Brain tumor: Difference between revisions
No edit summary |
m (Bot: Removing from Primary care) |
||
| (13 intermediate revisions by one other user not shown) | |||
| Line 2: | Line 2: | ||
{{Infobox_Disease | {{Infobox_Disease | ||
| Name = Brain tumor | | Name = Brain tumor | ||
| Image = | | Image = Hirnmetastase_MRT-T1_KM.jpg | ||
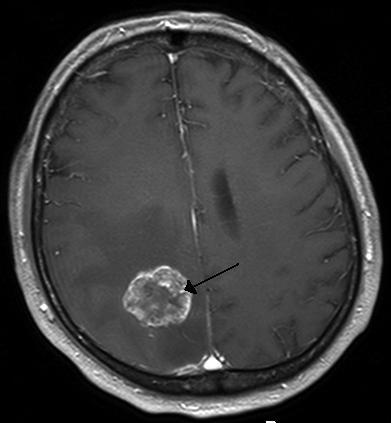
| Caption = [[Computed tomography|CT scan]] of brain showing brain cancer to left [[parietal lobe]] in the [[ventricular system|peri-ventricular]] area. | | Caption = [[Computed tomography|CT scan]] of brain showing brain cancer to left [[parietal lobe]] in the [[ventricular system|peri-ventricular]] area.https://en.wikipedia.org/wiki/File:Hirnmetastase_MRT-T1_KM.jpg | ||
}} | }} | ||
{{Brain tumor}} | {{Brain tumor}} | ||
| Line 15: | Line 15: | ||
==[[Brain tumor classification|Classification]]== | ==[[Brain tumor classification|Classification]]== | ||
Brain tumors can be classified as follows: | |||
{{Family tree/start}} | |||
{{Family tree | | | | | | | | | | | | A01 | | | | | | | | | | | | A01=Brain tumors}} | |||
{{Family tree | | | | | | |,|-|-|-|-|-|+|-|-|-|-|-|.| | | | | | | }} | |||
{{Family tree | | | | | | B01 | | | | B02 | | | | B03 | | | | | | B01=Adult primary brain tumor|B02=Childhood primary brain tumor|B03=Brain metastase}} | |||
{{Family tree | | | | | | |!| | | | | |!| | | | | |!| | | | | | | }} | |||
{{Family tree |boxstyle=text-align: left; | | | | | C01 | | | | C02 | | | | | C03 | | | | | | C01=<br>•Glioblastoma multiforme<br>•Oligodendroglioma<br>•Meningioma<br>•Hemangioblastoma<br>•Pituitary adenoma<br>•Schwannoma<br>•Primary CNS lymphoma|C02=<br>•Pilocytic astrocytoma<br>•Medulloblastoma<br>•Ependymoma<br>•Craniopharyngioma<br>•Pinealoma|C03=<br>•Lung cancer<br>•Breast cancer<br>•Melanoma<br>•Gastrointestinal tract cancer<br>•Renal cell carcinoma<br>•Osteosarcoma<br>•Head and neck cancer<br>•Neuroblastoma<br>•Lymphoma<br>•Prostate cancer}} | |||
{{Family tree | | | | | | | | | | | | | | | | | | | | | | | | | | }} | |||
{{Family tree | | | | | | | | | | | | | | | | | | | | | | | | | | }} | |||
{{Family tree | | | | | | | | | | | | | | | | | | | | | | | | | | }} | |||
{{Family tree | | | | | | | | | | | | | | | | | | | | | | | | | | }} | |||
{{Family tree | | | | | | | | | | | | | | | | | | | | | | | | | | }} | |||
{{Family tree | | | | | | | | | | | | | | | | | | | | | | | | | | }} | |||
{{Family tree/end}} | |||
<br /> | |||
==[[Brain tumor causes|Causes]]== | ==[[Brain tumor causes|Causes]]== | ||
The exact cause of brain tumor is not known. | |||
==[[Brain tumor differential diagnosis|Differentiating Brain Tumor from other Diseases]]== | ==[[Brain tumor differential diagnosis|Differentiating Brain Tumor from other Diseases]]== | ||
On the basis of [[seizure]], [[visual disturbance]], and constitutional symptoms, | On the basis of [[seizure]], [[visual disturbance]], and constitutional symptoms, brain tumors must be differentiated from [[Arteriovenous malformation|AV malformation]], [[brain aneurysm]], [[bacterial]] [[brain]] [[abscess]], [[tuberculosis]], [[toxoplasmosis]], [[hydatid cyst]], [[CNS]] [[cryptococcosis]], [[CNS]] [[aspergillosis]], and [[brain metastasis]]. | ||
{| | {| | ||
|- style="background: #4479BA; color: #FFFFFF; text-align: center;" | |- style="background: #4479BA; color: #FFFFFF; text-align: center;" | ||
| Line 43: | Line 59: | ||
