaths are prevented by varicella vaccination in the United States.
- Each year, more than 3.5 million cases of varicella, 9,000 hospitalizations, and 100 deaths are prevented by varicella vaccination in the United States.
Incidence
- In the United States according to the 2012 survey, varicella incidence declined by 79% during 2000-2010 in 31 states and the incidence declined 72% during 2006-2010, after a routine second dose of varicella vaccination was administered. Varicella incidence from 2 active surveillance sites declined 98% during 1995-2010. [1]
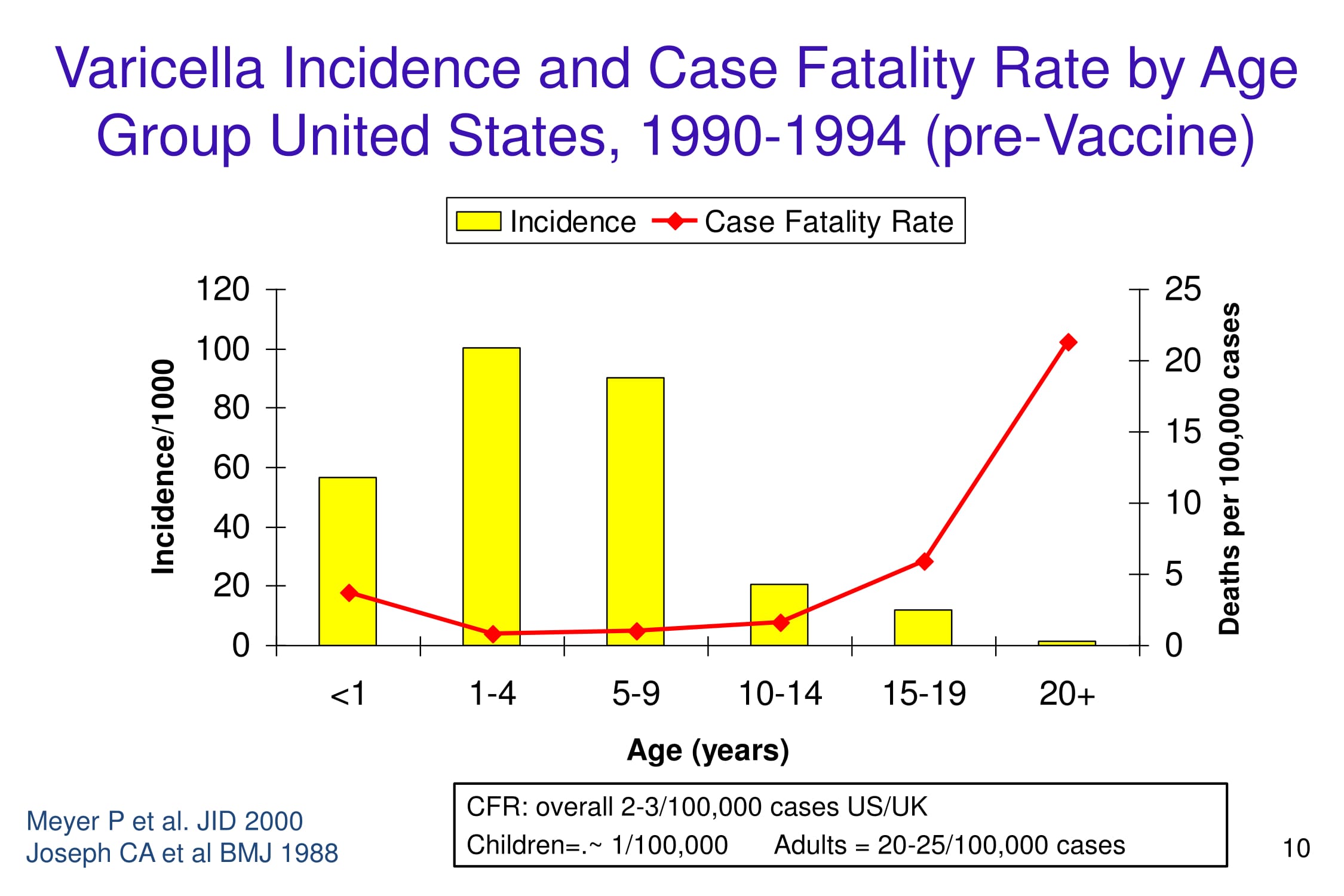
Case Fatality Rate
- In 1990-1994, case fatality rate is 2-3/100,000 cases in the US/UK among which children's cases were 1/100,000 and adults cases were 20-25/100,000 cases. [2]
Age
- Varicella being one of the classical diseases of childhood, has a highest prevalence occurring in the age groups of less than 10 years old.
