|
|
| (99 intermediate revisions by 12 users not shown) |
| Line 1: |
Line 1: |
| '''For patient information click [[{{PAGENAME}} (patient information)|here]] {{SI}}'''{Infobox_Disease |
| | __NOTOC__ |
| | {| class="infobox" style="float:right;" |
| | |- |
| | |[[File:Siren.gif|30px|link= Bradycardia resident survival guide]]||<br>||<br> |
| | |[[Bradycardia resident survival guide|'''Resident'''<br>'''Survival'''<br>'''Guide''']] |
| | |} |
| | {| class="infobox" style="float:right;" |
| | {{Infobox_Disease | |
| Name = Bradycardia | | | Name = Bradycardia | |
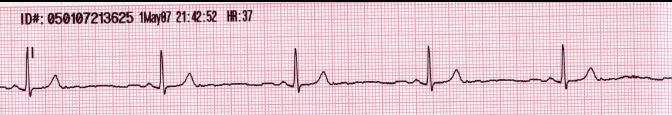
| Image = Lead II rhythm generated sinus bradycardia.JPG| | | Image = Lead II rhythm generated sinus bradycardia.JPG| |
| ICD10 = {{ICD10|R|00|1|r|00}} |
| |
| ICD9 = {{ICD9|427.81}}, {{ICD9|659.7}}, {{ICD9|785.9}}, {{ICD9|779.81}} |
| |
| }} | | }} |
| {{SI}} | | {{Bradycardia}} |
| {{WikiDoc Cardiology Network Infobox}}
| | {{CMG}}; {{AE}} {{MUT}} {{Ibtisam}} |
| {{CMG}} | |
| __NOTOC__
| |
| '''Associate Editor-In-Chief:''' {{MUT}}
| |
| | |
| {{Editor Help}}
| |
| | |
| ==Overview==
| |
| | |
| '''Bradycardia''', as applied to adult medicine, is defined as a resting [[heart rate]] of under 60 beats per minute, though it is seldom symptomatic until the rate drops below 50 beat/min. <ref name=SINUS-BRADYCARDIA>[http://www.emedicine.com/emerg/topic534.htm Sinus Bradycardia] eMedicine</ref> Trained athletes tend to have slow resting heart rates, and resting bradycardia in athletes should not be considered abnormal if the individual has no symptoms associated with it.
| |
| | |
| The term ''relative bradycardia'' is used to explain a heart rate that, while not technically below 60 beats per minute, is considered too slow for the individual's current medical condition.
| |
| | |
| This [[cardiac arrhythmia]] can be underlain by several causes, which are best divided into cardiac and non-cardiac causes.
| |
| Non-cardiac causes are usually secondary, and can involve [[recreational drug use|drug]] use or [[drug abuse|abuse]]; [[metabolism|metabolic]] or [[endocrine]] issues, especially in the [[thyroid]]; an [[electrolyte]] imbalance; [[:Category:Neurology|neurologic]] factors; autonomic reflexes; situational factors such as prolonged bed rest; and [[autoimmune|autoimmunity]].
| |
| Cardiac causes include acute or chronic [[ischemic heart disease]], vascular [[heart disease]], [[valvular heart disease]], or degenerative primary electrical disease.
| |
| Ultimately, the causes act by three mechanisms: depressed automaticity of the heart, conduction block, or escape pacemakers and rhythms.
| |
| | |
| == Causes ==
| |
| | |
| There are generally two types of problems that result in bradycardias: disorders of the [[sinus node]], and disorders of the [[atrioventricular node]] (AV node).
| |
| | |
| With sinus node dysfunction (sometimes called [[sick sinus syndrome]]), there may be disordered automaticity or impaired conduction of the impulse from the sinus node into the surrounding atrial tissue (an "exit block").
| |
| It is difficult and sometimes impossible to assign a mechanism to any particular bradycardia, but the underlying mechanism is not clinically relevant to treatment, which is the same in both cases of sick sinus syndrome: a permanent [[artificial pacemaker|pacemaker]].