! colspan="11" style="background: #7d7d7d; color: #FFFFFF; padding: 5px; text-align: center;" |Adult primary brain tumors | ! colspan="11" style="background: #7d7d7d; color: #FFFFFF; padding: 5px; text-align: center;" |Adult primary brain tumors | ||
|- | |- | ||
| style="background: #DCDCDC; padding: 5px; text-align: center;" |[[Glioblastoma multiforme]]<br | | style="background: #DCDCDC; padding: 5px; text-align: center;" |[[Glioblastoma multiforme]]<br> | ||
| style="background: #F5F5F5; padding: 5px; text-align: center;" | + | | style="background: #F5F5F5; padding: 5px; text-align: center;" | + | ||
| style="background: #F5F5F5; padding: 5px; text-align: center;" | +/− | | style="background: #F5F5F5; padding: 5px; text-align: center;" | +/− | ||
| Line 77: | Line 93: | ||
* Most of the time, focal [[neurological]] deficit is the presenting [[Sign (medical)|sign]]. | * Most of the time, focal [[neurological]] deficit is the presenting [[Sign (medical)|sign]]. | ||
|- | |- | ||
| style="background: #DCDCDC; padding: 5px; text-align: center;" |[[Oligodendroglioma]]<br | | style="background: #DCDCDC; padding: 5px; text-align: center;" |[[Oligodendroglioma]]<br> | ||
| style="background: #F5F5F5; padding: 5px; text-align: center;" | + | | style="background: #F5F5F5; padding: 5px; text-align: center;" | + | ||
| style="background: #F5F5F5; padding: 5px; text-align: center;" | + | | style="background: #F5F5F5; padding: 5px; text-align: center;" | + | ||
| Line 104: | Line 120: | ||
* Most of the time, [[epileptic seizure]] is the presenting [[Sign (medicine)|sign]]. | * Most of the time, [[epileptic seizure]] is the presenting [[Sign (medicine)|sign]]. | ||
|- | |- | ||
| style="background: #DCDCDC; padding: 5px; text-align: center;" |[[Meningioma]]<br | | style="background: #DCDCDC; padding: 5px; text-align: center;" |[[Meningioma]]<br> | ||
| style="background: #F5F5F5; padding: 5px; text-align: center;" | + | | style="background: #F5F5F5; padding: 5px; text-align: center;" | + | ||
| style="background: #F5F5F5; padding: 5px; text-align: center;" | +/− | | style="background: #F5F5F5; padding: 5px; text-align: center;" | +/− | ||
| Line 132: | Line 148: | ||
* May be associated with [[Neurofibromatosis type II|NF-2]] | * May be associated with [[Neurofibromatosis type II|NF-2]] | ||
|- | |- | ||
| style="background: #DCDCDC; padding: 5px; text-align: center;" |[[Hemangioblastoma]]<br | | style="background: #DCDCDC; padding: 5px; text-align: center;" |[[Hemangioblastoma]]<br> | ||
| style="background: #F5F5F5; padding: 5px; text-align: center;" | + | | style="background: #F5F5F5; padding: 5px; text-align: center;" | + | ||
| style="background: #F5F5F5; padding: 5px; text-align: center;" | +/− | | style="background: #F5F5F5; padding: 5px; text-align: center;" | +/− | ||
| Line 153: | Line 169: | ||
* May be associated with [[Von Hippel-Lindau Disease|von hippel-lindau syndrome]] | * May be associated with [[Von Hippel-Lindau Disease|von hippel-lindau syndrome]] | ||
|- | |- | ||
| style="background: #DCDCDC; padding: 5px; text-align: center;" |[[Pituitary adenoma]]<br | | style="background: #DCDCDC; padding: 5px; text-align: center;" |[[Pituitary adenoma]]<br><ref name=":0" /> | ||
| style="background: #F5F5F5; padding: 5px; text-align: center;" | − | | style="background: #F5F5F5; padding: 5px; text-align: center;" | − | ||
| style="background: #F5F5F5; padding: 5px; text-align: center;" | − | | style="background: #F5F5F5; padding: 5px; text-align: center;" | − | ||
| Line 176: | Line 192: | ||