- The highest age-specific incidence of varicella was among children 1–4 years of age, who accounted for 39% of all cases. This age distribution was probably a result of earlier exposure to VZV in preschool and child care settings. Children 5–9 years of age accounted for 38% of cases. Adults 20 years of age and older accounted for only 7% of cases (National Health Interview Survey data, 1990–1994). Data from three active varicella surveillance areas indicate that the incidence of varicella, as well as varicella-related hospitalizations, has decreased significantly since licensure of vaccine in 1995.
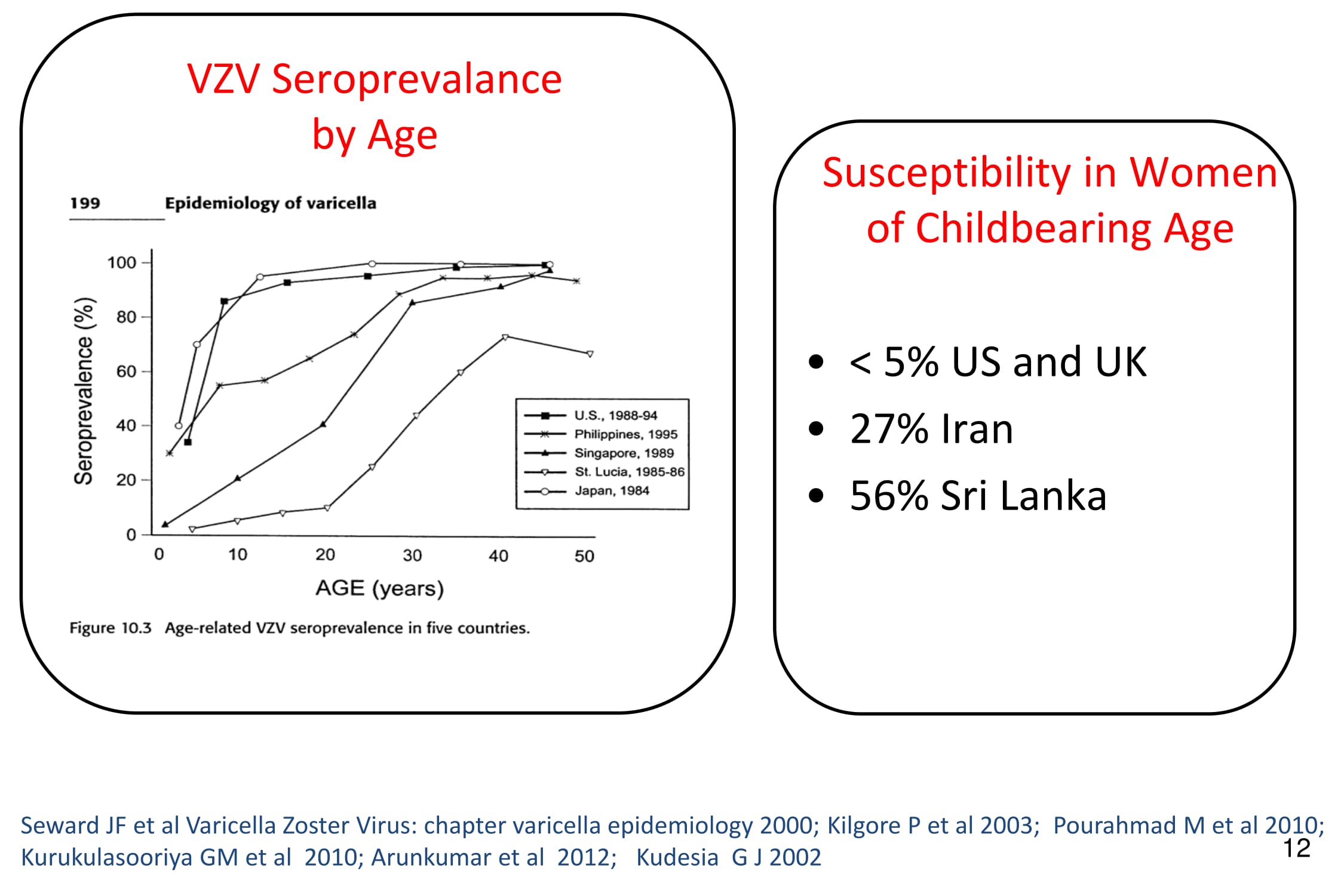
- It is highly communicable, with an attack rate of 90% in close contacts. Occurs mostly before adulthood but 10% of young adults remain susceptible. This pattern varies by regions, eg. in rural India, varicella is predominantly a disease of adults with the mean age of infection being 23.4 years which could be due to the interference by other respiratory viruses that the children are exposed to at an early age.[3]
- From generations, varicella has been a disease predominantly affecting the preschool and school-aged children. In tropical regions, the disease noticed among adults has the characteristics of the pocks being darker and the scars being more prominent than their younger counterparts.[3]
- In the U.S., 55% of chickenpox deaths are in the over-20 age group, even though they are a tiny fraction of the cases.
Gender
- The prevalence and incidence of chickenpox does not vary by gender. Gender differences in the incidence of chickenpox were observed in the 15-24 years age group females who are affected more comparatively. [4]
Race
- There is no racial predilection for chickenpox.
Developed Countries
The epidemiology and demographics of chickenpox in the developed countries are as follows:[2]