| |
| | |
| Atrioventricular conduction disturbances (aka: AV block; [[First degree AV block|1<sup>o</sup> AV block]], [[Second degree AV block|2<sup>o</sup> type I AV block]], [[Second degree AV block|2<sup>o</sup> type II AV block]], [[Third degree AV block|3<sup>o</sup> AV block]]) may result from impaired conduction in the AV node, or anywhere below it, such as in the bundle of HIS.
| |
| | |
| Patients with bradycardia have likely acquired it, as opposed to having it [[congenital]]ly.
| |
| Bradycardia is more common in older patients.
| |
| | |
| <div align="left">
| |
| <gallery heights="175" widths="275">
| |
| Image:Lead II rhythm generated sinus bradycardia.JPG
| |
| </gallery>
| |
| </div>
| |
| | |
| ===Complete Differential Diagnosis of the Causes of Bradycardia===
| |
| | |
| (In alphabetical order)
| |
| {{MultiCol}} | |
| *[[Aceclidine]]
| |
| *[[Acepromazine]]
| |
| *[[Acetylcholinesterase inhibitor]]
| |
| *[[Adenosine]]
| |
| *[[Amiodarone]]
| |
| *[[Amodiaquine]]
| |
| *[[Anorexia Nervosa]]
| |
| *[[Apnea of prematurity]]
| |
| *[[Atenolol]]
| |
| *[[Atrioventricular Block]]
| |
| *[[Autonomic neuropathy]]
| |
| *[[Barbiturates]]
| |
| *[[Beta-blockers]]
| |
| *[[Brucellosis]]
| |
| *[[Bupivacaine]]
| |
| *[[Calcium channel blocker]]
| |
| *[[Cardiac arrhythmia]]
| |
| *[[Cardiac Dysrhythmias]]
| |
| *[[Cardiomegaly]]
| |
| *[[Catecholaminergic polymorphic ventricular tachycardia]]
| |
| *[[Cerebral Hemorrhage]]
| |
| *[[Cerebral venous sinus thrombosis]]
| |
| *[[Chagas' disease]]
| |
| *[[Clomipramine]]
| |
| *[[Colorado tick fever]]
| |
| *[[Congenital Long QT Syndrome]]
| |
| *[[Cushing reaction]]
| |
| *[[Cushing reflex]]
| |
| *[[Cushing's triad]]
| |
| *[[Detomidine]]
| |
| *[[Digitalis]]
| |
| *[[Diltiazem]]
| |
| *[[Diphenhydramine]]
| |
| *[[Donepezil]]
| |
| *[[Doxepin]]
| |
| *[[Drowning]]
| |
| *[[Emery-Dreifuss muscular dystrophy]]
| |
| *[[Enema]]
| |
| *[[Fetal distress]]
| |
| *[[Gamma-Hydroxybutyric acid]]
| |
| *[[Gastric lavage]]
| |
| *[[Glyceryl trinitrate ]]
| |
| *[[Grayanotoxin]]
| |
| *[[Hantavirus pulmonary syndrome]]
| |
| *[[Hellebore]]
| |
| *[[Holt-Oram syndrome]]
| |
| *[[Hydrocodone]]
| |
| *[[Hydroxyethyl starch]]
| |
| *[[Hypercalcemia]]
| |
| *[[Hyperkalemia]]
| |
| *[[Hypokalemia]]
| |
| *[[Hypothermia]]
| |
| *[[Hypothyroidism]]
| |
| *[[Ibuprofen]]
| |
| *[[Isosorbide dinitrate]]
| |
| *[[Ivabradine]]
| |
| *[[Legionella pneumonia and Mycoplasma pneumonia]]
| |
| *[[Levobetaxolol]]
| |
| *[[Levobupivacaine]]
| |
| *[[Lidocaine]]
| |
| {{ColBreak}} | |
| *[[Lithium]]
| |
| *[[Mammalian diving reflex]]
| |
| *[[Medetomidine]]
| |
| *[[Mefloquine]]
| |
| *[[Mepivacaine]]
| |
| *[[Methacholine]]
| |
| *[[Methoxamine]]
| |
| *[[Methyldopa]]
| |
| *[[Morphine]]
| |
| *[[Moxonidine]]
| |
| *[[Myxedema coma]]
| |
| *[[Nadolol]]
| |
| *[[Nalbuphine]]
| |
| *[[Nalmefene]]
| |
| *[[Neonatal lupus erythematosus]]
| |
| *[[Neostigmine]]
| |
| *[[Nesiritide]]
| |