* | * | ||
|- | |- | ||
| style="background: #DCDCDC; padding: 5px; text-align: center;" |[[Schwannoma]]<br | | style="background: #DCDCDC; padding: 5px; text-align: center;" |[[Schwannoma]]<br> | ||
| style="background: #F5F5F5; padding: 5px; text-align: center;" | − | | style="background: #F5F5F5; padding: 5px; text-align: center;" | − | ||
| style="background: #F5F5F5; padding: 5px; text-align: center;" | − | | style="background: #F5F5F5; padding: 5px; text-align: center;" | − | ||
| Line 198: | Line 214: | ||
* May be associated with [[Neurofibromatosis type II|NF-2]] (bilateral [[Schwannoma|schwannomas]]) | * May be associated with [[Neurofibromatosis type II|NF-2]] (bilateral [[Schwannoma|schwannomas]]) | ||
|- | |- | ||
| style="background: #DCDCDC; padding: 5px; text-align: center;" |[[Primary central nervous system lymphoma|Primary CNS lymphoma]]<br | | style="background: #DCDCDC; padding: 5px; text-align: center;" |[[Primary central nervous system lymphoma|Primary CNS lymphoma]]<br> | ||
| style="background: #F5F5F5; padding: 5px; text-align: center;" | + | | style="background: #F5F5F5; padding: 5px; text-align: center;" | + | ||
| style="background: #F5F5F5; padding: 5px; text-align: center;" | +/− | | style="background: #F5F5F5; padding: 5px; text-align: center;" | +/− | ||
| Line 222: | Line 238: | ||
! colspan="11" style="background: #7d7d7d; color: #FFFFFF; padding: 5px; text-align: center;" |Childhood primary brain tumors | ! colspan="11" style="background: #7d7d7d; color: #FFFFFF; padding: 5px; text-align: center;" |Childhood primary brain tumors | ||
|- | |- | ||
| style="background: #DCDCDC; padding: 5px; text-align: center;" |[[Pilocytic astrocytoma]]<br | | style="background: #DCDCDC; padding: 5px; text-align: center;" |[[Pilocytic astrocytoma]]<br> | ||
| style="background: #F5F5F5; padding: 5px; text-align: center;" | + | | style="background: #F5F5F5; padding: 5px; text-align: center;" | + | ||
| style="background: #F5F5F5; padding: 5px; text-align: center;" | +/− | | style="background: #F5F5F5; padding: 5px; text-align: center;" | +/− | ||
| Line 245: | Line 261: | ||
* Most of the time, [[Cerebellum|cerebellar]] dysfunction is the presenting [[signs]]. | * Most of the time, [[Cerebellum|cerebellar]] dysfunction is the presenting [[signs]]. | ||
|- | |- | ||
| style="background: #DCDCDC; padding: 5px; text-align: center;" |[[Medulloblastoma]]<br | | style="background: #DCDCDC; padding: 5px; text-align: center;" |[[Medulloblastoma]]<br> | ||
| style="background: #F5F5F5; padding: 5px; text-align: center;" | + | | style="background: #F5F5F5; padding: 5px; text-align: center;" | + | ||
| style="background: #F5F5F5; padding: 5px; text-align: center;" | +/− | | style="background: #F5F5F5; padding: 5px; text-align: center;" | +/− | ||
| Line 267: | Line 283: | ||
* [[Drop metastasis]] ([[metastasis]] through [[CSF]]) | * [[Drop metastasis]] ([[metastasis]] through [[CSF]]) | ||
|- | |- | ||
| style="background: #DCDCDC; padding: 5px; text-align: center;" |[[Ependymoma]]<br | | style="background: #DCDCDC; padding: 5px; text-align: center;" |[[Ependymoma]]<br><ref name=":0" /> | ||
| style="background: #F5F5F5; padding: 5px; text-align: center;" | + | | style="background: #F5F5F5; padding: 5px; text-align: center;" | + | ||
| style="background: #F5F5F5; padding: 5px; text-align: center;" | +/− | | style="background: #F5F5F5; padding: 5px; text-align: center;" | +/− | ||
| Line 290: | Line 306: | ||