- Incidence
- 15.0 – 16.0/1,000 persons per year
- Highest incidence < 10 years
- Complications
- 2-4% of cases
- Hospitalizations
- 3-6 hospitalizations per 1,000 cases
- Congenital varicella syndrome
- Risk = 1-2% for pregnancies affected 0-20 weeks
- Deaths
- 3 deaths per 100,000 cases
- Most deaths occur in healthy people
Developing Countries
- Guinea Bissau 2000 (small study 2 deaths/1539 cases –6 months and 17 years) approximately 129/100,000 case, 50 times higher than US/UK.
- India late 1970s enhanced rash illness surveillance post smallpox eradication 433 deaths/862,155 reported cases; 80% deaths adults 52/100,000 cases, 20 times higher than US/UK
- Brazil 2008: estimated case fatality rate is 4/100,000. (deaths from vital statistics, cases from modeling). [2]
Deaths in hospital admissions.
- Nigeria (1970s): 14 deaths among 2,153 hospital admissions.
- Sri Lanka (2000-2001): 41 deaths among 989 varicella admissions (4.2%).
- Papua New Guinea (1980s): 10 deaths in adults at small hospital over 2 years in population 130,000.[2]
Gallery
-
-
-
-
-
-
Varicella cases and states reporting, United States, 1972-1996. From Public Health Image Library (PHIL). [5]
References
- ↑ 1.0 1.1 "Chickenpox | Monitoring Vaccine Impact | Varicella | CDC".
- ↑ 2.0 2.1 2.2 2.3 "www.who.int" (PDF).
- ↑ 3.0 3.1 "Epidemiology of Varicella Zoster Virus Infection, Epidemiology of VZV Infection, Epidemiology of Chicken Pox, Epidemiology of Shingles". Retrieved 2008-04-22.
- ↑ Fleming DM, Cross KW, Cobb WA, Chapman RS (2004). "Gender difference in the incidence of shingles". Epidemiol. Infect. 132 (1): 1–5. PMC 2870070. PMID 14979582.
- ↑ "Public Health Image Library (PHIL)".
![Varicella cases and states reporting, United States, 1972-1996. From Public Health Image Library (PHIL). [5]](/images/2/26/Chickenpox40.jpeg)