| *[[Neurocardiogenic Syncope]]
| |
| *[[Neurogenic shock]]
| |
| *[[Norepinephrine]]
| |
| *[[Oculocardiac reflex]]
| |
| *[[Opioid]]
| |
| *[[Oxymorphone]]
| |
| *[[PCI Complications: Radiocontrast toxicity]]
| |
| *[[Phenobarbital]]
| |
| *[[Phenylephrine]]
| |
| *[[Phenytoin]]
| |
| *[[Pilocarpine]]
| |
| *[[Propafenone]]
| |
| *[[Propranolol]]
| |
| *[[Pulseless ventricular tachycardia]]
| |
| *[[Quinidine]]
| |
| *[[Raised Intracranial pressure]]
| |
| *[[Rapid sequence induction]]
| |
| *[[Reserpine]]
| |
| *[[Right Bundle Branch Block]]
| |
| *[[Ropivacaine]]
| |
| *[[Second Degree AV Block]]
| |
| *[[Sick sinus syndrome]]
| |
| *[[Sinoatrial Block]]
| |
| *[[Speedball (drug)]]
| |
| *[[ST Elevation Myocardial Infarction Complications]]
| |
| *[[Subarachnoid hemorrhage]]
| |
| *[[Sulpiride]]
| |
| *[[Suxamethonium chloride]]
| |
| *[[Tacrine]]
| |
| *[[Theobromine poisoning]]
| |
| *[[Timolol]]
| |
| *[[Trazodone]]
| |
| *[[Trypanosoma cruzi]]
| |
| *[[Tularaemia]]
| |
| *[[Typhoid fever]]
| |
| *[[Uncaria tomentosa]]
| |
| *[[Vagal episode]]
| |
| *[[Vasa previa]]
| |
| *[[Vasovagal syncope]]
| |
| *[[Vertebral subluxation]]
| |
| *[[Xylazine]]
| |
| {{EndMultiCol}} | |
| | |
| ===Complete Differential Diagnosis of the Causes of Bradycardia===
| |
| | |
| (By organ system)
| |
| | |
| {|style="width:70%; height:100px" border="1"
| |
| |style="height:100px"; style="width:25%" border="1" bgcolor="LightSteelBlue" | '''Cardiovascular'''
| |
| |style="height:100px"; style="width:75%" border="1" bgcolor="Beige" |
| |
| [[Atrioventricular Block]],
| |
| [[Cardiac arrhythmia]],
| |
| [[Cardiac Dysrhythmias]],
| |
| [[Cardiomegaly]],
| |
| [[Right Bundle Branch Block]],
| |
| [[Second Degree AV Block]],
| |
| [[ST Elevation Myocardial Infarction Complications]],
| |
| [[Sinoatrial Block]],
| |
| [[Pulseless ventricular tachycardia]],
| |
| [[Sick sinus syndrome]],
| |
| | |
|
| |
|
| |-
| | {{SK}} Abnormally slow heartbeat, slow heartbeat |
| |-bgcolor="LightSteelBlue"
| | ==[[Bradycardia overview|Overview]]== |
| | '''Chemical / poisoning'''
| |
| |bgcolor="Beige"| No underlying causes
| |
| |-
| |
| |-bgcolor="LightSteelBlue"
| |
| | '''Dermatologic'''
| |
| |bgcolor="Beige"| No underlying causes
| |
| |-
| |
| |-bgcolor="LightSteelBlue"
| |
| | '''Drug Side Effect'''
| |
| |bgcolor="Beige"|
| |
| [[Aceclidine]], | |
| [[Acepromazine]],
| |
| [[Acetylcholinesterase inhibitor]],
| |
| [[Adenosine]],
| |
| [[Amiodarone]],
| |
| [[Amodiaquine]],
| |
| [[Atenolol]],
| |
| [[Barbiturates]],
| |
| [[Beta-blockers]],
| |
| [[Bupivacaine]],
| |
| [[Calcium channel blocker]],
| |
| [[Clomipramine]],
| |
| [[Detomidine]],
| |
| [[Digitalis]],
| |
| [[Diltiazem]],
| |
| [[Diphenhydramine]],
| |
| [[Donepezil]],
| |
| [[Doxepin]],
| |
| [[Glyceryl trinitrate ]],
| |
| [[Hydrocodone]],
| |
| [[Ibuprofen]],
| |
| [[Isosorbide dinitrate]],
| |
| [[Ivabradine]],
| |
| [[Levobetaxolol]],
| |
| [[Levobupivacaine]],
| |