* Causes an unusually persistent, continuous [[headache]] in children. | * Causes an unusually persistent, continuous [[headache]] in children. | ||
|- | |- | ||
| style="background: #DCDCDC; padding: 5px; text-align: center;" |[[Craniopharyngioma]]<br | | style="background: #DCDCDC; padding: 5px; text-align: center;" |[[Craniopharyngioma]]<br><ref name=":0" /> | ||
| style="background: #F5F5F5; padding: 5px; text-align: center;" | + | | style="background: #F5F5F5; padding: 5px; text-align: center;" | + | ||
| style="background: #F5F5F5; padding: 5px; text-align: center;" | +/− | | style="background: #F5F5F5; padding: 5px; text-align: center;" | +/− | ||
| Line 311: | Line 327: | ||
* Initialy presents with lower bitemporal quadrantanopsia followed by [[Bitemporal hemianopia|bitemporal hemianopsia]] (pressure on [[Optic chiasm|optic chiasma]] from above) | * Initialy presents with lower bitemporal quadrantanopsia followed by [[Bitemporal hemianopia|bitemporal hemianopsia]] (pressure on [[Optic chiasm|optic chiasma]] from above) | ||
|- | |- | ||
| style="background: #DCDCDC; padding: 5px; text-align: center;" |[[Pinealoma]]<br | | style="background: #DCDCDC; padding: 5px; text-align: center;" |[[Pinealoma]]<br> | ||
| style="background: #F5F5F5; padding: 5px; text-align: center;" | + | | style="background: #F5F5F5; padding: 5px; text-align: center;" | + | ||
| style="background: #F5F5F5; padding: 5px; text-align: center;" | +/− | | style="background: #F5F5F5; padding: 5px; text-align: center;" | +/− | ||
| Line 330: | Line 346: | ||
! colspan="11" style="background: #7d7d7d; color: #FFFFFF; padding: 5px; text-align: center;" |Vascular | ! colspan="11" style="background: #7d7d7d; color: #FFFFFF; padding: 5px; text-align: center;" |Vascular | ||
|- | |- | ||
| style="background: #DCDCDC; padding: 5px; text-align: center;" |[[Arteriovenous malformation|AV malformation]]<br | | style="background: #DCDCDC; padding: 5px; text-align: center;" |[[Arteriovenous malformation|AV malformation]]<br><ref name=":0" /> | ||
| style="background: #F5F5F5; padding: 5px; text-align: center;" | + | | style="background: #F5F5F5; padding: 5px; text-align: center;" | + | ||
| style="background: #F5F5F5; padding: 5px; text-align: center;" | + | | style="background: #F5F5F5; padding: 5px; text-align: center;" | + | ||
| Line 347: | Line 363: | ||
* We may see bag of worms appearance in [[CT angiography]] | * We may see bag of worms appearance in [[CT angiography]] | ||
|- | |- | ||
| style="background: #DCDCDC; padding: 5px; text-align: center;" |[[Brain aneurysm]]<br | | style="background: #DCDCDC; padding: 5px; text-align: center;" |[[Brain aneurysm]]<br> | ||
| style="background: #F5F5F5; padding: 5px; text-align: center;" | + | | style="background: #F5F5F5; padding: 5px; text-align: center;" | + | ||
| style="background: #F5F5F5; padding: 5px; text-align: center;" | +/− | | style="background: #F5F5F5; padding: 5px; text-align: center;" | +/− | ||
| Line 366: | Line 382: | ||
! colspan="11" style="background: #7d7d7d; color: #FFFFFF; padding: 5px; text-align: center;" |Infectious | ! colspan="11" style="background: #7d7d7d; color: #FFFFFF; padding: 5px; text-align: center;" |Infectious | ||
|- | |- | ||
| style="background: #DCDCDC; padding: 5px; text-align: center;" |Bacterial [[brain abscess]]<br | | style="background: #DCDCDC; padding: 5px; text-align: center;" |Bacterial [[brain abscess]]<br> | ||
