Cavernous angioma
Template:DiseaseDisorder infobox
|
Cavernous angioma Microchapters |
|
Diagnosis |
|---|
|
Treatment |
|
Case Studies |
|
Cavernous angioma On the Web |
|
American Roentgen Ray Society Images of Cavernous angioma |
Editor-In-Chief: C. Michael Gibson, M.S., M.D. [1]
Synonyms and keywords: Cerebral cavernous malformation; CCM; cavernous hemangioma, cavernous haemangioma; cavernoma
CCMs & venous angiomas
In up to 30% there is a coincidence of CCM with a venous angioma, also known as a developmental venous anomaly (DVA). These lesions appear either as enhancing linear blood vessels or caput medusae, a radial orientation of small vessels that resemble the hair of Medusa from Greek mythology. These lesions are thought to represent developmental anomalies of normal venous drainage. These lesions should not be removed, as reports of venous infarcts have been reported. When found in association with a CCM that needs resection, great care should be taken not to disrupt the angioma.
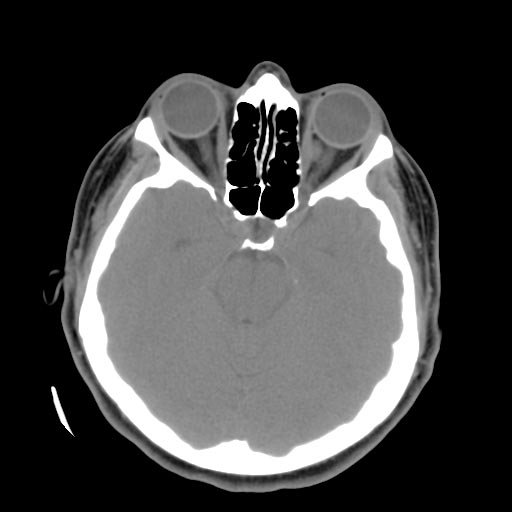
Left orbital cavernous hemangioma
Familial forms
Familial forms of CCM occur at three known genetic loci. The gene for CCM1 encodes KRIT1 (krev interaction trapped 1) and has been found to bind to ICAP1alpha (integrin cytoplasmic domain associated protein alpha), a beta1 integrin associated protein. The gene for CCM2 encodes a novel protein named "malcavernin" that contains a phosphotyrosine (PTB) binding domain. The exact biological function of CCM2 is not clear. Recently, it has been shown that CCM1 and CCM2 proteins as well as ICAP1alpha form a macromolecular complex in the cell. In addition, it appears that CCM2 protein may function as a scaffolding protein for MAP kinases that are essential in p38 activation responding to osmotic stress including MEKK3 and MKK3. It also binds to Rac and actin. Therefore, CCM2 protein is also called OSM (osmosensing scaffold for MEKK3). The CCM3 gene was the most recent CCM gene identified. CCM3 was known as PDCD10 (programmed cell death 10), which was initially identified as a gene that is up-regulated during the induction of apoptosis (cell death) in TF-1, a human myeloid cell line. The precise role of the PDCD10 protein in the CCM pathway that has been established to this point has not yet been determined. Research is ongoing to determine the function and properties of all three CCM gene products as well as the reaction pathways in which they are involved.
Mutations in these three genes account for 70 to 80 percent of all cases of cerebral cavernous malformations. The remaining 20 to 30 percent of cases may be due to other, still unidentified, genes.