| [[Lidocaine]],
| |
| [[Lithium]],
| |
| [[Medetomidine]],
| |
| [[Mefloquine]],
| |
| [[Mepivacaine]],
| |
| [[Methacholine]],
| |
| [[Methoxamine]],
| |
| [[Methyldopa]],
| |
| [[Morphine]],
| |
| [[Moxonidine]],
| |
| [[Nadolol]],
| |
| [[Nalbuphine]],
| |
| [[Nalmefene]],
| |
| [[Opioid]],
| |
| [[Oxymorphone]],
| |
| [[Phenobarbital]],
| |
| [[Phenylephrine]],
| |
| [[Phenytoin]],
| |
| [[Pilocarpine]],
| |
| [[Propafenone]],
| |
| [[Propranolol]],
| |
| [[Quinidine]],
| |
| [[Reserpine]],
| |
| [[Ropivacaine]],
| |
| [[Sulpiride]],
| |
| [[Suxamethonium chloride]],
| |
| [[Tacrine]],
| |
| [[Timolol]],
| |
| [[Trazodone]],
| |
| [[Uncaria tomentosa]],
| |
| [[Xylazine]],
| |
|
| |
|
| |-
| | ==[[Bradycardia historical perspective|Historical Perspective]]== |
| |-bgcolor="LightSteelBlue"
| |
| | '''Ear Nose Throat'''
| |
| |bgcolor="Beige"| No underlying causes
| |
| |-
| |
| |-bgcolor="LightSteelBlue"
| |
| | '''Endocrine'''
| |
| |bgcolor="Beige"| [[Hypothyroidism]],
| |
|
| |
|
| |-
| | ==[[Bradycardia classification|Classification]]== |
| |-bgcolor="LightSteelBlue"
| |
| | '''Environmental'''
| |
| |bgcolor="Beige"|
| |
| [[Grayanotoxin]], | |
| [[Hellebore]],
| |
| [[Hypothermia]],
| |
|
| |
|
| | ==[[Bradycardia pathophysiology|Pathophysiology]]== |
| | ==[[Bradycardia causes|Causes]]== |
| | ==[[Bradycardia differential diagnosis|Differentiating Bradycardia from other Conditions]]== |
| | ==[[Bradycardia epidemiology and demographics|Epidemiology and Demographics]]== |
|
| |
|
| | | ==[[Bradycardia risk factors|Risk Factors]]== |
| |-
| | ==[[Bradycardia screening|Screening]]== |
| |-bgcolor="LightSteelBlue"
| | ==[[Bradycardia natural history, complications and prognosis|Natural History, Complications and Prognosis]]== |
| | '''Gastroenterologic'''
| | ==Diagnosis== |
| |bgcolor="Beige"| No underlying causes
| | [[Bradycardia history and symptoms|History and Symptoms]] | [[Bradycardia physical examination|Physical Examination]] | [[Bradycardia laboratory findings|Laboratory Findings]] | [[Bradycardia electrocardiogram|Electrocardiogram]] | [[Bradycardia chest x ray|Chest X Ray]] | [[Bradycardia CT|CT]] | [[Bradycardia echocardiography or ultrasound|Echocardiography]] | [[Bradycardia other diagnostic studies|Other Diagnostic Studies]] |
| |-
| |
| |-bgcolor="LightSteelBlue"
| |
| | '''Genetic'''
| |
| |bgcolor="Beige"|
| |
| [[Congenital Long QT Syndrome]], | |
| [[Catecholaminergic polymorphic ventricular tachycardia]],
| |
| [[Emery-Dreifuss muscular dystrophy]],
| |
| | |
|
| |
| |-
| |
| |-bgcolor="LightSteelBlue"
| |
| | '''Hematologic'''
| |
| |bgcolor="Beige"| No underlying causes
| |
| |-
| |
| |-bgcolor="LightSteelBlue"
| |
| | '''Iatrogenic'''
| |
| |bgcolor="Beige"|
| |
| [[Enema]], | |
| [[Gastric lavage]],
| |
| [[PCI Complications: Radiocontrast toxicity]],
| |
| [[Rapid sequence induction]],
| |
| | |
| | |
| | |
| |-
| |
| |-bgcolor="LightSteelBlue"
| |
| | '''Infectious Disease'''
| |