| style="background: #F5F5F5; padding: 5px; text-align: center;" | + | | style="background: #F5F5F5; padding: 5px; text-align: center;" | + | ||
| style="background: #F5F5F5; padding: 5px; text-align: center;" | +/− | | style="background: #F5F5F5; padding: 5px; text-align: center;" | +/− | ||
| Line 386: | Line 402: | ||
* The most common causes of [[brain abscess]] are [[Streptococcus]] and [[Staphylococcus]]. | * The most common causes of [[brain abscess]] are [[Streptococcus]] and [[Staphylococcus]]. | ||
|- | |- | ||
| style="background: #DCDCDC; padding: 5px; text-align: center;" |[[Tuberculosis]]<br | | style="background: #DCDCDC; padding: 5px; text-align: center;" |[[Tuberculosis]]<br><ref name=":0" /> | ||
| style="background: #F5F5F5; padding: 5px; text-align: center;" | + | | style="background: #F5F5F5; padding: 5px; text-align: center;" | + | ||
| style="background: #F5F5F5; padding: 5px; text-align: center;" | +/− | | style="background: #F5F5F5; padding: 5px; text-align: center;" | +/− | ||
| Line 407: | Line 423: | ||
* It is associated with [[HIV]] [[infection]] | * It is associated with [[HIV]] [[infection]] | ||
|- | |- | ||
| style="background: #DCDCDC; padding: 5px; text-align: center;" |[[Toxoplasmosis]]<br | | style="background: #DCDCDC; padding: 5px; text-align: center;" |[[Toxoplasmosis]]<br> | ||
| style="background: #F5F5F5; padding: 5px; text-align: center;" | + | | style="background: #F5F5F5; padding: 5px; text-align: center;" | + | ||
| style="background: #F5F5F5; padding: 5px; text-align: center;" | +/− | | style="background: #F5F5F5; padding: 5px; text-align: center;" | +/− | ||
| Line 425: | Line 441: | ||
* It is associated with [[HIV]] [[infection]] | * It is associated with [[HIV]] [[infection]] | ||
|- | |- | ||
| style="background: #DCDCDC; padding: 5px; text-align: center;" |[[Hydatid cyst]]<br | | style="background: #DCDCDC; padding: 5px; text-align: center;" |[[Hydatid cyst]]<br><ref name=":0" /> | ||
| style="background: #F5F5F5; padding: 5px; text-align: center;" | + | | style="background: #F5F5F5; padding: 5px; text-align: center;" | + | ||
| style="background: #F5F5F5; padding: 5px; text-align: center;" | +/− | | style="background: #F5F5F5; padding: 5px; text-align: center;" | +/− | ||
| Line 443: | Line 459: | ||
* [[Brain]], [[eye]], and [[Spleen|splenic]] [[Cyst|cysts]] may not produce detectable amount of [[antibodies]] | * [[Brain]], [[eye]], and [[Spleen|splenic]] [[Cyst|cysts]] may not produce detectable amount of [[antibodies]] | ||
|- | |- | ||
| style="background: #DCDCDC; padding: 5px; text-align: center;" |[[CNS]] [[cryptococcosis]]<br | | style="background: #DCDCDC; padding: 5px; text-align: center;" |[[CNS]] [[cryptococcosis]]<br> | ||
| style="background: #F5F5F5; padding: 5px; text-align: center;" | + | | style="background: #F5F5F5; padding: 5px; text-align: center;" | + | ||
| style="background: #F5F5F5; padding: 5px; text-align: center;" | +/− | | style="background: #F5F5F5; padding: 5px; text-align: center;" | +/− | ||
| Line 472: | Line 488: | ||
* Since [[brain]] [[Biopsy|biopsies]] are highly invasive and may may cause [[neurological]] deficits, we [[diagnose]] [[CNS]] [[fungal]] [[Infection|infections]] based on [[laboratory]] and imaging findings | * Since [[brain]] [[Biopsy|biopsies]] are highly invasive and may may cause [[neurological]] deficits, we [[diagnose]] [[CNS]] [[fungal]] [[Infection|infections]] based on [[laboratory]] and imaging findings | ||
|- | |- | ||
