Central pontine myelinolysis: Difference between revisions
No edit summary |
No edit summary |
||
| Line 18: | Line 18: | ||
{{SK}} CPM; osmotic demyelination syndrome; osmotic myelinolysis; central pontine myelinosis | {{SK}} CPM; osmotic demyelination syndrome; osmotic myelinolysis; central pontine myelinosis | ||
== | ==[[Central pontine myelinolysis overview|Overview]]== | ||
== | ==[[Central pontine myelinolysis historical perspective|Historical Perspective]]== | ||
== | ==[[Central pontine myelinolysis pathophysiology|Pathophysiology]]== | ||
== | ==[[Central pontine myelinolysis causes|Causes]]== | ||
== | ==[[Central pontine myelinolysis differential diagnosis|Differentiating Central pontine myelinolysis from other Diseases]]== | ||
== | ==[[Central pontine myelinolysis epidemiology and demographics|Epidemiology and Demographics]]== | ||
== | ==[[Central pontine myelinolysis risk factors|Risk Factors]]== | ||
== | ==[[Central pontine myelinolysis natural history, complications and prognosis|Natural History, Complications and Prognosis]]== | ||
==Diagnosis== | |||
[[Central pontine myelinolysis history and symptoms|History and Symptoms]] | [[Central pontine myelinolysis physical examination|Physical Examination]] | [[Central pontine myelinolysis laboratory findings|Laboratory Findings]] | [[Central pontine myelinolysis CT|CT]] | [[Central pontine myelinolysis MRI|MRI]] | [[Central pontine myelinolysis echocardiography or ultrasound|Echocardiography or Ultrasound]] | [[Central pontine myelinolysis other imaging findings|Other Imaging Findings]] | [[Central pontine myelinolysis other diagnostic studies|Other Diagnostic Studies]] | |||
==Treatment== | ==Treatment== | ||
[[Central pontine myelinolysis medical therapy|Medical Therapy]] | [[Central pontine myelinolysis prevention|Prevention]] | [[Central pontine myelinolysis cost-effectiveness of therapy|Cost-Effectiveness of Therapy]] | [[Central pontine myelinolysis future or investigational therapies|Future or Investigational Therapies]] | |||
==Case Studies== | |||
[[Central pontine myelinolysis case study one|Case #1]] | |||
{{Diseases of the nervous system}} | {{Diseases of the nervous system}} | ||
Revision as of 13:47, 28 September 2012
| Central pontine myelinolysis | |
 | |
|---|---|
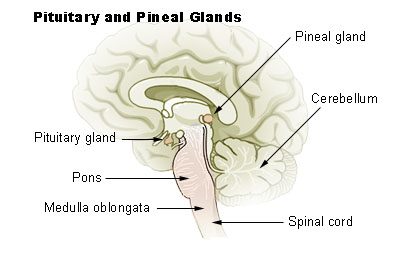
| Pons labeled at bottom left | |
| ICD-10 | G37.2 |
| DiseasesDB | 2198 |
| MedlinePlus | 000775 |
| MeSH | D017590 |
For patient information, click here
|
Central pontine myelinolysis Microchapters |
|
Differentiating Central pontine myelinolysis from other Diseases |
|---|
|
Diagnosis |
|
Treatment |
|
Case Studies |
|
Central pontine myelinolysis On the Web |
|
American Roentgen Ray Society Images of Central pontine myelinolysis |
|
Risk calculators and risk factors for Central pontine myelinolysis |
Editor-In-Chief: C. Michael Gibson, M.S., M.D. [1]
Synonyms and keywords: CPM; osmotic demyelination syndrome; osmotic myelinolysis; central pontine myelinosis
Overview
Historical Perspective
Pathophysiology
Causes
Differentiating Central pontine myelinolysis from other Diseases
Epidemiology and Demographics
Risk Factors
Natural History, Complications and Prognosis
Diagnosis
History and Symptoms | Physical Examination | Laboratory Findings | CT | MRI | Echocardiography or Ultrasound | Other Imaging Findings | Other Diagnostic Studies
Treatment
Medical Therapy | Prevention | Cost-Effectiveness of Therapy | Future or Investigational Therapies
Case Studies
Template:Diseases of the nervous system
de:Zentrale pontine Myelinolyse