| |bgcolor="Beige"|
| |
| [[Chagas' disease]], | |
| [[Hantavirus pulmonary syndrome]],
| |
| [[Legionella pneumonia and Mycoplasma pneumonia]],
| |
| [[Tularaemia]],
| |
| [[Colorado tick fever]],
| |
| [[Brucellosis]],
| |
| [[Trypanosoma cruzi]],
| |
| [[Typhoid fever]],
| |
| | |
| | |
| | |
| | |
| |-
| |
| |-bgcolor="LightSteelBlue"
| |
| | '''Musculoskeletal / Ortho'''
| |
| |bgcolor="Beige"|
| |
| [[Holt-Oram syndrome]],
| |
| [[Vertebral subluxation]],
| |
| | |
| | |
| |-
| |
| |-bgcolor="LightSteelBlue"
| |
| | '''Neurologic'''
| |
| |bgcolor="Beige"|
| |
| [[Vasovagal syncope]],
| |
| [[Vagal episode]],
| |
| [[Neurogenic shock]],
| |
| Subarachanoid hemorrhage,
| |
| [[Raised Intracranial pressure]],
| |
| [[Autonomic neuropathy]],
| |
| [[Cerebral hemorrhage]],
| |
| [[Cerebral venous sinus thrombosis]],
| |
| Cushing triad,
| |
| [[Cushing reaction]],
| |
| [[Cushing reflex]],
| |
| [[Neurocardiogenic Syncope]],
| |
| | |
| | |
| | |
| | |
| | |
| |-
| |
| |-bgcolor="LightSteelBlue"
| |
| | '''Nutritional / Metabolic'''
| |
| |bgcolor="Beige"|
| |
| [[Hypercalcemia]], | |
| [[Hyperkalemia]], | |
| [[Hypokalemia]], | |
| [[Anorexia Nervosa]], | |
| | |
| | |
| |-
| |
| |-bgcolor="LightSteelBlue"
| |
| | '''Obstetric/Gynecologic'''
| |
| |bgcolor="Beige"|
| |
| [[Fetal distress]],
| |
| [[Neonatal lupus erythematosus]],
| |
| [[Vasa previa]],
| |
| | |
| | |
| | |
| |-
| |
| |-bgcolor="LightSteelBlue"
| |
| | '''Oncologic'''
| |
| |bgcolor="Beige"| No underlying causes
| |
| |-
| |
| |-bgcolor="LightSteelBlue"
| |
| | '''Opthalmologic'''
| |
| |bgcolor="Beige"| [[Oculocardiac reflex]],
| |
| | |
| |-
| |
| |-bgcolor="LightSteelBlue"
| |
| | '''Overdose / Toxicity'''
| |
| |bgcolor="Beige"|
| |
| [[Gamma-Hydroxybutyric acid]],
| |
| [[Hydroxyethyl starch]]
| |
| [[Speedball (drug)]],
| |
| [[Theobromine poisoning]],
| |
| | |
| |-
| |
| |-bgcolor="LightSteelBlue"
| |
| | '''Psychiatric'''
| |
| |bgcolor="Beige"| [[Anorexia Nervosa]],
| |
| | |
| |-
| |
| |-bgcolor="LightSteelBlue"
| |
| | '''Pulmonary'''
| |
| |bgcolor="Beige"| [[Apnea of prematurity]],
| |
| | |
| |- | |
| |-bgcolor="LightSteelBlue"
| |
| | '''Renal / Electrolyte'''
| |
| |bgcolor="Beige"| No underlying causes
| |
| |-
| |
| |-bgcolor="LightSteelBlue"
| |
| | '''Rheum / Immune / Allergy'''
| |
| |bgcolor="Beige"| No underlying causes
| |
| |-
| |
| |-bgcolor="LightSteelBlue"
| |
| | '''Sexual'''
| |
| |bgcolor="Beige"| No underlying causes
| |
| |-
| |
| |-bgcolor="LightSteelBlue"
| |
| | '''Trauma'''
| |
| |bgcolor="Beige"| No underlying causes
| |
| |-
| |
| |-bgcolor="LightSteelBlue"
| |
| | '''Urologic'''
| |
| |bgcolor="Beige"| No underlying causes
| |
| |-
| |
| |-bgcolor="LightSteelBlue"
| |
| | '''Miscellaneous'''
| |
| |bgcolor="Beige"|
| |
| [[Drowning]], | |
| [[Mammalian diving reflex]],
| |
| | |
| | |
| |-
| |
| |} | |
| | |
| == Management ==
| |
| There are two main reasons for treating any [[cardiac arrhythmia]]s.