| style="background: #DCDCDC; padding: 5px; text-align: center;" |[[CNS]] [[aspergillosis]]<br | | style="background: #DCDCDC; padding: 5px; text-align: center;" |[[CNS]] [[aspergillosis]]<br> | ||
| style="background: #F5F5F5; padding: 5px; text-align: center;" | + | | style="background: #F5F5F5; padding: 5px; text-align: center;" | + | ||
| style="background: #F5F5F5; padding: 5px; text-align: center;" | +/− | | style="background: #F5F5F5; padding: 5px; text-align: center;" | +/− | ||
| Line 498: | Line 514: | ||
! colspan="11" style="background: #7d7d7d; color: #FFFFFF; padding: 5px; text-align: center;" |Other | ! colspan="11" style="background: #7d7d7d; color: #FFFFFF; padding: 5px; text-align: center;" |Other | ||
|- | |- | ||
| style="background: #DCDCDC; padding: 5px; text-align: center;" |[[Brain metastasis]]<br | | style="background: #DCDCDC; padding: 5px; text-align: center;" |[[Brain metastasis]]<br><ref name=":0" /> | ||
| style="background: #F5F5F5; padding: 5px; text-align: center;" | + | | style="background: #F5F5F5; padding: 5px; text-align: center;" | + | ||
| style="background: #F5F5F5; padding: 5px; text-align: center;" | +/− | | style="background: #F5F5F5; padding: 5px; text-align: center;" | +/− | ||
| Line 526: | Line 542: | ||
[[CNS]]=[[Central nervous system]], AV=Arteriovenous, [[CSF]]=[[Cerebrospinal fluid]], [[NF-2]]=[[Neurofibromatosis type 2]], [[MEN1|MEN-1]]=[[Multiple endocrine neoplasia]], [[GFAP]]=[[Glial fibrillary acidic protein]], [[HIV]]=[[Human Immunodeficiency Virus|Human immunodeficiency virus]], BhCG=[[Human chorionic gonadotropin]], [[ESR]]=[[Erythrocyte sedimentation rate]], [[AFB]]=Acid fast bacilli, [[Magnetic resonance angiography|MRA]]=[[Magnetic resonance angiography]], [[CT angiography|CTA]]=[[CT angiography]] | [[CNS]]=[[Central nervous system]], AV=Arteriovenous, [[CSF]]=[[Cerebrospinal fluid]], [[NF-2]]=[[Neurofibromatosis type 2]], [[MEN1|MEN-1]]=[[Multiple endocrine neoplasia]], [[GFAP]]=[[Glial fibrillary acidic protein]], [[HIV]]=[[Human Immunodeficiency Virus|Human immunodeficiency virus]], BhCG=[[Human chorionic gonadotropin]], [[ESR]]=[[Erythrocyte sedimentation rate]], [[AFB]]=Acid fast bacilli, [[Magnetic resonance angiography|MRA]]=[[Magnetic resonance angiography]], [[CT angiography|CTA]]=[[CT angiography]] | ||
== References == | |||
[[fr:Tumeur du cerveau]] | [[fr:Tumeur du cerveau]] | ||
[[ja:脳腫瘍]] | [[ja:脳腫瘍]] | ||
| Line 538: | Line 552: | ||
{{WikiDoc Help Menu}} | {{WikiDoc Help Menu}} | ||
{{WikiDoc Sources}} | {{WikiDoc Sources}} | ||
<references /> | |||
[[Category:Disease]] | [[Category:Disease]] | ||
[[Category:Brain]] | [[Category:Brain]] | ||
[[Category:Oncology]] | [[Category:Oncology]] | ||
[[Category:Neurology]] | [[Category:Neurology]] | ||
[[Category:Up-To-Date]] | |||
[[Category:Medicine]] | [[Category:Medicine]] | ||
[[Category:Neurosurgery]] | [[Category:Neurosurgery]] | ||
Latest revision as of 20:41, 29 July 2020
| Brain tumor | |
 | |
|---|---|
| CT scan of brain showing brain cancer to left parietal lobe in the peri-ventricular area.https://en.wikipedia.org/wiki/File:Hirnmetastase_MRT-T1_KM.jpg |
|
Brain tumor Microchapters |
For patient information click here
Editor-In-Chief: C. Michael Gibson, M.S., M.D. [1] Assosciate editor(s)-In-Chief Fahimeh Shojaei, M.D., Prashanth Saddala, Sujit Routray, M.D. [2]
Synonyms and keywords: Brain tumour; brain cancer; intracranial tumor; astrocytoma; glioblastoma; oligodendrocytoma; meningioma; ependymoma; craniopharyngioma.
Overview
Classification
Brain tumors can be classified as follows:
| Brain tumors | |||||||||||||||||||||||||||||||||||||||||||||||||||
| Adult primary brain tumor | Childhood primary brain tumor | Brain metastase | |||||||||||||||||||||||||||||||||||||||||||||||||
•Glioblastoma multiforme •Oligodendroglioma •Meningioma •Hemangioblastoma •Pituitary adenoma •Schwannoma •Primary CNS lymphoma | •Pilocytic astrocytoma •Medulloblastoma •Ependymoma •Craniopharyngioma •Pinealoma | •Lung cancer •Breast cancer •Melanoma •Gastrointestinal tract cancer •Renal cell carcinoma •Osteosarcoma •Head and neck cancer •Neuroblastoma •Lymphoma •Prostate cancer | |||||||||||||||||||||||||||||||||||||||||||||||||
Causes
The exact cause of brain tumor is not known.
Differentiating Brain Tumor from other Diseases
On the basis of seizure, visual disturbance, and constitutional symptoms, brain tumors must be differentiated from AV malformation, brain aneurysm, bacterial brain abscess, tuberculosis, toxoplasmosis, hydatid cyst, CNS cryptococcosis, CNS aspergillosis, and brain metastasis.
| Diseases | Clinical manifestations | Para-clinical findings | Gold standard |
Additional findings | ||||||
|---|---|---|---|---|---|---|---|---|---|---|
| Symptoms | Physical examination | |||||||||
| Lab Findings | MRI | Immunohistopathology | ||||||||
| Head- ache |
Seizure | Visual disturbance | Constitutional | Focal neurological deficit | ||||||
| Adult primary brain tumors | ||||||||||
| Glioblastoma multiforme |
+ | +/− | +/− | − | + | − |
|
|
| |
| Oligodendroglioma |
+ | + | +/− | − | + | − |
|
|
| |
| Meningioma |
+ | +/− | +/− | − | + | − |
|
|
| |
| Hemangioblastoma |
+ | +/− | +/− | − | + | − |
|
| ||
| Pituitary adenoma [1] |
− | − | + Bitemporal hemianopia | − | − |
|
|
|
| |
| Schwannoma |
− | − | − | − | + | − |
|
|
| |
| Primary CNS lymphoma |
+ | +/− | +/− | − | + | − |
|
|
| |
| Childhood primary brain tumors | ||||||||||
| Pilocytic astrocytoma |
+ | +/− | +/− | − | + | − |
|
|
| |
| Medulloblastoma |
+ | +/− | +/− | − | + | − |
|
|
| |
| Ependymoma [1] |
+ | +/− | +/− | − | + | − |
|
|
| |
| Craniopharyngioma [1] |
+ | +/− | + Bitemporal hemianopia | − | + |
|
|
|
| |
| Pinealoma |
+ | +/− | +/− | − | + vertical gaze palsy |
|
|
|
| |
| Vascular | ||||||||||
| AV malformation [1] |
+ | + | +/− | − | +/− | − |
|
| ||
| Brain aneurysm |
+ | +/− | +/− | − | +/− | − |
|
|
|
|
| Infectious | ||||||||||
| Bacterial brain abscess |
+ | +/− | +/− | + | + |
|
|
|
|
|
| Tuberculosis [1] |
+ | +/− | +/− | + | + |
|
|
|
|
|
| Toxoplasmosis |
+ | +/− | +/− | − | + |
|
|
|
|
|
| Hydatid cyst [1] |
+ | +/− | +/− | +/− | + |
|
|
|
|
|
| CNS cryptococcosis |
+ | +/− | +/− | + | + |
|
|
|
|
|
| CNS aspergillosis |
+ | +/− | +/− | + | + |
|
|
|
|
|
| Other | ||||||||||
| Brain metastasis [1] |
+ | +/− | +/− | + | + | − |
|
|
|
|
ABBREVIATIONS
CNS=Central nervous system, AV=Arteriovenous, CSF=Cerebrospinal fluid, NF-2=Neurofibromatosis type 2, MEN-1=Multiple endocrine neoplasia, GFAP=Glial fibrillary acidic protein, HIV=Human immunodeficiency virus, BhCG=Human chorionic gonadotropin, ESR=Erythrocyte sedimentation rate, AFB=Acid fast bacilli, MRA=Magnetic resonance angiography, CTA=CT angiography