| |
| With bradycardia, the first is to address the associated symptoms, such as [[Fatigue (physical)|fatigue]], limitations on how much an individual can physically exert, [[fainting]] (syncope), [[dizziness]] or lightheadedness, or other vague and non-specific symptoms.
| |
| The other reason to treat bradycardia is if the person's ultimate outcome (prognosis) will be changed or impacted by the bradycardia.
| |
| Treatment in this vein depends on whether any symptoms are present, and what the underlying cause is.
| |
| Primary or [[idiopathic]] bradycardia is treated symptomatically if it is significant, and the underlying cause is treated if the bradycardia is secondary.
| |
|
| |
|
| ==Treatment== | | ==Treatment== |
| | [[Bradycardia medical therapy|Medical Therapy]] | [[Bradycardia surgery|Surgery]] | [[Bradycardia primary prevention|Primary Prevention]] | [[Bradycardia secondary prevention|Secondary Prevention]] | [[Bradycardia cost-effectiveness of therapy|Cost-Effectiveness of Therapy]] | [[Bradycardia future or investigational therapies|Future or Investigational Therapies]] |
|
| |
|
| Drug treatment for bradycardia is typically not indicated for patients who are asymptomatic. In symptomatic patients, underlying electrolyte or acid-base disorders or hypoxia should be corrected first. IV [[atropine]] may provide temporary improvement in symptomatic patients, although its use should be balanced by an appreciation of the increase in myocardial oxygen demand this agent causes.
| | ==Case Studies== |
|
| |
|
| [[Atropine]] 0.5-1 mg IV or ET q3-5min up to 3 mg total (0.04 mg/kg) | | :[[Bradycardia case study one|Case #1]] |
|
| |
|
| ==See also== | | ==Related Chapter== |
| * [[Normal sinus rhythm]]
| |
| * [[Tachycardia]]
| |
| * [[Hypotension]]
| |
|
| |
|
| ==References==
| | *[[AV Block]] |
| {{reflist}}
| |
|
| |
|
| {{Symptoms and signs}} | | {{WikiDoc Help Menu}} |
| {{SIB}} | | {{WikiDoc Sources}} |
| | | [[CME Category::Cardiology]] |
| [[de:Bradykardie]]
| |
| [[es:Bradicardia]]
| |
| [[fr:Bradycardie]]
| |
| [[it:Bradicardia]]
| |
| [[nl:Bradycardie]]
| |
| [[nn:Bradykardi]]
| |
| [[pl:Bradykardia]]
| |
| [[pt:Bradicardia]]
| |
| [[ru:Брадикардия]]
| |
| [[sk:Bradykardia]] | |
| [[sv:Bradykardi]]
| |
|
| |
|
| [[Category:Cardiology]] | | [[Category:Cardiology]] |
| [[Category:Symptoms]] | | [[Category:Medical signs]] |
| | [[Category:Signs and symptoms]] |
| [[Category:Emergency medicine]] | | [[Category:Emergency medicine]] |
| | | [[Category:Arrhythmia]] |
| {{WikiDoc Help Menu}}
| | [[Category:Electrophysiology]] |
| {{WikiDoc Sources}}
| |